Mental Illness Fellowship Victoria. (n.d.). Factsheet – Understanding schizophrenia. http://www.mifellowship.org/sites/default/files/styles/Fact%20Sheets/UnderstandingSchizophrenia_001.pdf
Schizophrenia is a major mental illness affecting the normal functioning of the brain. It is characterised by psychotic symptoms and a diminished range of expressions of emotion.
The symptoms of schizophrenia are generally separated into the following categories:
Positive symptoms are experiences and behaviours that have been added to the person’s normal way of functioning
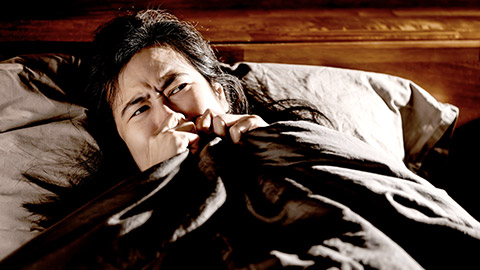
- Hallucinations are distortions of the senses that are very real to the person. The brain hears, sees, smells, tastes or feels things that are not there in the external world:
- Hearing voices
- Food tasting strange
- Seeing things that aren’t real
- Delusions are fixed and false beliefs – e.g. something outside of me is controlling my thoughts
- Disorganised speech
- Disorganised behaviour
Negative symptoms take away something from a person’s experience of the world. Negative symptoms are sometimes difficult to evaluate because they may be a result of a number of other factors such as a consequence of positive symptoms, medication side-effects and depression. The distinction requires sound clinical judgement
- Diminished range of emotional expressiveness (most of the time)
- Reduced speech (alogia)
- Inability to initiate and sustain goal-directed activities (avolition)
Cognitive symptoms
- Disorganised thinking
- Impaired executive function affecting:
- poor concentration and focus
- limited response to social cues
- difficulty prioritising and organising
These symptoms must be persistent for six months before a diagnosis of schizophrenia will be given.
How Common is Schizophrenia?
Widely accepted figures place the incidence of schizophrenia at about one in 100 people across all populations. Recent research challenges this and suggests that incidence may be significantly lower. It also shows that incidence is higher in males, in urban communities and among migrants.
The most common time of onset for males is between 18 and 25 years and for females between 25 years and mid-30s.
What Causes Schizophrenia?
No single cause has been identified but several factors are believed to contribute to the onset of schizophrenia in some people. Both the onset and the course of schizophrenia can be viewed in terms of stress-vulnerability. A variety of biological, psychological and social factors can influence vulnerability to the onset of psychosis and vulnerability to relapse (see over). It is recognised that stressful incidents often precede the onset of schizophrenia.
Insight into the Experience of Schizophrenia
Schizophrenia takes on many forms. It can show itself both cognitively (in the way a person is thinking), affectively (in a person’s mood) and in a person’s behaviour. The following chart looks at various behaviours that might manifest as a result of the positive and negative symptoms of schizophrenia and interventions that may be helpful.
| Positive symptoms | Associated behaviour Remember, these behaviours are out of keeping with the person’s normal value system | Helpful interventions |
|---|---|---|
| Delusions and hallucinations |
|
|
| Paranoia (a delusion) |
|
|
| Disordered thinking and behaviour |
|
|
| Negative symptoms |
Associated behaviour Remember, these behaviours are out of keeping with the person’s normal value system |
Helpful interventions |
| Affective (mood) flattening or a reduced range of emotional expression |
|
|
| Poverty of speech (alogia) |
|
|
| Inability to initiate and persist in goal-directed activities (avolition) |
|
|
Biological factors
- Family history (genetics) – A family history of psychosis and certain personality disorders are associated with an increased risk of vulnerability to schizophrenia.
- Physical abnormality of the brain – there is some evidence which suggests that people with schizophrenia have some alterations in brain shape (enlarged ventricles, smaller hippocampus).
- Chemical imbalance – there is some evidence to suggest that the chemical systems involving the neurotransmitters dopamine and glutamate are involved.
- Neurodevelopmental factors
Personal attributes
- Poor social and coping skills
- Poor communication skills
Environmental stress
Schizophrenia is not a stress-related illness, but stress can interact with other risk factors to trigger acute (psychotic) episodes of the illness. Stress-inducing activities and events include substance use, work/school problems, rejection by others, family conflicts, low social supports and major life events.
None of the risk factors are the cause of schizophrenia, but the vulnerability to schizophrenia (and relapse) increases for people with a number of risk factors present.
Protective factors
- Good coping skills
- Good social supports
- Medication
Advancements in medication are continually improving the outlook for people with schizophrenia. With psychological and social support, the majority can live full and active lives.
Keeping in mind the impacts of schizophrenia on those living with the illness, the treatment model takes into account the biological aspects of the illness (medication) and the psychological and social impacts, ie a biopsychosocial approach.
Treatment for acute episodes of schizophrenia will consider the safety of the person with the illness, their nutritional needs and the distress involved (both for the person and for the relatives). Therefore hospitalisation is considered at this time to treat the symptoms. Antipsychotic and tranquillising medications are commonly used in conjunction with medical support and the reduction of external stimulus.
Once the acute symptoms have subsided the psychosocial aspect of rehabilitation is encouraged. These types of services are important in helping people regain confidence and make friends and social connections which will reduce the morbidity caused by the illness (social isolation, poverty from unemployment, and loss of social skills).
In addition to the specific interventions previously mentioned, there are many things friends and family can do to help.
- Always remember that schizophrenia is a medical condition that requires medical treatment. Just as you cannot stop a person’s leg bleeding by talking to them, you cannot stop schizophrenia without medical intervention. Treatment is effective.
- The majority of people with schizophrenia are not violent. Where the symptoms for schizophrenia are active or where there is misuse of drugs or alcohol there may be an increase in violence. Engage safety first principles.
- Be aware of the possibility of other illnesses developing where the person with schizophrenia is using drugs. The rate of Hepatitis C infection amongst people with a mental illness is eleven times that found in the wider community. Seek advice if you have concerns.
- Find out as much about the illness as you can. Knowledge is power and gives you a much better chance of developing good coping strategies.
- Be patient. People experiencing schizophrenia need to come to some insight regarding their illness. This is not always easy and takes time.
- Know what to expect of the mental health system and be prepared to be assertive in seeking appropriate care.
- Link in with community organisations that offer supports and services that complement the mental health system. They often provide educational programs, counselling and local support groups.
- Remember to stay healthy yourself. Do not underestimate the impact of the illness on you. Schizophrenia often involves trauma and grief and has an impact on whole families. Be prepared to seek support to develop strategies that keep you well.
Ask an expert – receive answers to questions about schizophrenia from consultants and professionals: SFNSW
www.sfnsw.org.au/questions/discussion.htm
Mental Illness Fellowship Victoria
www.mifellowship.org
Mental Health Services Website (Vic)
www.health.vic.gov.au/mentalhealth
National Alliance of the Mentally Ill (NAMI) (USA)
www.nami.org
Mental Health Council of Australia
www.mhca.com.au
SANE Australia
www.sane.org
Beyond Blue
www.beyondblue.org.au
