Assessment Information
There are two assessments due in this module:
- 04A2 due at the end of Week 10.
- 02A1 due at the end of Week 23 (at the end of level 4)
04A2 is a written theory assessment.
Please note that 02A1 has practical components that you will have 10 weeks to complete. You should complete Task 1 of the assessment in Week 12 of this module, but you will continue working on Task 2 for 10 weeks after this. Please download the assessment immediately and read it thoroughly to plan your time.
When compounding in the dispensary, you will follow a formula. In this topic, we will review examples and give you opportunities to refresh your calculations and conversion skills.
Just below, we will show you an example of a standardised formula for preparing 40ml of Phenobarbital sodium solution 10 mg/ml.
Using the knowledge you already have, take a moment first and consider what features of a formula you would need to take note of when reviewing it. Write a list, then check it against ours by selecting the label or (+) sign. (Note: By connecting your new knowledge with what you already know, you are more likely to absorb it.)
Note the following features of the formula:
|
 |
| Up to: You will notice that the formula is a mixture of solids and liquids. When we have a preparation like this, the quantity of the vehicle will state up to. This means that we carefully add the vehicle to the other ingredients until the total quantity of the preparation equals the quantity prescribed. In our formula for Phenobarbital sodium solution, the vehicle is water. The quantity of water is ‘up to 40ml’. | |
When we have a preparation that has a formula made up of all liquids or a preparation made up of all solids, then we will calculate the quantity of the ingredients and the vehicle and then combine them together.
Time to see the formula! View and download the front and back of the New Zealand standardised oral formulation batch sheet (and find the key features of the formula that we listed above).
Let’s look at another example:
You receive a prescription for 75ml of Wart Paint. The formula for Wart Cream is as follows:
| Wart Paint | |
|---|---|
| Ingredient | Amount |
| Lactic Acid | 32ml |
| Salicylic Acid | 32g |
| Collodion Flex | To 100ml |
We can see that there is a mixture of liquid (Lactic Acid) and solid (Salicylic Acid) ingredients in a liquid vehicle (Collodian Flex).
To make the Wart Paint, we need to know how much of each ingredient we need to measure out to make the total amount stated in the prescription.
The following is one calculation method you could use:
1. Lactic Acid
32ml divided by 100ml of Wart Paint, multiplied by 75g (the total quantity we want).
2. Salicylic Acid
32g divided by 100ml of Wart Paint, multiplied by 75g (the total quantity we want).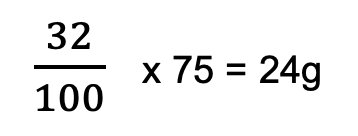
3. Collodion Flex
Once the salicylic acid has been dissolved in the lactic acid, we would then add enough collodion flex to make the total quantity of the preparation up to 75ml.
Your turn!
Now, it's time to work out some calculations on your own. As we often learn best by doing, download this worksheet and complete the calculations for each question. Once you've completed it or given it your best go, click the label or (+) button to download the answers (and compare them to your own).
Here is an example of a formula for a preparation where the formula contains all solids. We want to calculate the quantities required to make up 35g of Zee Cream.
| Zee Cream | |
|---|---|
| Ingredient | Amount |
| Solid X | 0.3g |
| Solid Y | 0.12g |
| Base | To 4g |
Your calculations for the Zee Cream will include finding the quantity of the Base. One method you can use is as follows:
Total Quantity required minus Quantity of Solid X minus Quantity of Solid Y = Quantity of Base
35g – Quantity Solid X (g) – Quantity Solid Y (g) = Quantity Base (g)
Look at the table and activity below. Using your preferred method of working, complete the activity.
| Zee Cream | ||
|---|---|---|
| Ingredient | Amount | Answer |
| Solid X | 0.3g | [A] |
| Solid Y | 0.12g | [B] |
| Base | To 4g | [C] |
As a pharmacy technician, you may be asked to prepare a preparation that involves a percentage. Consider the following:
Scenario:
Ivy has been to her doctor about a skin condition. Her doctor tells her the skin condition is eczema and has prescribed a cream to treat it. Ivy comes to your pharmacy and hands you her prescription. The doctor has prescribed 2% Hydrocortisone powder in Fatty cream (Mitte: 250 grams).
To prepare this cream for Ivy, you will need to calculate how many grams of Hydrocortisone powder you will need and how much of the fatty cream.
Take a moment now to think about what you already know about percentages so you can help Ivy.
Hydrocortisone 2%
Percent means parts per hundred. Therefore, our calculation would be: 2 divided by 100, multiplied by 250g (quantity of the final preparation).
To calculate the amount of fatty cream, we would need to do the following:
Weight of final prepared cream - weight of hydrocortisone powder (Ag) = amount of fatty cream needed.
Kei a koe te rākau ināianei, it's your turn now!
Over time, with practice in the workplace, you will become confident in these types of calculations.
If you are struggling with this topic, don’t forget your tutor is here to support you, and it is up to you to reach out. They will gladly assist you to develop your skills and knowledge.
Self-directed learning activities:
In today’s SDL activities, we will be looking at other types of calculations that involve percentages. Complete the following 9 questions.
Ka pai - great work! You finished another week of Professional Practice Part 1. It may have felt challenging for you, so good on you for getting to this point.

Step 7. Selecting Medicine
![]()
In this step, you are selecting the correct medicine to dispense from stock.
Using the original prescription, you will be checking the stock for the following:
- The medicine name and dosage form
- The strength
- The quantity
- The expiry date.
Generic vs Brand
As you may know, every medicine has two names. These are:
| The generic name | This name comes from the medicine's active ingredient. The active ingredient is the component of a medication that produces the intended therapeutic effect. Generic names are not typically capitalised. |
| The brand name | Often referred to as the ‘trade name’, it's the name given to a medicine by the pharmaceutical company that manufactures it. These names are typically catchy and easy to remember, and they are used for marketing purposes to help distinguish one product from another. Brand names are usually capitalised. |
|
Example: A generic drug, one used for hypertension, is metoprolol, whereas a brand name for the same drug is Betaloc. |
|
|
|
|
- Read the Pharmac pamphlet about generic medicines and complete the activity below.
Step 8. Assembling
After selecting the medicine from the stock, you will need to gather and assemble all the items needed. In some cases, this may involve the tasks of counting out or measuring medicines from stock and putting them into the appropriate containers for dispensing. We will now take a closer look at how best to carry out these tasks.
| Section 5 of the Health and Disability Services Pharmacy Service Standards discusses the expected standards for the tasks of dispensing and repackaging medicines. The standards can be used by pharmacies to develop their own Standard Operating Procedures (SOPs) for these tasks. |  |
Work area
Read through the following key points about the work area for assembling medicines for dispensing:
- The work areas should be designated areas that are separate from sales and customer areas. The public and unauthorised staff should not have access. This ensures that patients' health information is kept private and ensures the health and safety of those working, and the products. It also minimises the risk of theft from the dispensary.
- The layout should enable a logical workflow and be away from the workflow of others to prevent distractions and hazards such as bumps, trips, or falls.
- The area should be orderly and uncluttered, and only the equipment needed for dispensing should be present.
- All equipment used is clean, dry, and easily accessed when needed.
- All equipment is in working order and only used for the purpose intended.
- The walls, floors, and surfaces are properly constructed, maintained, and easily cleaned so that a clean and hygienic space can be maintained at all times.
- Preparation surfaces such as benches should be smooth, impervious, and washable to ensure hygiene is maintained and risks of contamination are minimised.
- Products in the area are protected from contamination from dust, dirt debris and cross-contamination from other products.
- The area is protected from insects and animals entering.
- The temperature, humidity and light are properly controlled for carrying out work and to protect products.
Dispensing equipment

One piece of equipment you may use when dispensing tablets or capsules from stock bottles is a pill counting tray and spatula similar to the one in this picture. It is important that the tray is cleaned and dried between each use to avoid cross-contamination between medicines and that no dirt or unwanted substances are transferred into the dispensing container.
Accuracy when counting out tablets or capsules is essential. Too few tablets and the customer will not get the full course of treatment required, and too many and they may get confused and take more than what is prescribed.
Strategies to ensure you count and dispense the correct amount from stock include:
- Carry out the process in the designated area so you won’t be disturbed, distracted, or physically bumped during the process
- Ensure the area is well-lit so you can see clearly
- Ensure the pill counter and spatula are in functioning order
- Have all the equipment needed before you start the process, including the prescription, so you don’t need to leave to collect anything during the count
- Check the prescription before the count
- Complete one task or prescription item at a time so you don’t mix up the medicines or the count
- Focus on what you are doing
Watch: Pill Counting Tray Procedure (1:51 minutes)
For a brief look at how a pill counting tray is used, watch this clip.
Accuracy in counting applies to all dispensing actions, including measuring out liquids and counting out strip or blister packaging from stock.
Repackaging and safety containers
During the assembling stage of dispensing, you may be required to repackage medicines from stock into containers and packages for dispensing to the customer. It is important you choose the appropriate containers for each medicine.
Factors to consider when repacking are:
The legal requirements under the New Zealand law for containers and repackaging. These can be found in the Medicines Act 1981, section 44 details the rules for containers and packages of medicines and Medicines Regulations 1984, section 37 (4 & 5).
Certain medications require special containers, such as glass or amber-coloured plastic, to prevent light from affecting the medicine.
Different containers are required for each dosage form, such as bottles for liquids.
Proper labelling is essential to ensure that the medication is administered correctly. The container must be large enough to accommodate the required labelling, including the name of the medication, strength, dosage, and patient information.
Certain medications require special handling and storage conditions, such as refrigeration, and the container must be able to maintain the appropriate temperature and prevent exposure to light or air.
The container must be safe for the patient, particularly for children or elderly patients. Some medications require child-resistant packaging, and it is important to ensure that the container meets these requirements.
Read the sections of the Medicines Act and Medicines Regulations noted above and answer the following questions.

Safety containers, sometimes referred to as child-resistant packaging, is packaging used to reduce the risk of children opening a medicine container and swallowing the medication inside.
Read about Child-Resistant Closures at the National Poisons Centre to learn more about safety containers.
Then, answer these questions.
⚠ The following are examples of potentially dangerous medications:
- Paracetamol
- Salicylates/NSAIDs
- Anticonvulsants
- Thyroxine
- Antidepressants
- Narcotics
- Beta-2-agonists
- Benzodiazepines
- Theophylline
- Iron salts
- Digoxin
- Cardiac drugs
- Phenothiazines, including sedating antihistamines.
Although this is a list of potentially dangerous medications, all accidental ingestion of medicine can be dangerous and require urgent medical attention.
Container types
There are a variety of containers and packaging to choose from:
 |
 |
 |
One of the aims when selecting the appropriate containers for different medications is to make a clear distinction between medicines that are to be taken internally and those extended for external use.
Read through the following tables for examples.
1. Internal medicines
| Preparation | Container |
|---|---|
| Mixtures | Plain, amber, glass or plastic, mission bottle or tablet vials |
| Emulsions (Internal) | Plain, amber, glass or plastic medicine bottle with a wide neck, if available |
| Elixirs | Plain, amber, glass or plastic mission bottle or tablet vials |
| Linctuses | Plain, amber, glass or plastic mission bottle or tablet vials |
| Tablets and capsules | Plain, amber, glass, plastic vial, tablet bottle or skillet |
| Powders | Individually wrapped in powder papers and dispensed in a skillet |
2. Substances for topical application
| Preparation | Container |
|---|---|
| Eye drops, ear drops, nasal drops | Dropper bottle |
| Mouthwashes and gargles | Clear ribbed bottle, glass or plastic, or, amber if contents sensitive to light |
| Enemas | Ribbed potion bottle, amber, glass or plastic |
| Lotions, liniments and antiseptics | Ribbed potion bottle, amber or clear, glass or plastic |
| Creams, ointments, pastes and gels | Ointment jars or tubes |
| Suppositories and pessaries | Individually wrapped in foil plastic and dispensed in a skillet |
After you have dispensed medicines from stock, leave the stock next to the dispensed medicines, ready for the final check. This means that the pharmacist can easily check to stock bottles you have used.
At this stage, you will also be gathering any medicine documentation, patient information or counselling aids that you will need when the patient collects their prescription.
Step 9: Attaching the label

Attaching the label may seem like a simple and obvious step in the dispensing process, but it is an important step to carry out correctly.
As you know, medicine labels play a crucial role in ensuring that patients receive the right medication at the right dosage and at the right time. The medication label provides essential information that customers need to know about their medication, such as the:
- drug name
- strength
- dosage instructions
- expiration date
- warnings about potential side effects.
Once the label has been printed, it needs to be attached to the medicine in such a way that this essential information can be easily read.
![[ADD IMAGE'S ALT TEXT]](/sites/default/files/Medicine%20Labels.png)
Guidelines for attaching the label
- Ensure that you attach the correct label to the correct medicine. This a very important check to avoid a very serious error!
- The container or package should be clean and dry so the label will stick and not fall off.
- The label needs to be straight and visibly balanced so the customer can easily see where it is and can read it easily.
- The label should be smoothly attached so there are no rips, folds, or wrinkles that would make it difficult to read.
- The label should be placed where it is not likely to be damaged or removed when the container is in use.
- The label should be placed where important information on the container is not covered up.
- The label is not overlapping on itself, covering up the writing and making it difficult to read.
- If the medicine container is inside another package, the label should be attached to the medicine container. This is known as the primary container.
- When attaching the label, ensure it is firmly stuck down to the container so it will not fall off during use.
| Part of your job as a pharmacy technician is to ensure that medication labels are correctly and securely attached to each medication before dispensing it to a customer. If the label is missing, incorrect, or poorly placed, it can result in serious consequences for the patient, including overdose, underdose, or other adverse drug reactions. |  |
Self-directed learning activities:
Next week, we will look at the last two steps in the dispensing process. Therefore, now is a good opportunity to spend some time reviewing the dispensing process so far.
You might like to:
- review the previous online content
- go over your personal notes
- consider if you have any questions or want to know more about any parts of the process (and then find the information you need!).
Congratulations. The learning for this week's Introduction to Dispensing is complete. Ka pai!
Colds and flu
Let's get started by reviewing your previous knowledge of coughs, colds and flu with this quiz.
The table below provides a summary of the key characteristics of cold and flu. Review the characteristics and take extra note of any that you weren't aware of.
| Characteristics | Cold | Flu |
|---|---|---|
| Season | All year round | May - September |
| Onset of symptoms | Build over 48 hours | Sudden, builds over hours |
| Duration of symptoms | 3 - 10 days | 7 - 14 days or longer |
| Sneezing | Usual | Sometimes |
| Cough | Common-productive | Common-dry |
| Sore throat | Usual | Sometimes |
| Fever | Rare or mild only | Usually high, above 38°C |
| Nasal congestion | Usual | Sometimes |
| Fatigue and weakness | Mild, 2-3 days | Can last 2-3 weeks |
| Extreme exhaustion | Absent | Common |
| Headache | Uncommon or mild | Severe |
| Muscular aches and pains | Uncommon or mild | Usual, often severe |
Colds and flu: treatment & advice
Treatment and advice for colds and flu focus on alleviating the symptoms and self-care to support recovery. Before we take a look at some of the common symptoms and the appropriate treatment and advice, we will review when to refer to a pharmacist
⚠WHEN TO REFER TO THE PHARMACIST
Colds:
- High temperature, body chills, joint aches, or pains
- Feel extremely unwell
- Earache or facial/sinus pain.
Flu:
- Symptoms include a stiff neck or rash
- Confusion
- Difficulty breathing
- Skin discolouration
- Diarrhoea or vomiting
- Problems eating and drinking
- Fever lasting more than a few days
- Have recently been overseas
- Symptoms worsen or persist longer than a week.
Cough
A cough can be a feature of both colds and flu. A cough is an important reflex to protect the airways and lungs. Coughing clears the airways of mucus, phlegm, a foreign body or other irritants or blockages.
Coughs can be divided into two types:
- Productive cough
- Also known as a ‘wet’ or ‘chesty’ cough
- Produces mucus or phlegm
- Often associated with a cold.
- Non-productive cough
- Also known as a ‘dry’ cough
- Does not produce mucus or phlegm
- Often associated with the flu.
Knowing what type of cough your customer has means that you can provide the appropriate treatment and advice. Coughs can be treated using products that can be divided into the following categories based on the effect they have:
- Cough suppressants
- Cough expectorants
- Mucolytics
- Combination.
To learn about these products, complete the activity below (make sure to click the 'Turn' button to see more).
Carry out your own research into how to alleviate a cough caused by a cold or flu. List your findings in your journal.
⚠ COUGH: WHEN TO REFER TO THE PHARMACIST
With any of these other symptoms of concern:
- Breathing difficulties
- Chest pain
- High fever
- Severe headache
- Rash
- Weight loss for no reason
- Coughing up blood or pink-tinged mucus
- Cough that only occurs at night
- Cough that has lasted longer than ten days or goes away for a period of time only to reoccur
- Customer who smokes
- Has allergies to medicines.
Sore throats
The sore throats caused by colds can be treated with a number of products.
These may be:
- non-medicated lozenges
- antiseptic/antibacterial lozenges
- lozenges or spray with locally acting anaesthetic
- lozenges with locally acting NSAIDs
- analgesics.
⚠ SORE THROAT: WHEN TO REFER TO THE PHARMACIST
- Children and adolescents reporting a particularly sore throat
- Swallowing is difficult, and preventing drinking fluids
- Showing signs of dehydration
- Severe sore throat, signs of pus or ulceration, white patches on tonsils
- Sore throats not related to a cold
- Persisted for several weeks or reoccurs
- With symptoms of rash, fever, vomiting, ear pain, breathlessness or general fatigue.
Nasal congestion
Nasal congestion or a ‘stuffy nose’ resulting from colds and flu can be treated with both pharmacy and self-care treatments.
Read this article about nasal decongestants and make your own notes on the side effects.
To review and take a further look at cold and flu treatments, watch this video from Abraham the Pharmacist. This clip covers the following cold and flu topics and will help you with the next learning activity.
- Signs and symptoms
- Sore throat and cough treatment
- Blocked nose, mucus or phlegm
- Headache and fever
- When to seek medical advice.
Coughs and cold in children: treatment & advice
All cough and cold medicines are contraindicated in children under six years of age. This means they should not be given them. There is no evidence to support that they are effective in this age group, and they can cause serious adverse reactions such as:
- convulsions
- increased heart rate
- decreased level of consciousness
- allergic reactions
- abnormal heart rhythms
- hallucinations.
Treatment and advice for children under six are:
- rest
- provide plenty of fluids to drink
- appropriate doses of paracetamol or ibuprofen for babies over three months old
- children over 12 months old can be given honey drinks or use saline nose drops
- children over two years old can use vapour rubs.
Children between six and twelve years can use cough and cold medicines sold in pharmacies but may require pharmacist advice before being sold.

⚠ Aspirin should NEVER be given to children under the age of 16 unless on the advice of a doctor. This is due to the risk of the child developing a condition called Reyes Syndrome. It is a rare but serious condition that causes confusion, swelling in the brain and liver damage.
Read the following scenario between a pharmacy technician and a customer, and answer the questions during the story.

Scenario:
Diana is in her early 20s. She looks tired and distressed. You noticed she has been sniffing a lot, and she keeps massaging her temples.
Diana: Hi, I don't feel very well. I’ve had colds before but nothing like this! I’m not sure what’s wrong with me. I have a headache, and I feel hot, but sometimes I shiver, it’s really freaky. I think I might have something serious.
My sister reckons I have a cold, but my boyfriend said it could be the flu. I don’t know. All I know is I was feeling fine the day before yesterday, and now I can't get rid of this headache, and my leg muscles ache. My nose is stuffed up too. What do you think I have?
I haven't taken anything for this yet, I didn’t know what to take. I don’t have any allergies, and I’m not on any medication. Usually, I’m really fit and healthy. I don’t have any health conditions. I’ve only been sick with this for two days. What should I take to help me feel better?
Activity
Using your previous experience and what you've learned in this topic, reflect on the following two points and write your responses in your notes.
- Explain the OTC products and self-care advice you would provide for this customer.
- Explain when Diana should seek further medical attention for her health condition.
Well done! You have completed another week of Introduction to Patient Care!


