In this topic, we focus on the names, structure, function and classification of joints within the skeletal system. You will learn:
- joint structure and function
- joint nomenclature (naming system)
- different joint types and classifications
- common joint conditions
- exercise and joint considerations.
Terminology and vocabulary reference guide
As an allied health professional, you need to be familiar with terms associated with basic exercise principles and use the terms correctly (and confidently) with clients, your colleagues, and other allied health professionals. You will be introduced to many terms and definitions. Add any unfamiliar terms to your own vocabulary reference guide.
Activities
There are activities throughout the topic and an end of topic automated quiz. These are not part of your assessment but will provide practical experience that will help you in your work and help you prepare for your formal assessment.
Joints or 'articulations' are formed at the point where two bones meet. They are the connection between bones in the body and which link the skeletal system as a functional whole system.
Thankfully, nature has our backs and has placed connective tissues amid our skeletal systems! This enables the union of bones via the joint or articulation structures and connective tissue structures to hold the bones of our skeletal system together (structure) whilst permitting some degree of movement (function). When it is said that one bone 'articulates' with another, it implies that the bone forms a joint. Examples are shown in the following illustrations.
Without joints, our skeleton would be a rigid deck structure unable to move. Have you ever been unfortunate enough to find yourself with a limb in a cast? If so, you can attest to how this limited the functional movement.
Let's recap. A joint is a point of contact:
- between two bones
- between bone and cartilage
- between bone and teeth.
So, what joints do and how draws on our understanding of basic anatomical terminology and the fundamental principles of anatomy and physiology.
Structure mirrors function
You will hear the phrase 'structure mirrors function' a lot in your studies. This phrase helps explain why our insides and outsides 'look how they look and do what they do'! Let's begin by looking at the functions of a joint.
Functions of a joint
Joints have two main functions:
- Joints hold the skeleton together.
- Joints give the skeleton mobility.
Here we see the first union of two body systems (the skeletal system and the muscular system) performing their own role and working together. Together, these two systems are referred to as the musculoskeletal system. In this topic we focus on the skeletal system, particularly the joints and how and why they do what they do (or don't do).
Welcome to the next level of your new language of anatomy and physiology! Have your personalised terminology and vocabulary reference guide handy!
Before we begin, let's define 'nomenclature'. Nomenclature is a system of names or terms, or the rules for forming these terms in a particular field of arts or sciences. In this case, anatomy and physiology.
Within this branch of science, you will meet terms in both Latin and Greek as well as English. This can feel overwhelming. However, if we take the term back to its grassroots we can avoid this feeling. So, when you find a word that looks borderline intimidating stop, break the term up into smaller words, and as if by magic, they begin to look familiar.
Typically, the scientific joint names are derived from the names of the bones involved. By identifying even half of a word like 'sternoclavicular joint' we begin to gather information such as location, function, where the structure starts and stops, or how the structure performs its function.
With practice, you will soon be able to easily 'translate' these names. This will support and enhance your understanding of anatomy and physiology, and also develop safe and effective exercise prescriptions. When this knowledge is combined with knowledge of muscle tissue, structure, and function, you will have a solid understanding of:
- where muscles and bones are located in the human body
- which muscles are in a specific area
- what bones are involved
- which joints are present
- how these all work together to provide particular movements.
Becoming comfortable with this level of detail, which will take time and practice, will see your program design and rationale soar. You will also find your skills and reputation as a fitness industry representative grow. This will provide huge value to your reputation and that of your business and set yourself apart from your colleagues.
The science behind joint names
The scientific joint names are derived from the names of the bones involved. Joint names can be 'translated' similarly to the examples that follow.
Sternoclavicular joint
The sternoclavicular is where the clavicle meets the sternum (sterno-sternum, clavicular- clavicle).
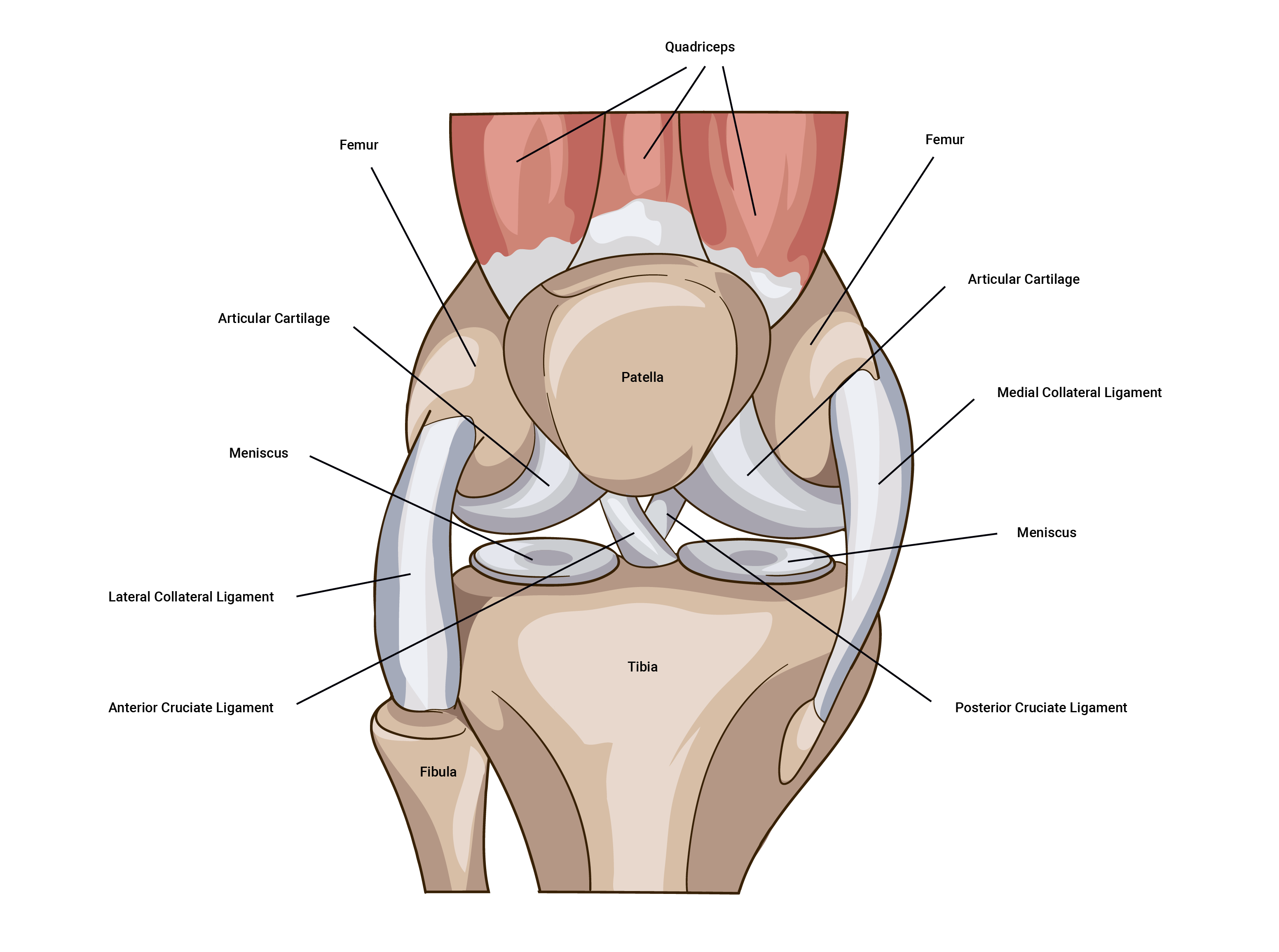
Tibiofemoral joint
The tibiofemoral joint is where the femur meets the tibia. In this situation, the joint (synovial) is made complete by the patella (knee cap). Note, the patella completes the knee structure and is not classified as a component of a synovial joint.
Glenohumeral joint
The glenohumeral joint is where the humerus meets the glenoid cavity of the shoulder.
Of course, there are more common names for the key joints of the body:
Shoulder region
Humero-scapular joint (involving the humorous and the scapula)
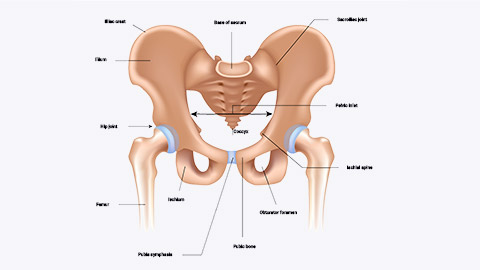
Hip
Iliofemoral Joint (involving the ileum and the femur)
Knuckles
Metacarpophalangeal (involving the metacarpal bones and the phalangeal bones)
Elbow
Humeroulnar joint (involving the humerus and the ulna)
Ankle
Talocrural joint (involving the tibia, fibula and the talus (heel bone))
Being able to understand these and adapt your language around these (that is, comfortably changing between 'street names' and medical terminology) will enhance your skills and knowledge. It will also support your reputation and the level of comfort clients have when working with you.
The skeletal system contains different classifications of joints based on two characteristics:
- Their structural composition (anatomical characteristics)
- Their function (degree of movement) to the skeletal system.
The phrase 'structure mirrors function' is worth repeating.
Structural classification of joints
The structural classification of joints is based on the presence or absence of a synovial cavity and the type of connective tissue they are composed of.
There are four main joint types (based on their structure):
- fibrous joints
- synostosis joints
- synovial joints
- cartilaginous joints.
Let's look at each of these in more detail. We will identify the structure and give an example of each type of joint.
Fibrous joints
Structure
There is no synovial cavity. Bones are held very closely together by dense irregular connective tissue that is rich in collagen fibres. Functionally classified as synarthrosis (immovable). Refer to the functional classification of joints in the following table.
Example
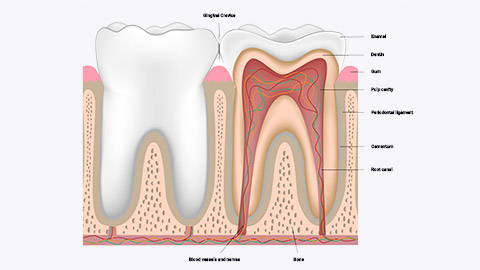
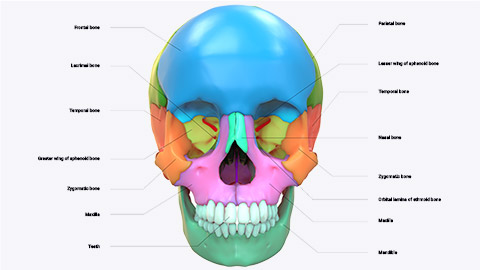
The joints which hold the teeth in their sockets and joints holding the bones of the skull together.
Synostosis joints
Structure
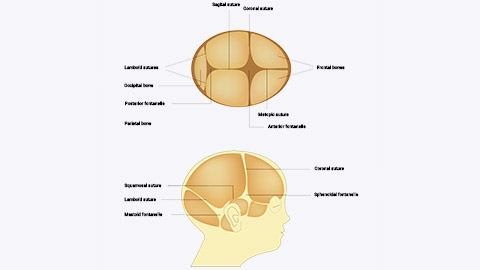
There is no synovial cavity. Fused sutures have calcified and now present as bone tissue. As a person's development continues into adulthood, some sutures are replaced by bone. When this occurs, this is no longer referred to as a suture but a suture that is now a synostosis, where two bones have completely fused into one. Refer to the functional classification of joints in the following table.
Example
The frontal bone of the skull (forehead bone) begins in two parts, however by the age of six, this is usually totally fused. This was previously a suture and now classified as synostosis which is totally immobile. Functionally classified as synarthrosis (immovable).
Synovial joints
Structure
A synovial joint does have a synovial cavity between the articulating bones. The synovial cavity is filled with synovial fluid with the articular bones connected by an articular capsule which is composed of dense irregular connective tissue and accessory ligaments. The synovial fluid allows smooth, frictionless movement, provides nutrients, and removes wastes. A synovial cavity allows significant movement of the joint. It also contains hyaline cartilage known as articular cartilage which provides shock absorption and reduces friction. It is functionally classified as freely moveable, diarthrosis. Refer to the functional classification of joints in the following table.
Example
Examples include the ball and socket joint of the hip, the hinge joint of the elbow, other pivot joints located between C1 and C2 in the vertebral column, and the saddle joint of the wrist.
Cartilaginous joints
Structure
Cartilaginous joints contain no synovial cavity. The articulating bones are joined by cartilage (hyaline or fibrocartilage). They provide more movement than fibrous joints but less than synovial joints.
Example
The joints between the vertebra of the spine, and the join in the pubic symphysis, or between the ribs and the sternum (breast bone) (represented in blue in the following image).

Functional classification of joints
This is the second joint classification type. The functional classification of joints relates to the degree of movement they permit. Functionally, joints are classified as one of the three types in the following table.
| Name | Functional classification | Example |
|---|---|---|
| Synarthrosis | An immovable joint | Suture between bones in the skull The joint between a tooth and its socket |
| Amphiarthrosis | A slightly moveable joint | Joint located in the pubic symphysis |
| Diarthrosis | Freely moveable | Wrist, ankle, shoulder, elbow, hip and knee. |
Joints types explained
Study the names and locations of joints in the following images.
Fibrous joints
A joint which lacks a synovial cavity. Within a fibrous joint, bones are held together by dense irregular connective tissue composed of collagen fibres that emerge from the matrix of one bone into the matrix of the next. Fibrous joints permit little to no movement.
Fibrous joints fall into three categories.
- Sutures
- Syndemoses
- Interosseous membranes.
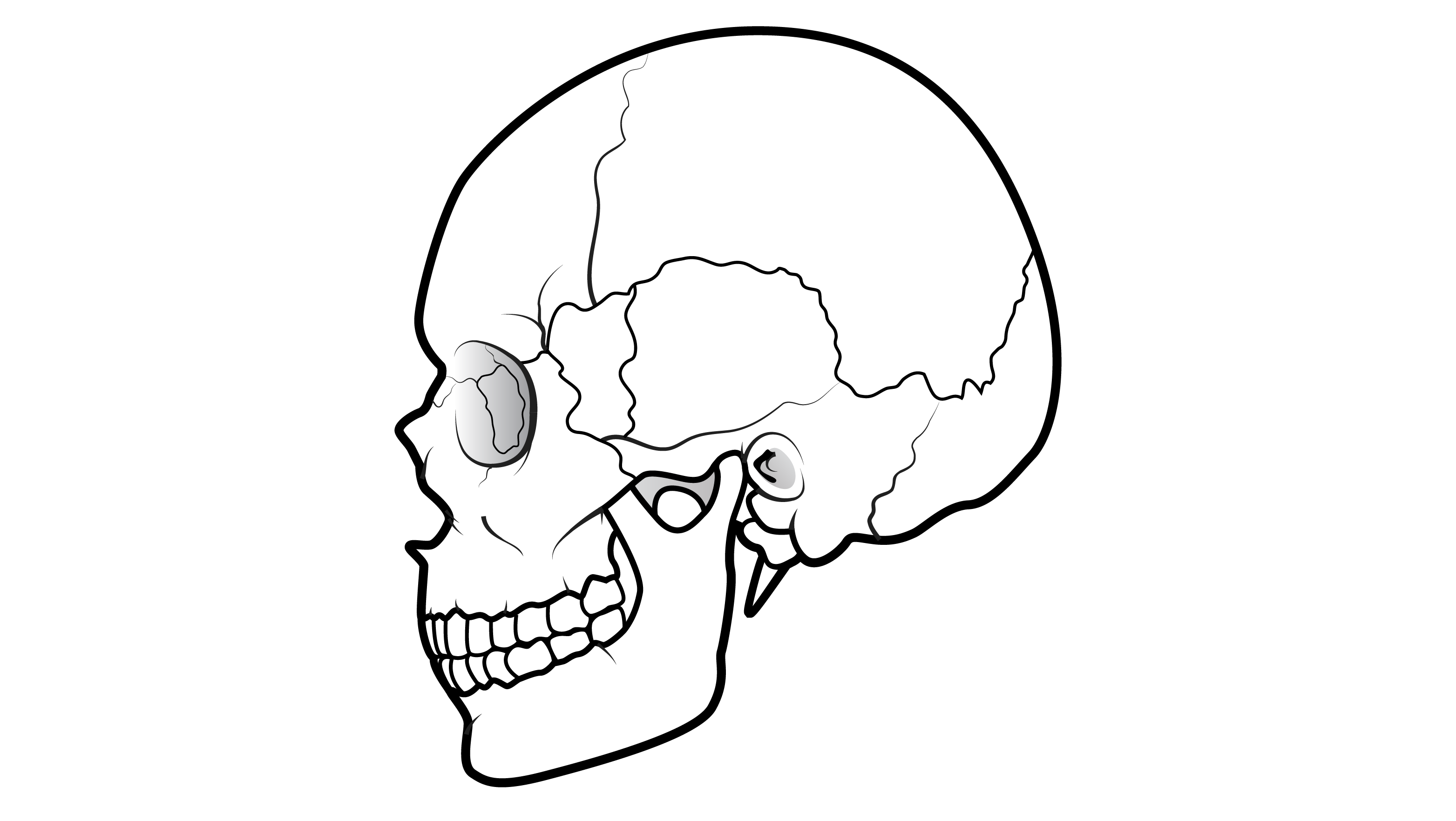
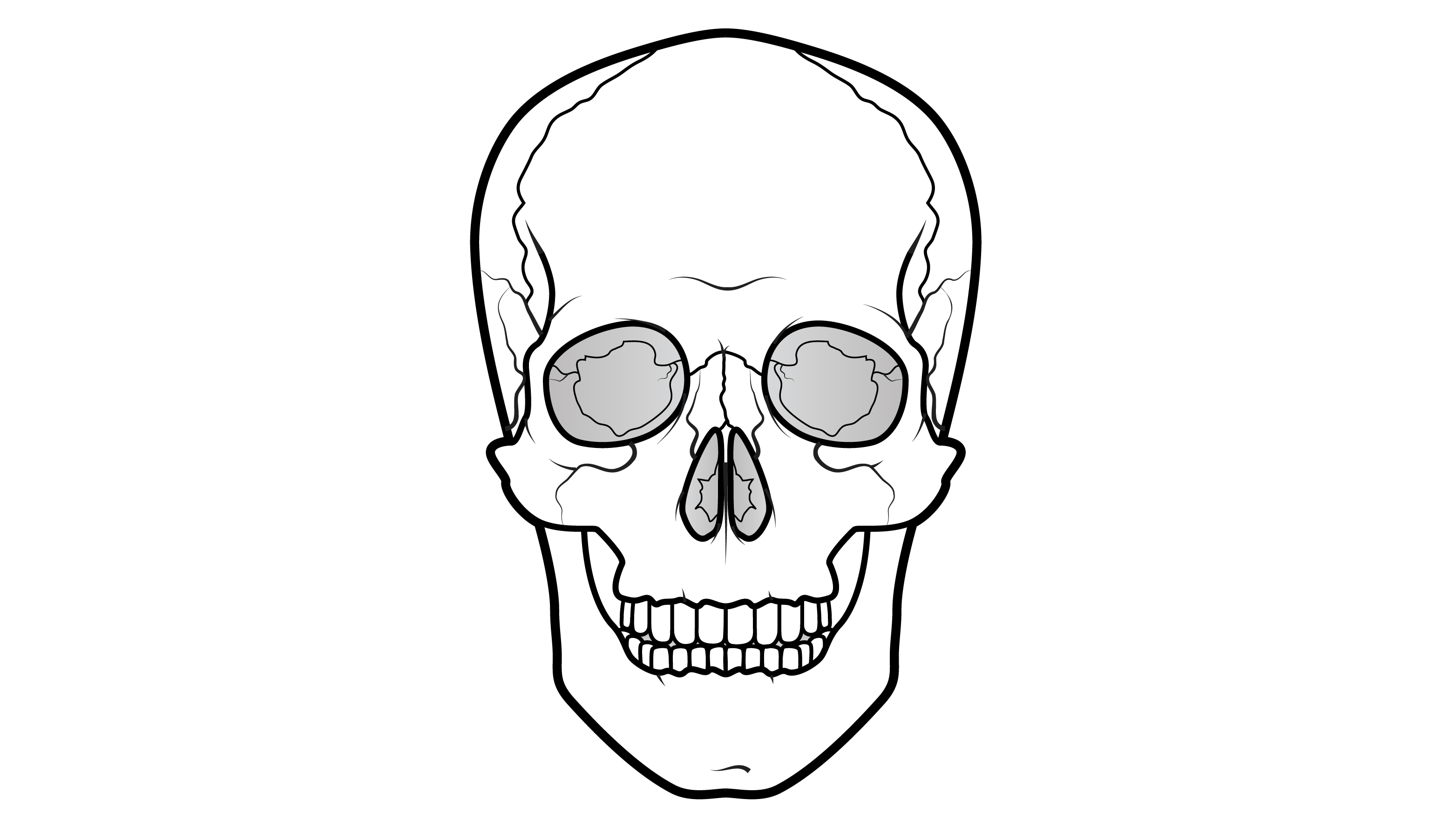
Sutures
Sutures are mmovable or slightly movable joints which are typically found between the bones of the skull. In older adults, these sutures are immovable (synarthroses), however, in children and infants they are slightly moveable (amphiarthroses). Here we see another example of structure and function: a baby's skull has 'soft spots' when born. It is this softer skull that permits movement and aids in childbirth. As the baby develops, we see the connective tissue turn to bone and the skull grows and solidifies.
Syndesmoses
Syndesmoses are immovable to slightly moveable (amphiarthrosis). A syndesmosis can be identified, by the lack of synovial cavity, and the distance between the adjoining bones in comparison to a suture. Within a suture, there is no space between the articulating bones. However, within a syndesmosis, there is more distance and volume of dense irregular connective tissue between the articulating bones of a syndesmosis. For example, teeth held in their socket (also known as 'gomphosis'). Another example is where two bones are held together by a ligament only (for example, the tibiofibular joint).
Typically, within a syndesmosis joint, the joining connective tissue is in the form of a ligament such as the periodontal ligament holding teeth in their sockets.
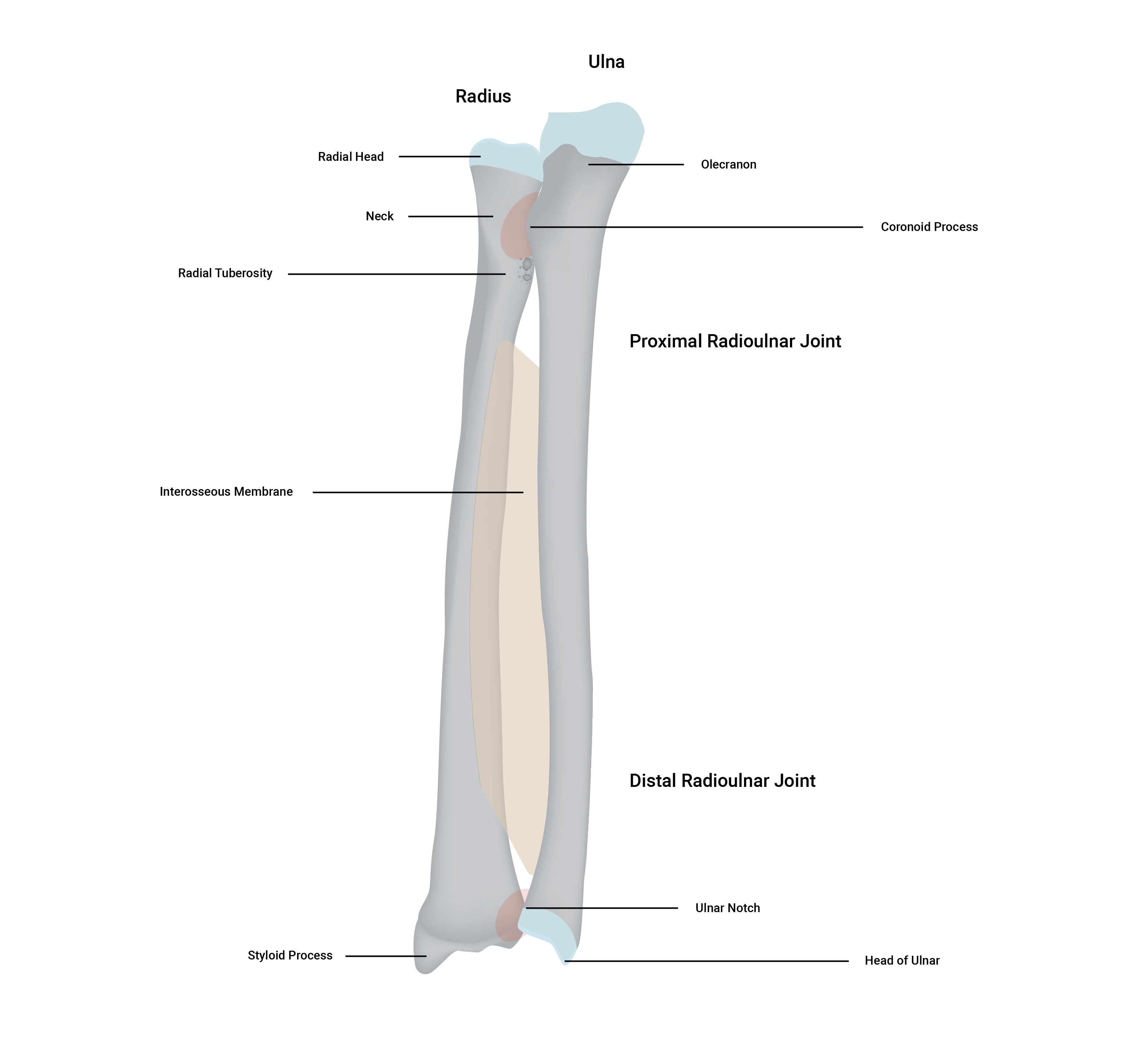
Interosseous membranes
The third fibrous joint category is the interosseous membrane. These are slightly moveable (amphiarthrosis) connection/articulation between two bones. This joint type is typically formed by a substantial sheet of dense connective tissue that binds neighbouring long bones and permits slight movement. There are two main interosseous membranes within the human body, between the tibia and fibula (shin bones) of the leg and the radius and ulna of the forearm.
Cartilaginous joints
Cartilaginous joints occur where the bones are bound by cartilage (either hyaline or fibrocartilage) which permit little to no movement. Like fibrous joints, cartilaginous joints lack a synovial cavity.
There are two types of cartilage that can join bones via a cartilaginous joint:
Softer and with more give. Glassy appearance, often with a bluish hue; Think gristle on the end of a chicken drumstick bone.
Tougher, denser, more rigid cartilage.
Cartilaginous joint classifications (based on structure)
Structurally, there are two categories of cartilaginous joints:
- Sympheses
- Synchondroses.
Symphyses
Symphyses (the plural of symphysis) refer to bones that are covered at the end in a layer of hyaline cartilage but are connected by a disk-like sheet of fibrocartilage. For example, the pubic symphysis within the pelvis, which provides strength and stability plus flexibility and movement during times such as pregnancy and especially childbirth. Another example is the site where the manubrium and the body of the sternum (breast bone) meet.
Synchondroses
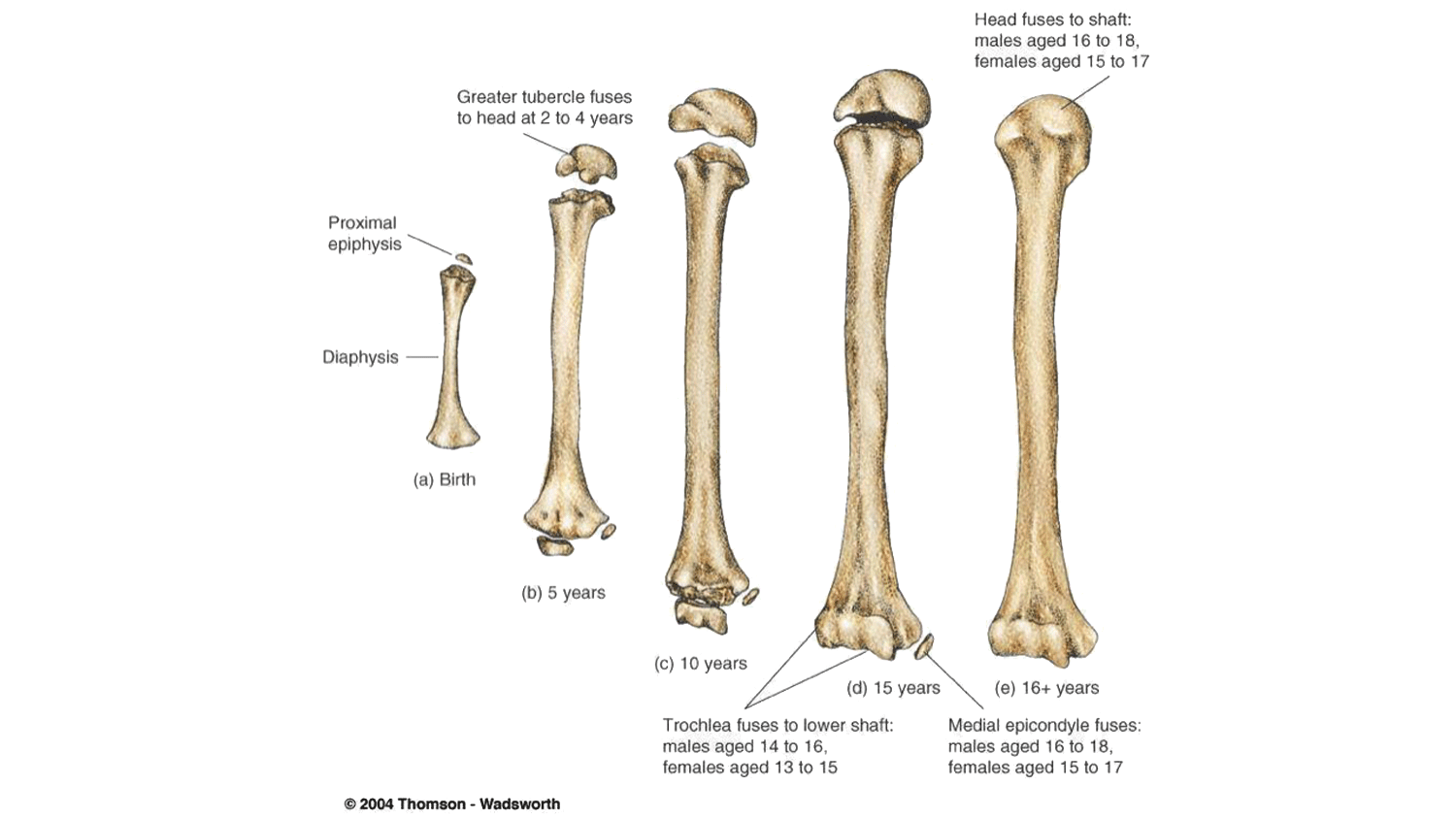
Synchondroses refers to where the articulating bones are connected via hyaline cartilage. For example, the epiphyseal plate (also known as growth plate) within long bones. Functionally, this joint begins its life as a synarthrosis because it provides no movement of the bones. However, as the bones elongate over time, the hyaline cartilage is replaced by bone and is then referred to as synostosis.
Synostosis joints
A synostosis is a type of suture that, as a person develops into adulthood changes its structural composition, and some/certain sutures are replaced by bone. When this occurs, this joint/articulation is no longer referred to as a suture but a suture that is now synostosis, where two bones have completely fused into one.
An example. The frontal bone of the skull (forehead bone) begins in two parts, however by the age of six, this is usually totally fused. The suture is now a synostosis that cannot move. The process is called 'ossification' (ossify = to turn into bone).These are fibrous and cartilaginous joints that ossify (or fuse together) as we mature, effectively, turning two bones into one. Magic!
Examples include:
- bones of the skull
- shafts and heads of long bones
- first rib to the sternum.
Synovial joints
The synovial joints are structurally and functionally different from their counterparts. As their name suggests, these joints are distinguished by the presence of a synovial cavity (the joint cavity which lies between the articulating bones). The structure of this joint (discussed in more detail shortly) offer many movement options, which earns them the title of 'freely-moveable' (diarthroses).
The ends of the articulating bones in synovial joints are covered with a layer of hyaline cartilage, called articular cartilage. Think of articulating bones; the naming of this cartilage, in this location should then make more sense. Synovial joints are some of our most used joints during activity.
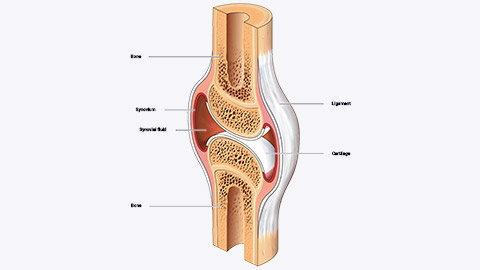
Typical structural components of a synovial joint include:
Synovial fluid
Synovial fluid is produced by the synovial membrane and housed within the cavity.
Articular cartilage
lines the end of the bones but does not join them.
Fibrous joint capsule
A fibrous joint capsule surrounds the joint, to join the two articulating bones and enclose the synovial cavity.
Synovial membrane
The synovial membrane secretes synovial fluid.
Accessory ligaments
Accessory ligaments are present in the region of the synovial joint, for example, the medial and lateral ligament of the knee. They are not part of a synovial joint directly, however, as their name suggests; they support the joint therefore it would be unfair to not give them a mention.
Synovial fluid-structure and function
A semi-thick, clear/pale yellow fluid (which resembles the consistency and appearance of an uncooked egg-white). This fluid forms a thin covering over the surface of the articular capsule and has three main and important functions:
- Lubrication
- Supply and distribute nutrients (including waste removal)
- Shock absorption.
Let's look further at these functions.
Lubrication
The fluid works like oil to prevent or reduce friction between the two bones.
Supply and distribute nutrients (including waste removal)
Joint movements force fluid into the tiny porous holes on cartilage and bone. This delivers nutrients to bone/cartilage to maintain density. The synovial fluid also contains cells that eat debris (waste removal cells) that ensure waste products such as carbon dioxide, metabolic wastes, and by-products of general wear and tear of the joint itself are dealt with. Fun fact: the cartilage tissue has no blood supply (avascular) so removing waste via blood vessels is not possible.
Shock absorption
The fluid in the capsule acts as a water cushion to dissipate force during loading and impact.
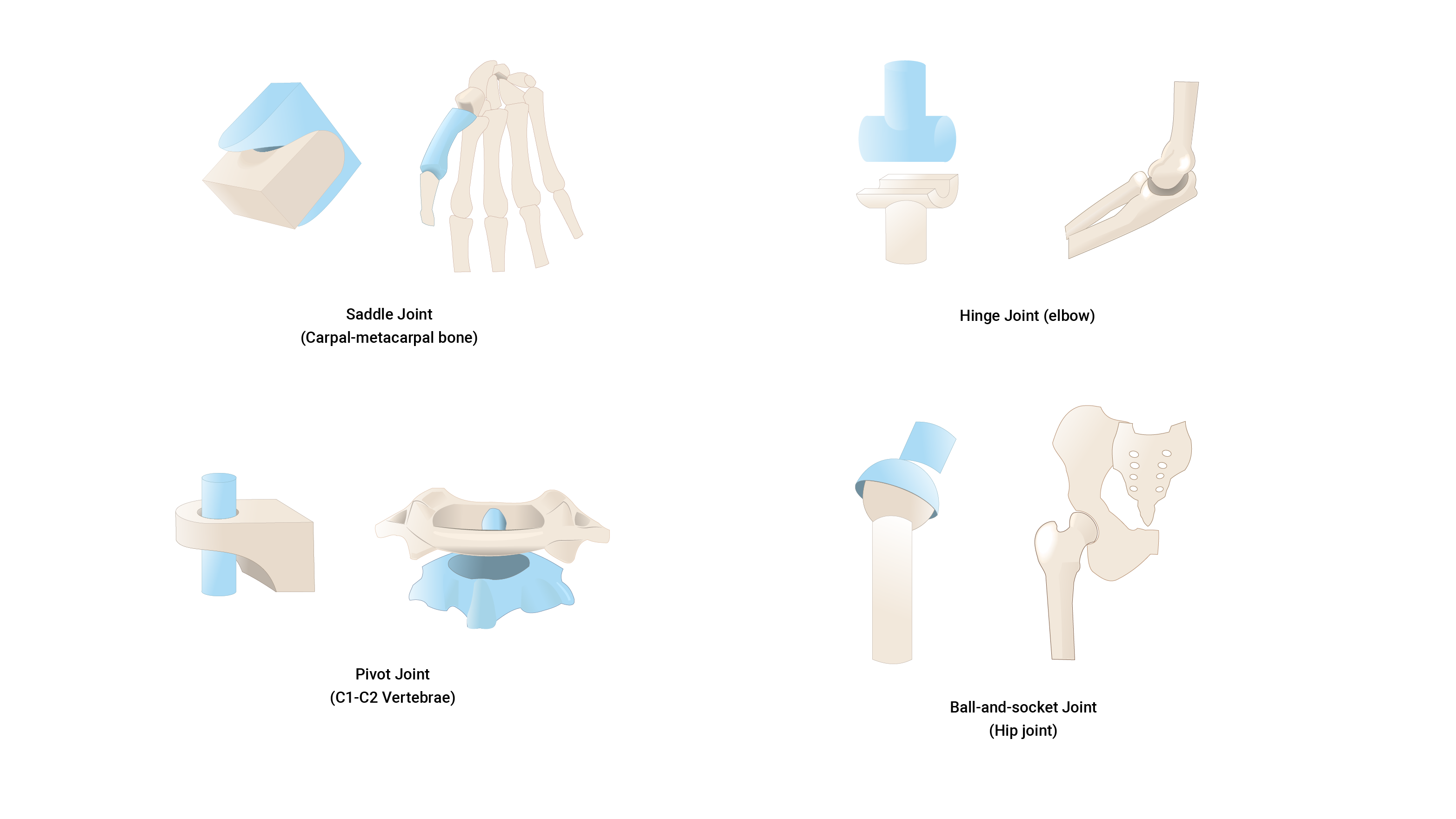
Synovial joint classifications (based on function)
Have a look at the following image and list of synovial joint categories. See if you can guess what common joints in the body belong in each.
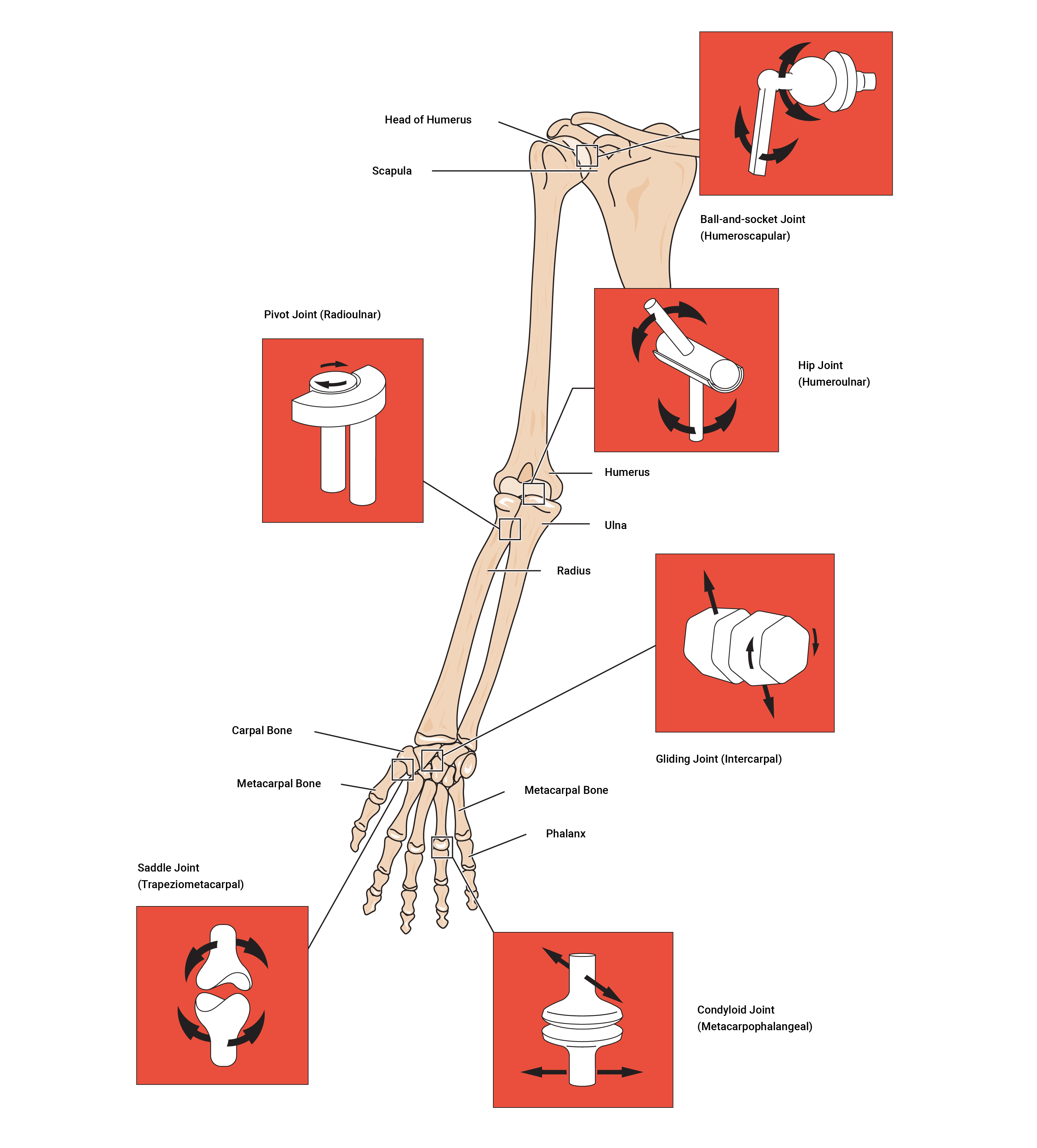
Ball and socket
Ball and sockets are due to the end of one bone having a 'ball' like end and the other bone having a 'socket' that the ball sits in. They move in multiple planes; for example, to flex, extend, rotate, abduct, adduct, and in circumduction.
Hinge
A hinge moves in one plane only, like a door hinge.
Pivot
A pivot is a pure 'rotating' joint.
Saddle
A saddle is when the end of one bone is like a concave 'saddle' that the other bone sits over like two legs. It allows a substantial range of movements.
Gliding
Gliding occurs when short bones glide along each other in all directions (but not far). Think of it like sliding two coins together between your fingers.
Condyloid
Condyloid refers to shallow ball and socket joints that can do everything a ball and socket joint can do except rotate.
There is a wide variety of joint types within the synovial family, and this is not surprising because as has been said, 'structure mirrors function'. This implies that there is a reason for all of these options and hey presto! There is a huge variety of movement types the skeleton can perform because of these joints.
Synovial joint movements
The movements provided by a synovial joint include:
- supination and pronation
- dorsiflexion and plantar flexion of the foot
- flexion and extension ( including hyperextension and lateral flexion)
- abduction and adduction
- inversion and eversion
- protraction and retraction
- elevation and depression
- opposition
- circumduction.
This is a long list! If there are any terms you are still trying to remember, add them to your personal terminology and reference guide.
Watch the following video for a summary of joint types and classifications
As we age, we know that after years of movement and lifestyle factors, we as humans are likely to experience some wear and tear, inside and out. Within the human skeletal system, degenerative conditions do present themselves, particularly as we age. Aging usually has an impact on functions such as; synovial fluid production with a joint, the thinning of articular cartilage, and the shortening of some muscular ligaments along with a decrease in flexibility. There’s a lot to look forward to! However, with supportive lifestyle factors, a good exercise regime, and diet, the onset of these can be delayed (if not totally prevented).
Arthritis
Arthritis is an inflammation of the joint cartilage. This inflammation has a negative impact on a joint's range of motion (due to a decrease in flexibility of the surrounding ligaments and factors mentioned above). Knowing about arthritis will help you develop safe and functional exercise programs for the elderly population that will help maintain the functions of ligaments, tendons, muscles, synovial fluid, and articular cartilage.
There are over a hundred types of arthritis but the two most common are osteoarthritis and rheumatoid arthritis. Can you identify the differences between them in the following images?
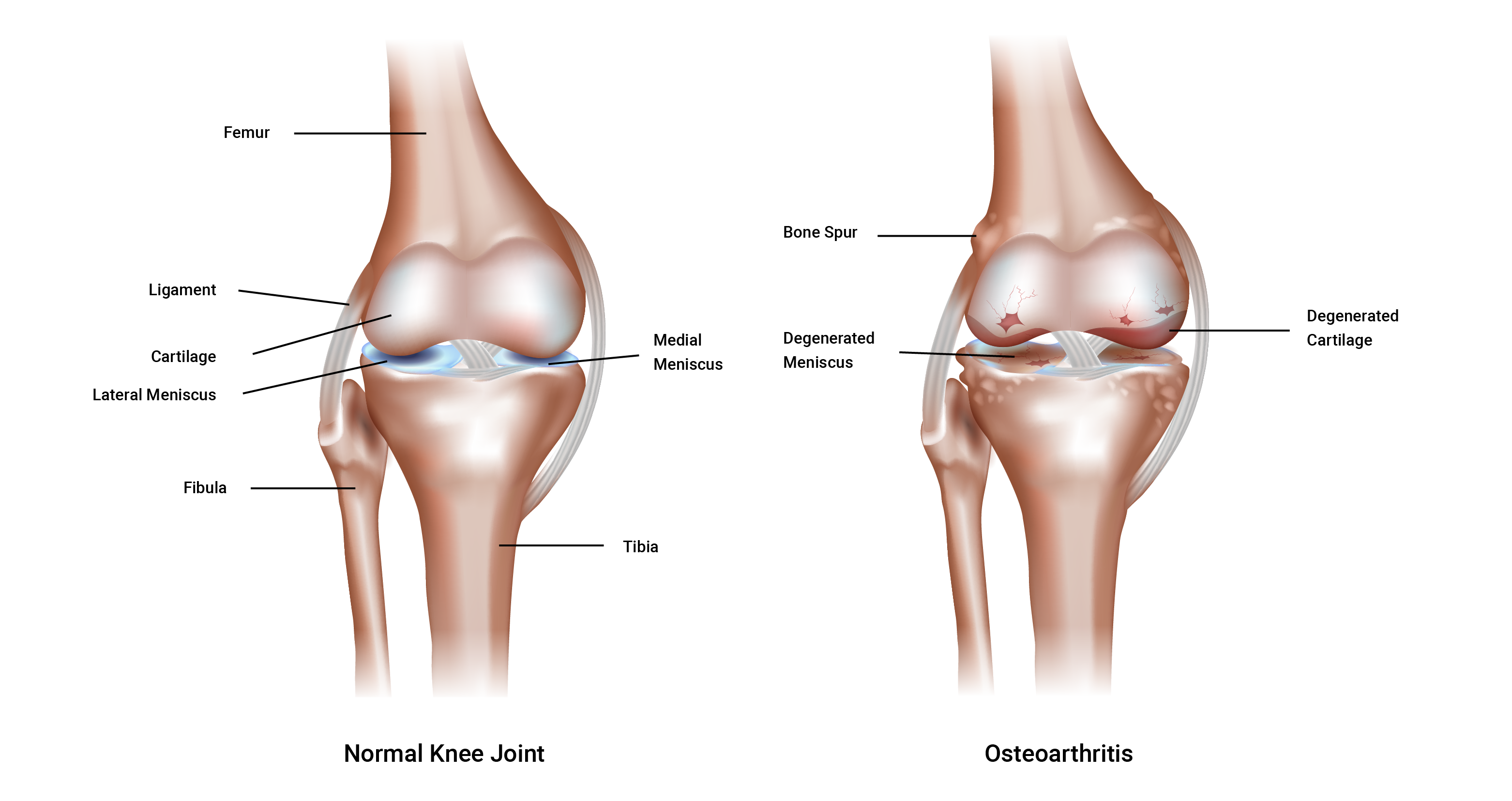
Osteoarthritis
Osteoarthritis is a largely age-related degeneration (this does not mean that younger generations are immune to osteoarthritis). It can be caused by wear and tear over time, or disuse due to lack of meaningful activity that can lead to weakened (thinner) cartilage. This is referred to as a degenerative joint disease where the cartilage is lost, from aging, obesity, joint irritation, muscle weakness, and general wear and tear. You can see the importance of effective exercise programming when working with clients who may have osteoarthritis. Their experience can be so much more than just 'a bit of cardio' style training.
If we break down the term, osteo = bone, ~athr = joint, ~itis = inflammation, we can begin to think along the lines of a condition related to joint inflammation. Compare the following images of a healthy joint and one with rheumatoid arthritis.
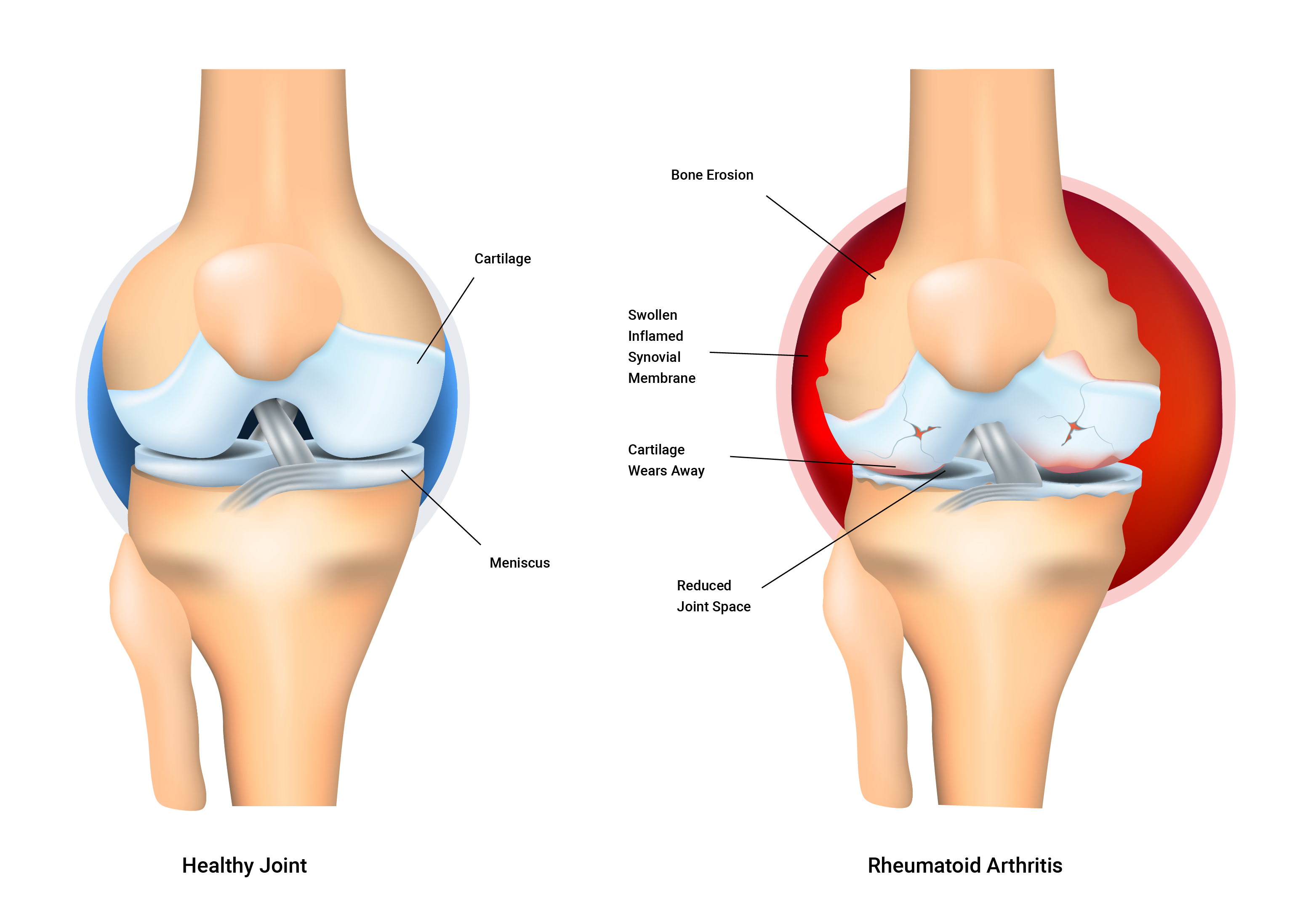
Rheumatoid arthritis
Rheumatoid arthritis is an auto-immune disorder. It occurs when your body’s immune system attacks the tissues of the body; in this case, its own joint linings and cartilage. These attacks affect the synovium, a soft tissue in your joints that produces synovial fluid that nourishes the cartilage and lubricates the joints.
Rheumatoid arthritis is a disease of the synovium that will invade and destroy a joint. It can eventually destroy the bone and cartilage inside the joint. It is typically characterised by inflammation (~itis) of the joint which can cause swelling, loss of function, and pain. Sadly, if one joint is affected, it is likely the other one will also be affected (but not usually to the same degree).
The exact cause of the immune system’s attacks is unknown. But scientists have discovered genetic markers that increase your risk of developing rheumatoid arthritis fivefold.
Articular cartilage and exercise
With exercise, the synovial fluid becomes less viscous (thick) and is more easily taken in by articular cartilage. This is beneficial (as we have learned) because the synovial fluid provides essential nutrients to nourish the bone and other cells remove unwanted debris and help keep the synovial joint 'clean and tidy'. Cartilage acts like a sponge and has tiny pores that allow fluid to enter and leave. That whole structure and function business again!
Exercise design should take into consideration the need for and the benefit of repetitive compression for nutrition and waste removal.
Ideal joint stability vs ideal range of motion
Unfortunately, it is difficult to achieve ideal joint stability and range of motion at the same time because an increase in one of these often occurs at the expense of the other. This should be considered when delivering a balanced and well thought out program design.
Joint stability (resistance to displacement)
Joint stability depends on three key factors:
- Joint ligaments
- Muscle tension
- Fascia tension.
Let's look at each of these.
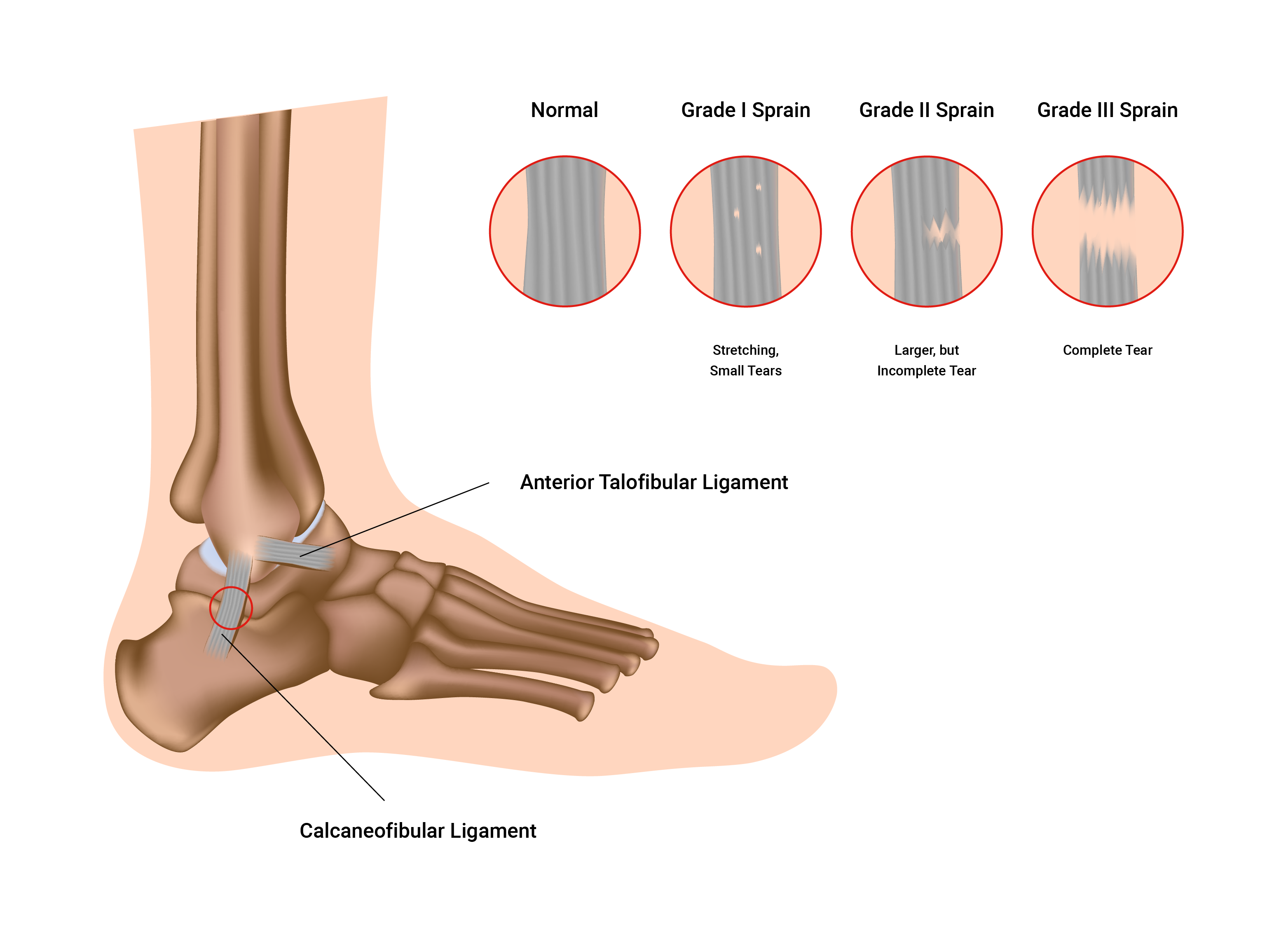
Ligaments
Ligaments are strong and flexible. They attach the ends of bones to form a movable joint. A ligament's main function is to maintain the correct relationship between bones. They also have receptors that monitor movement speed and range as well as resisting undesirable movements.
Think about this as you study the following illustration which shows different grades of a sprain.
Ligament injury (sprain)
Ligaments are not very elastic and if they over-stretched they may never regain normal length.
Once stretched their usefulness is permanently affected and joint stability is diminished. Think of an elastic band or a hair tie. Over time and repeated use they stretch and begin to lose their shape (become bigger) and if left to dry, they become rigid and stiff.
Sprains range in severity often referred to as a 'grade'. This scale-based terminology provides clear parameters outlining the current health and condition of the ligament (or ligaments) affected. Sprains range from first degree to third degree, with the third degree often representing a severe if not a full rupture of the ligaments as well as other signs and symptoms. Recovery time also increased from first to third-degree sprains. Typically ligaments (and tendons) have a lesser blood supply than muscles tissue (for example) which means that their nutrient delivery is less and therefore recovery will be slower.
Muscle tension
Muscles help static stability and provide dynamic stability (stability while moving). Strength training is an important defence against joint injury. Once ligaments are damaged (lengthened), muscles around the joint must be strengthened to maintain joint stability. This can lead to unfavourable changes in their range of motion.
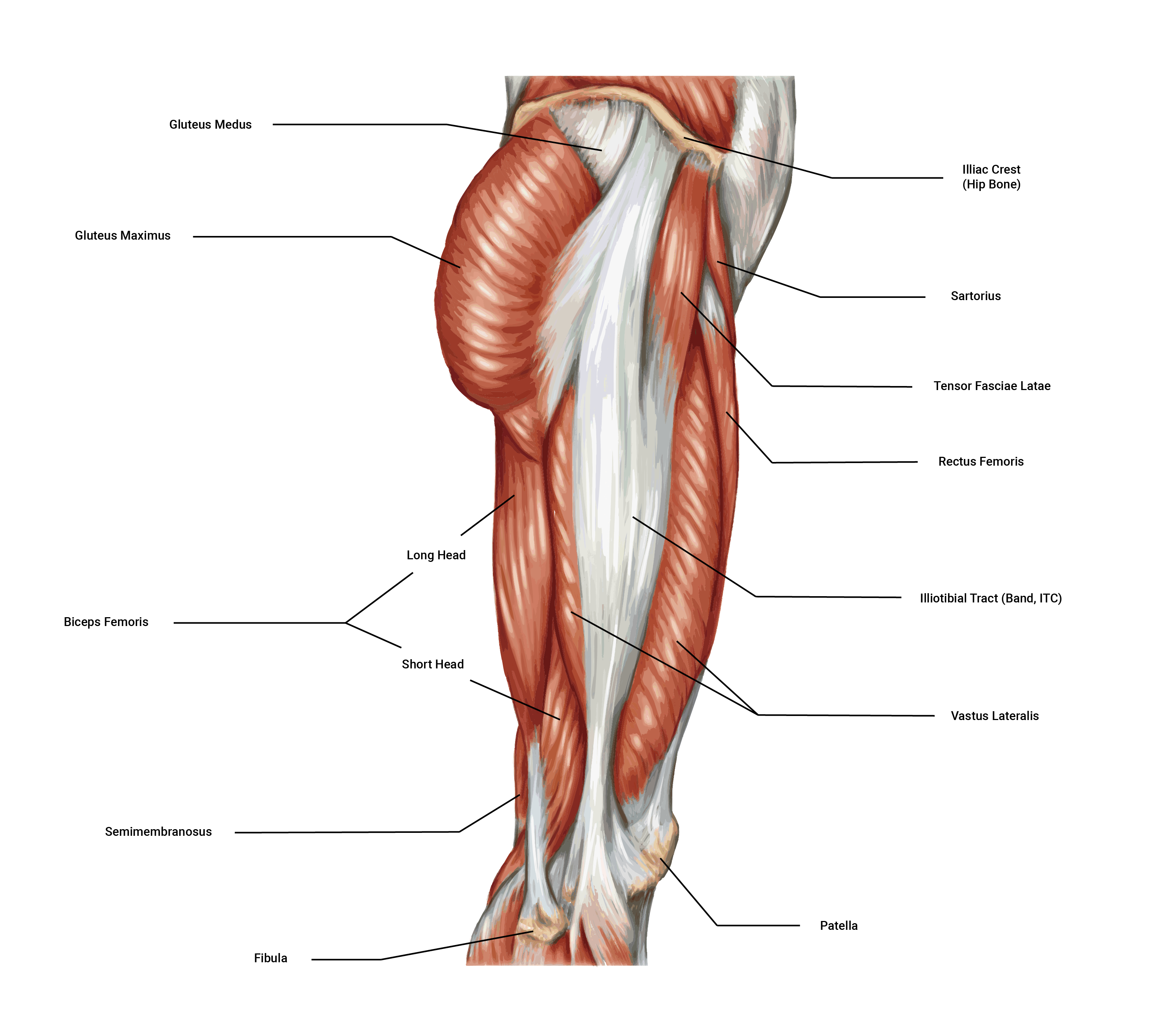
Fascia tension
Fascia is a connective tissue that wraps around individual muscle fibres and also groups of muscles. It is flexible and elastic within limits (for example, iliotibial tract, also known as the ITB). This facia supports joint stability/integrity by supporting muscle attachment. It can also cross over joints to provide extra stability. Structure and function yet again!
Menisci
Some loaded synovial joints (such as the knee) have flattened, shock-absorbing pads of fibrocartilage called menisci (the singular is meniscus) between the articulating surfaces of bones. These discs support the bones in the joint by binding strongly inside the joint capsule. They also offer depth to shallow joints and help absorb shock. The complete function of the menisci is not yet fully understood however they are known to be strong contributors to:
- absorbing shock
- providing cushioning and padding in between bony surfaces
- distributing synovial fluid over the articular surfaces of the joint.
Factors affecting joint range of movement
Three key factors affect the range of joint movement.
- Muscles and their tendons (flexibility)
- Bulky tissue (fat, excessive muscle)
- Disease and/or condition (pain).
Pliability of muscle and tendon
This is the single most important factor in joint range of movement. This can only be increased through dedicated and regular stretching. Warning: There is also a genetic predisposition to flexibility.
The bony structure of your joints will ultimately determine the range of motion you can achieve; that is, deep vs shallow sockets, and angle of the bones at insertion. Trying to stretch beyond your structural limitations will cause bone on bone contact and may result in bony lesions or spurs that result in ongoing pain.
Bulky tissue
Excess fat mass may make a person more restricted in their movement and function (as well as putting additional strain and pressure on the internal organs). Excess muscle mass can restrict the range of movement at joints if flexibility is not maintained. It is possible to have both though!
Disease, illness or condition
Through the course of this topic, you have now learned about the structure and function of a joint and its components. With this in mind, you now have a greater awareness of the implications should an aspect of their structure change, and the impact this would have on the functional capacity of the joint.
In this topic, we focused on we focus on the names, structure, function and classification of joints within the skeletal system. You learnt about:
- joint structure and function
- joint nomenclature (naming system)
- different joint types and classifications
- common joint conditions
- exercise and joint considerations.

