In this topic, we focus on the structure and function of the components and mechanics of the cardiovascular system. You will learn:
- an overview of the cardiovascular system
- structure and function of the components of the cardiovascular system
- circulatory system of the blood
- structure and function of blood
- physiology of blood pressure
- measurements of heart function.
Terminology and vocabulary reference guide
As an allied health professional, you need to be familiar with terms associated with basic exercise principles and use the terms correctly (and confidently) with clients, your colleagues, and other allied health professionals. You will be introduced to many terms and definitions. Add any unfamiliar terms to your own vocabulary reference guide.
Activities
There are activities throughout the topic and an end of topic automated quiz. These are not part of your assessment but will provide practical experience that will help you in your work and help you prepare for your formal assessment.
The Cardiovascular system (CV system) is integral to every facet of human life an athletic performance. The cardiovascular system (cardio~= heart, vascular~= blood or blood vessels) is composed of three interrelated components:
- The heart
- Blood vessels
- Blood.
The overall role of the cardiovascular system is to provide essential nutrients to the cells and tissues of the body as they require it and remove waste products from the body. This is achieved via a united combination of three components working in unison.
This topic will guide you through the structure and function of the cardiovascular system. We also have an in-depth look at each of its components and their contribution to athletic performance as well as the maintenance of homeostasis. Let’s take a look at the components of the CV system.
This short video shows the internal structure of the heart. Watch it to get familiar with the structure of the heart before we move on.
The heart is the 'battery' of the cardiovascular system. Without the heart beating and pumping blood through our vessels, the CV systems would not be able to remove waste and deliver nutrients throughout the body. Let’s take a look at the structure and function of the heart.
Heart function
The heart has one primary function. In order for the body to stay alive, each cell must receive a continuous supply of nutrients and oxygen. At the same time, carbon dioxide and other materials produced by the cells must be transported away from the tissues and removed from the body
These processes are continually maintained by the body’s cardiovascular system (circulatory system). It is the heart's job to produce the pressure required to move blood between the heart and lungs, and the heart and body tissues, pump blood around the body and maintain homeostasis.
Did you know: Your heart beats approximately 10,000 times a day, this amounts to approximately 35 million beats in a year and 2.5 billion times in an average lifetime.
Heart structure
Heart Size
Fun fact: Your heart is roughly the same size (but not the same shape) as your fist and weighs approximately 250g for females and 300 g in males.
Chambers of the Heart
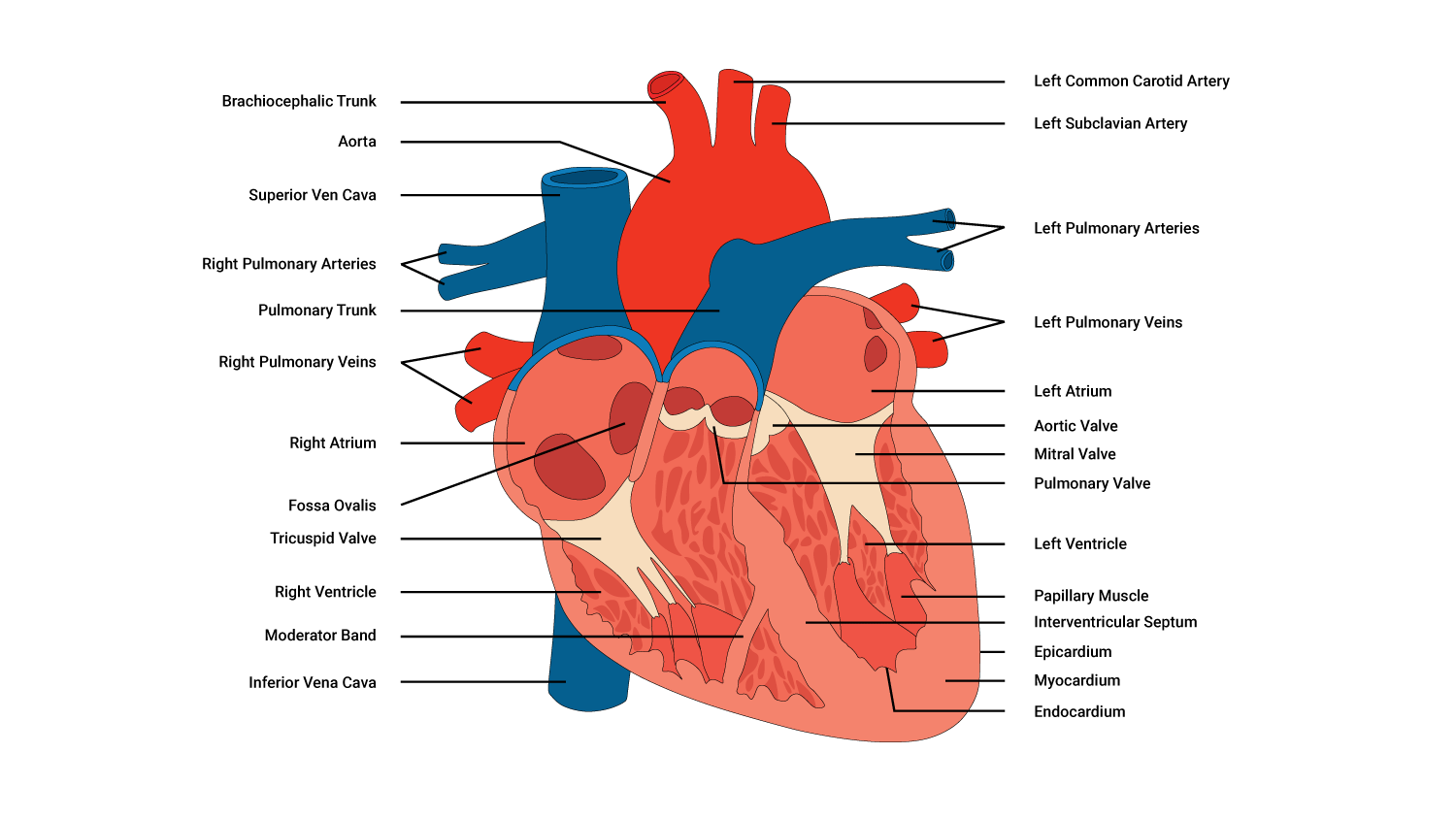
Anatomically, our heart is composed of four separate chambers that play their own role in terms of how the heart performs its pumping action. There are two superior receiving chambers (the atria) and two inferior (below the atria) pumping chambers (the ventricles) with one of each on the right and left portions of the heart. You can see these in the following diagramme:
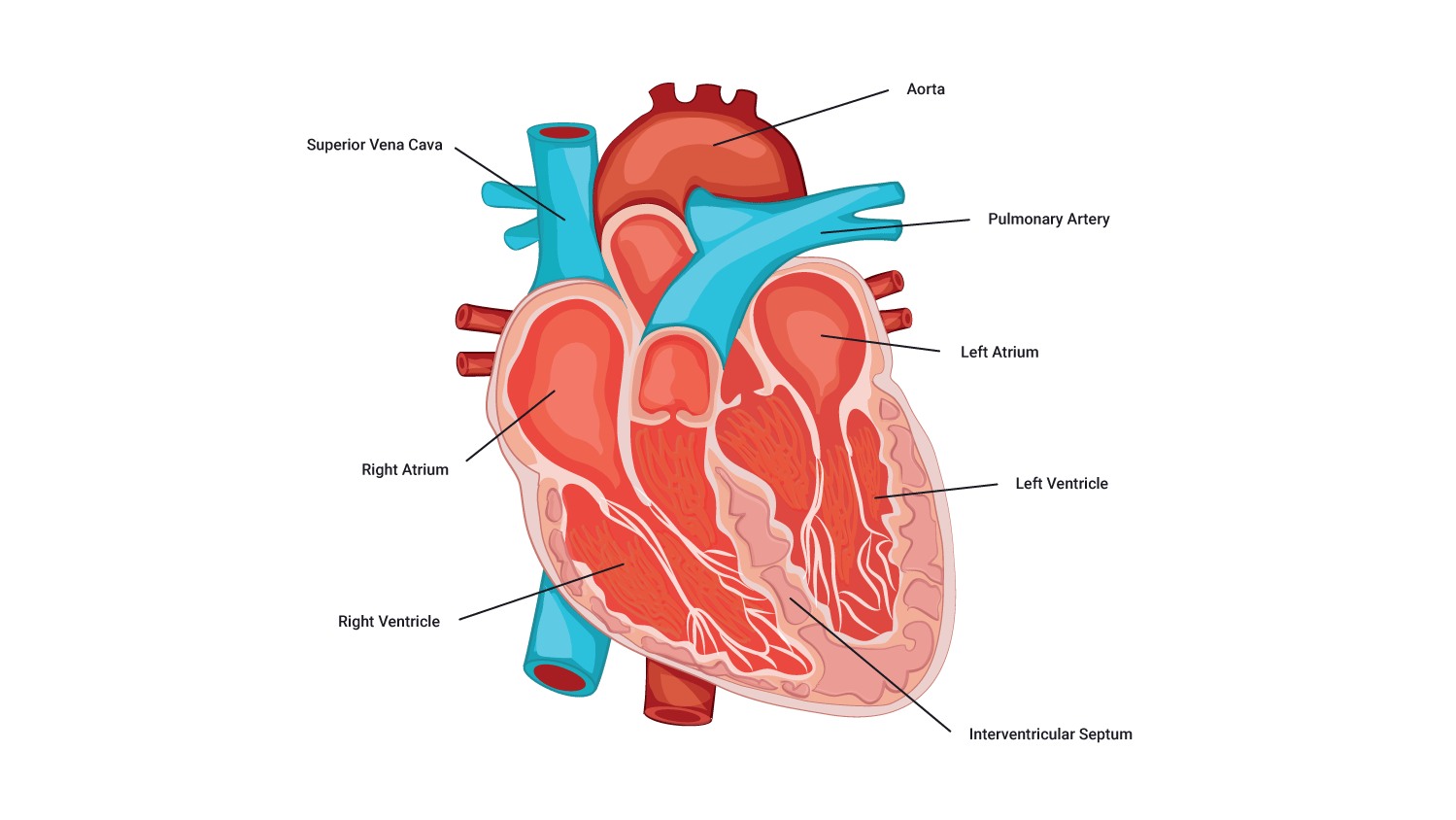
Right and left atria: Receiving chambers
The right and left atria receive blood returning to the heart. The right atrium receives de-oxygenated blood returning from the body tissues, while the left atrium receives oxygenated blood from the lungs. Between the right and left atria is a layer of tissue called the atrial septum that separates the left and the right receiving chambers.
Right and left ventricles: Pumping chambers
The right and left ventricles are the heart pumps. They receive the blood from the corresponding atria via 'gateways' called valves which we will look at more closely shortly. These valves open when there is sufficient pressure pushing against them, thus controlling the rate and flow of blood from the atria to the ventricles. Is it the job of the ventricles to pump this blood to relevant parts of the body depending on the oxygen status of the blood.
The right ventricle pumps deoxygenated blood to the lungs, while the left ventricle pumps oxygenated blood to the body tissues.
Heart valves and their role in blood flow
There are four valves present within the heart, two on the right and two on the left-hand side of the heart:
- Tricuspid valve: located between the right atrium and right ventricle
- Pulmonary valve: located in the pulmonary arch between the right ventricle and the pulmonary arteries
- Bicuspid valve: (also known as the mitral valve) located between the left atrium and left ventricle
- Aortic valve: located between the left ventricle and aorta.
The main role of the valves is to ensure one-way blood flow. Blood moves from an area of high blood pressure to an area of low blood pressure. The valves open when there is enough pressure in one chamber, pushing against valves and stimulating them to open and let blood pass through.
Work of the heart valves
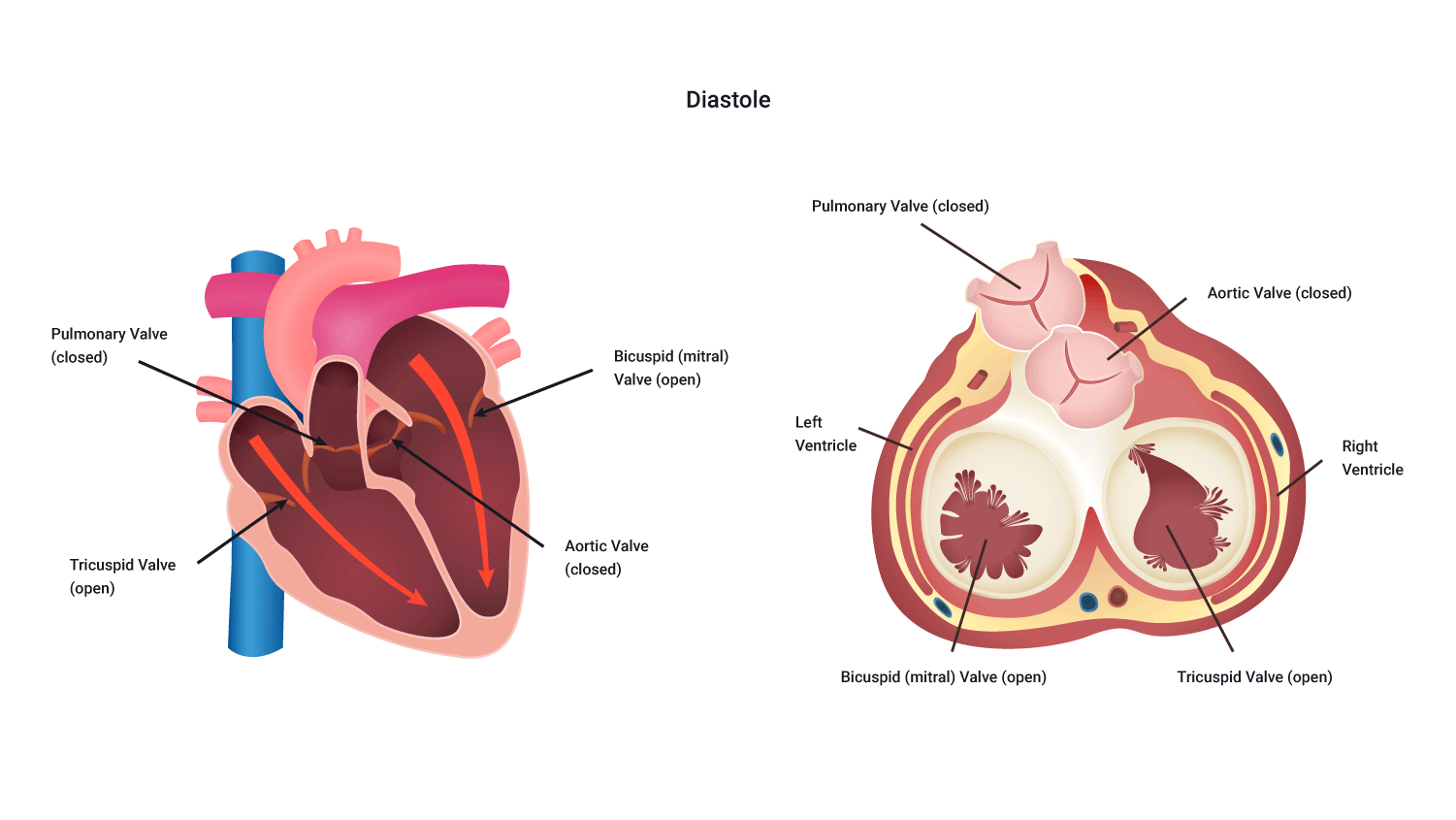
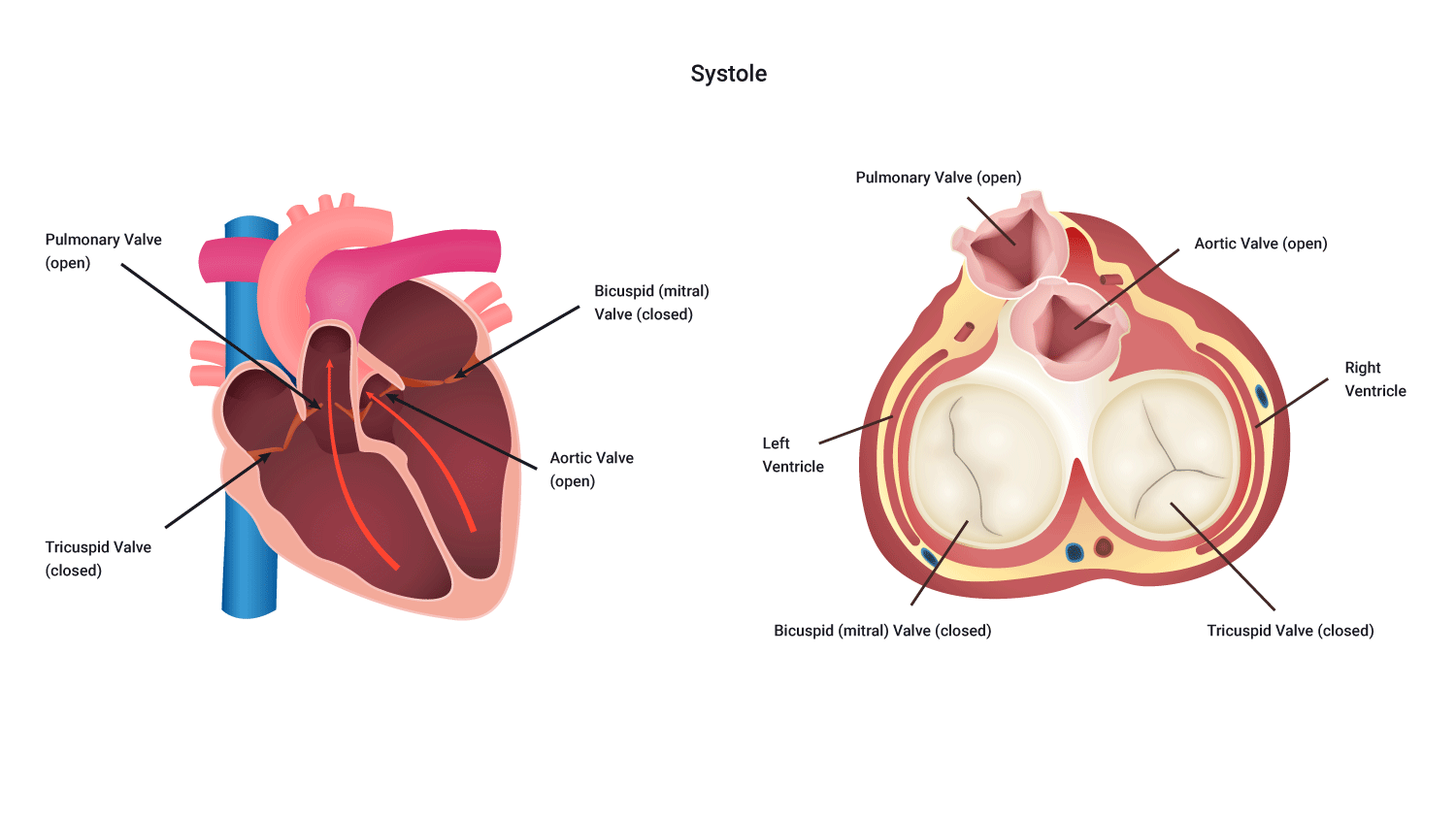
The valves work harmoniously to ensure sufficient pressure is attained to propel blood to the locations it needs to go. By closing as the chamber fills, enough pressure is generated that when the valve opens, blood forcefully makes its way into the next chamber, where it stretches the walls of that chamber allowing for a more forceful beat.
Their unique structural design ensures that they close when blood pushes back on them therefor preventing backward flow of blood (here we see the unique relationship between structure and function). The valves perform their important functions during each phase of a heartbeat, systole (a contraction of the ventricles) and diastole (relaxation of the ventricles).
Nutrient supply of the heart
The heart is a specialised muscle and like any muscle, the heart requires oxygen to stay alive. Ironically, our heart contains oxygen-rich blood however, the heart cannot gain its oxygen from the blood inside it. Instead, it is delivered O2 rich blood by the coronary arteries. The heart receives oxygen via the coronary arteries; these arteries branch off into smaller arteries that envelope the heart.
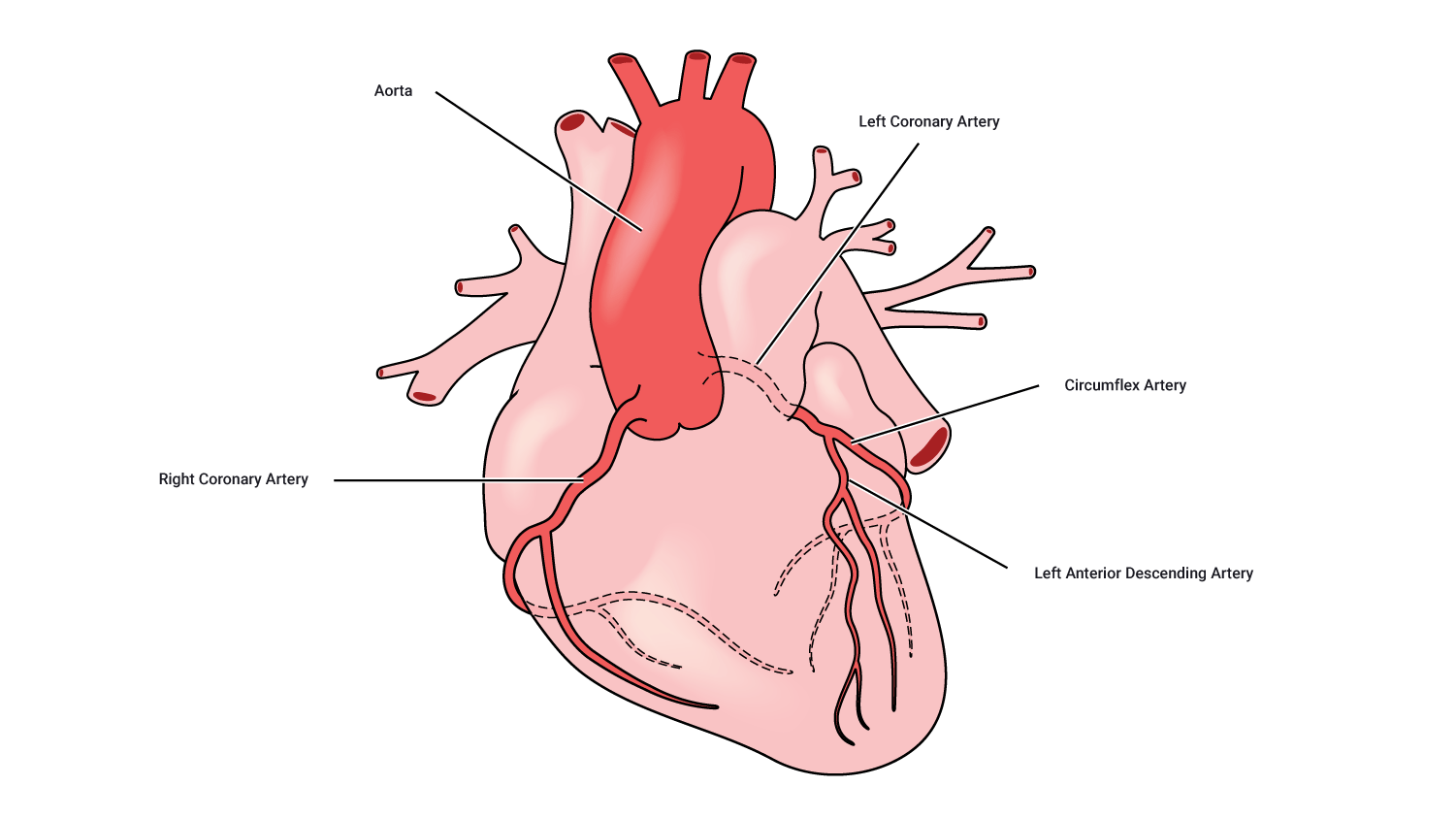
Typically, there is one artery on the right side and one on the left, with the left one generally being the larger. This is because the left side of the heart pumps blood to the body whereas the right-hand side pumps blood to the lungs.
The left main coronary artery divides into two sizable branches, the left anterior descending (supplying the front of the heart) and the left circumflex (wrapping around the left side and back of the heart). The right coronary artery supplies the back of the heart.
Blockages of these vessels are one of the leading causes of death in our society.
Muscular tissue of the heart: Myocardium
As mentioned, the heart is composed primarily of muscular tissue. We have noted how this receives nutrients in order to be able to perform its role as the body’s pump. However, there is a little more to its structure that is important to highlight and which further supports its pumping action. This should come at no surprise; but 'structure mirrors function' and here we see this in the muscular tissue of the heart, the myocardium.
When you look at a cross-section of the heart (see the following diagramme), you can see a subtle difference in the myocardium. If you look closely (well, not too closely) you can easily see that the left-hand side of the heart (on the right), particularly around the ventricle is substantially thicker than around the right ventricle. This is yet another example of structure and function. This is because the left ventricle pumps blood around the entire body, so it needs to be strong enough to create sufficient pressure to do so.
Heart muscle anatomy
How the heart beats
Ever wondered how the heart can manage to continue beating even after it has been removed from the body? The cardiac muscles of the heart are referred to as autorhythmic fibres because they are self-excitable. This refers to the fact that they repeatedly generate their own action potentials that trigger contractions of the heart muscle fibres.
Conduction System of the Heart
The origin and direction (conduction pathway) of electrical excitability are as follows:
- The sino-atrial (SA) node
- The atrioventricular (AV) node
- The bundle of His
- The left and right bundle branches
- The Purkinje fibres.
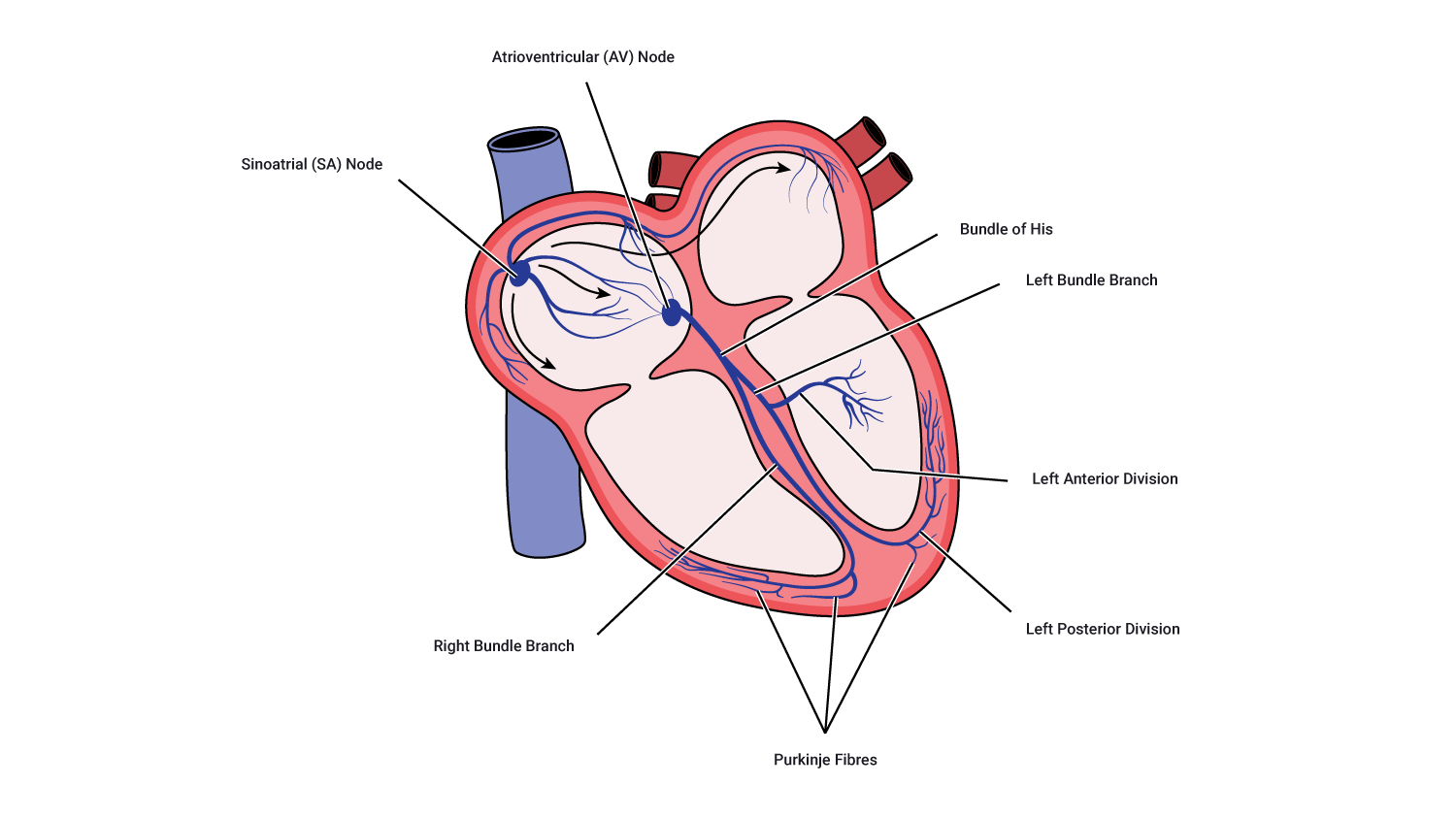
Pathway of heart conduction
- Excitation begins with the SA node which is responsible for creating the action potential. The SA node determines the rate of firing of an action potential, therefore, it is referred to as the pacemaker.
- This action potential (when at a sufficient threshold) causes a wave of excitation across the atria which in turn, results in the atria contracting.
- As the action potential the atrioventricular node (AV node), the signal is slightly delayed which allows time for the ventricles (the larger of the two chambers) to fill.
- The action potential reaches the bundle of His where it then enters both the left and right branches. These branches extend through the atrioventricular septum (the section between the atria and ventricle) and towards the apex of the heart.
- Lastly, the Purkinje fibres receive the action potential around the apex of the heart and rapidly conduct it towards the remainder of the ventricles. This causes the ventricles to contract, pumping blood out of the ventricles and to their respective destinations.
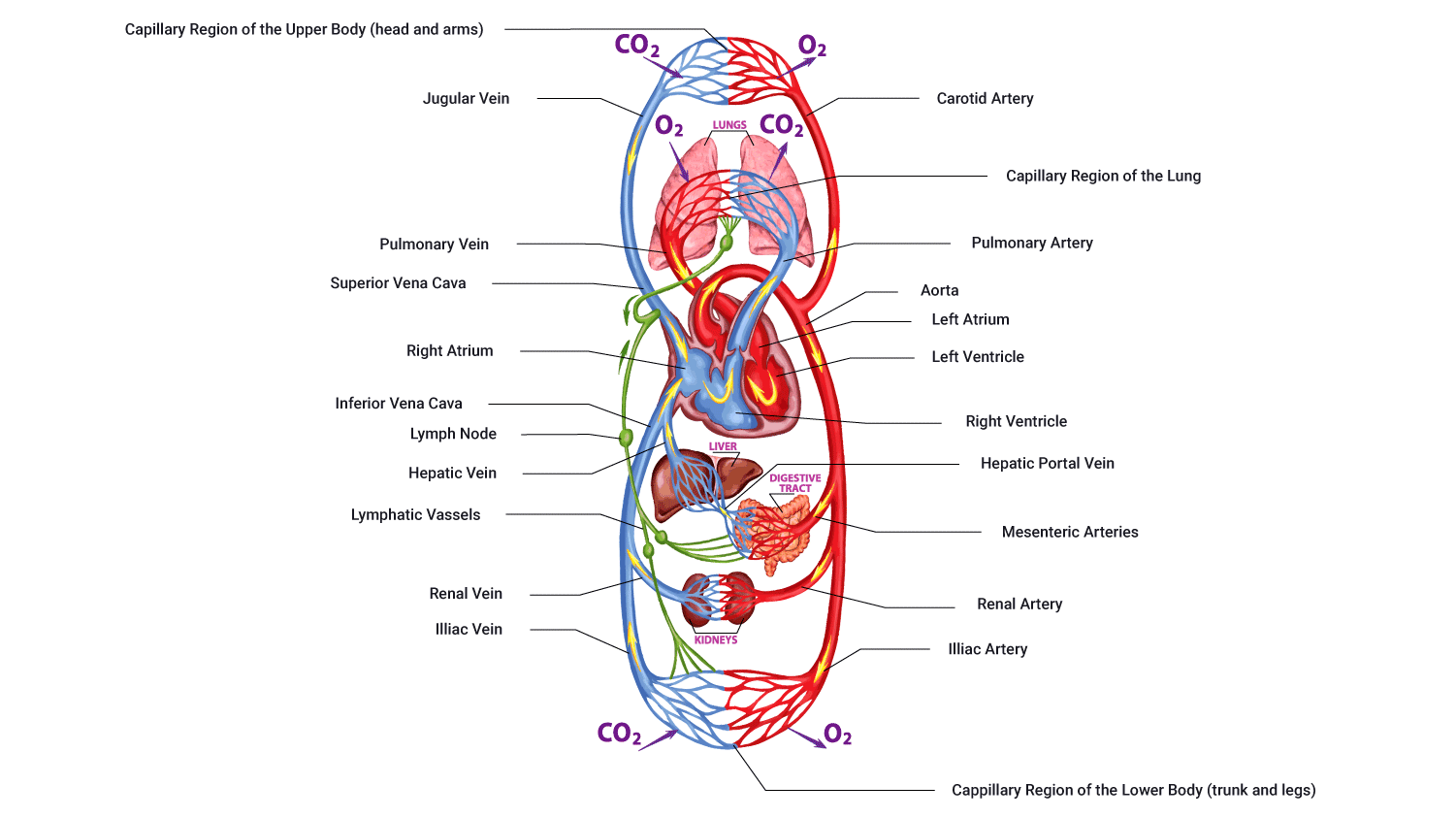
Blood vessels are the pathways for blood around the body. There are five blood vessel types in the human body:
- Arteries
- Arterioles
- Capillaries
- Venules
- Veins.
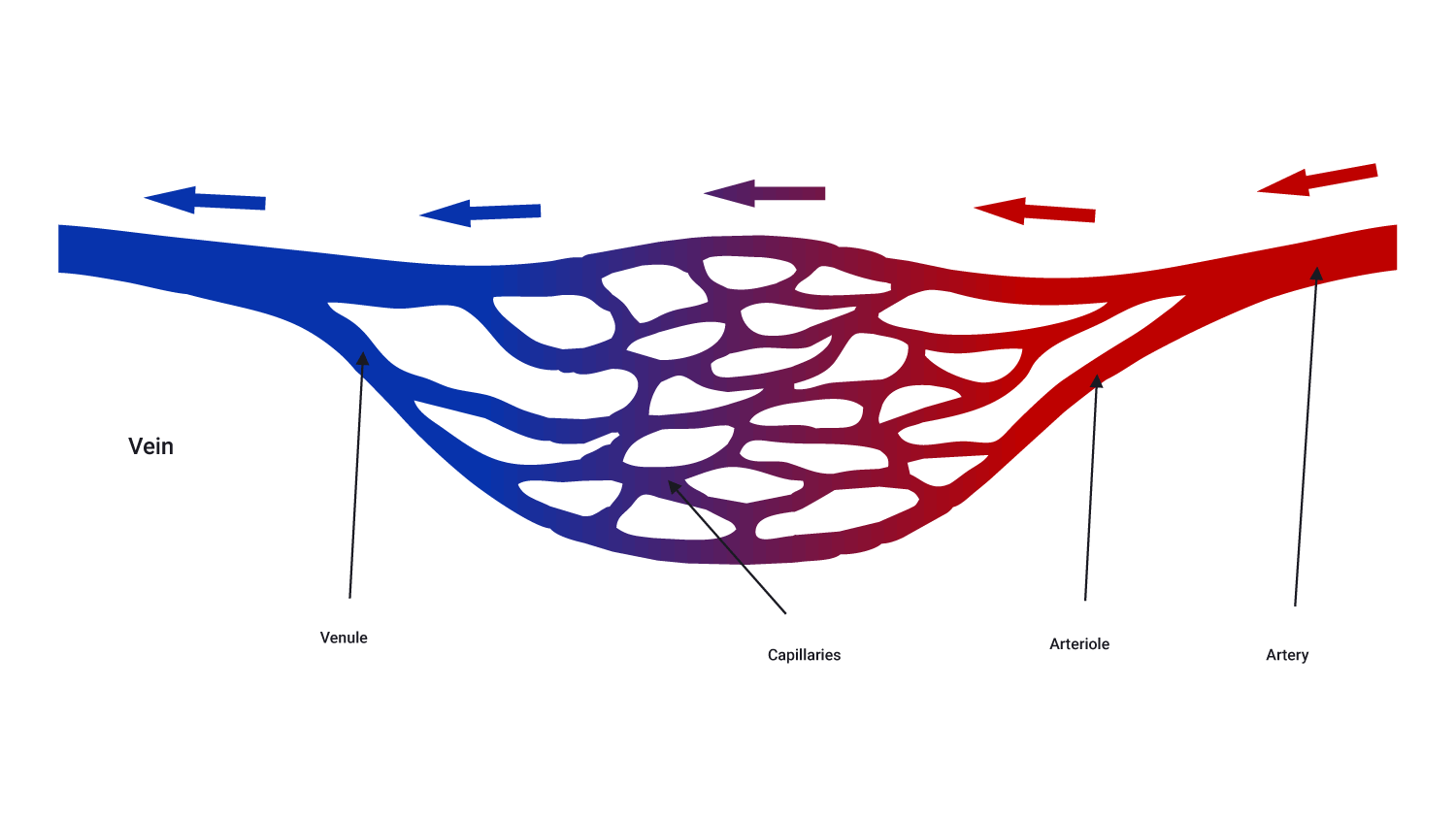
Arteries
Arteries are the largest of the blood vessels and carry blood away from the heart. There are two types:
- Systemic: Systemic arteries carry blood from the aorta to be distributed to the body tissues. These carry only oxygenated blood.
- Pulmonary: Pulmonary arteries carry blood from the pulmonary trunk to be distributed to the alveoli in the lungs. These carry only deoxygenated blood.
Arteries branch at intervals along their length into arterioles which are tiny branches of arteries that lead to capillaries. Along with smaller arteries, these are under the control of the sympathetic nervous system and constrict (narrow) and dilate (widen) to regulate blood flow.
Arterioles
These are small, largely microscopic structures that deliver blood to capillaries. Arterioles are the main effectors of blood pressure.
Capillaries
Capillaries are tiny (extremely narrow) blood vessels, of approximately 5-20 micro-metres (one micro-metre = 0.000001metre) diameter.
There are networks of capillaries in most of the organs and tissues of the body. Capillaries are supplied with blood by arterioles and are drained by venues. Capillary walls are very thin which allows them to exchange substances and gasses between the blood and the surrounding tissue (for example, oxygen, carbon dioxide, water, salts).
Venules
Venules are minute vessels that drain blood from capillaries and into veins. Many venules unite to form a vein. Unlike arterioles, venules have no muscular diameter control, instead, they drain blood from capillaries and pass it on into veins for return to the heart.
Veins
Veins transport blood towards the heart. There are two types of veins:
- Systemic: Systemic veins carry deoxygenated blood back to the right atrium of the heart (for example, superior and inferior vena cava).
- Pulmonary: Pulmonary veins carry oxygenated blood from the lungs back to the left atrium of the heart.
Veins have valves that aid the return of blood to the heart by preventing blood from flowing in the reverse direction.
The direction of blood flow through the heart
Blood follows a certain pattern through vessels both into and out of the heart. In anatomical diagrams, you will usually see blood depicted in two colours: blue and red.
- Blue represents deoxygenated blood which indicates a lack of oxygen being carried by this portion of blood and therefore likely heading back to the lungs to receive oxygen inhaled form the environment.
- Conversely, red indicates oxygen-rich blood which has been oxygenated and is now en-route to the tissues and cells of the body to provide an energy source for metabolic activities such as digestion, muscle contraction, and cell communication.
Take a look at the following image which highlights the direction of travel of blood both into and out of the heart.
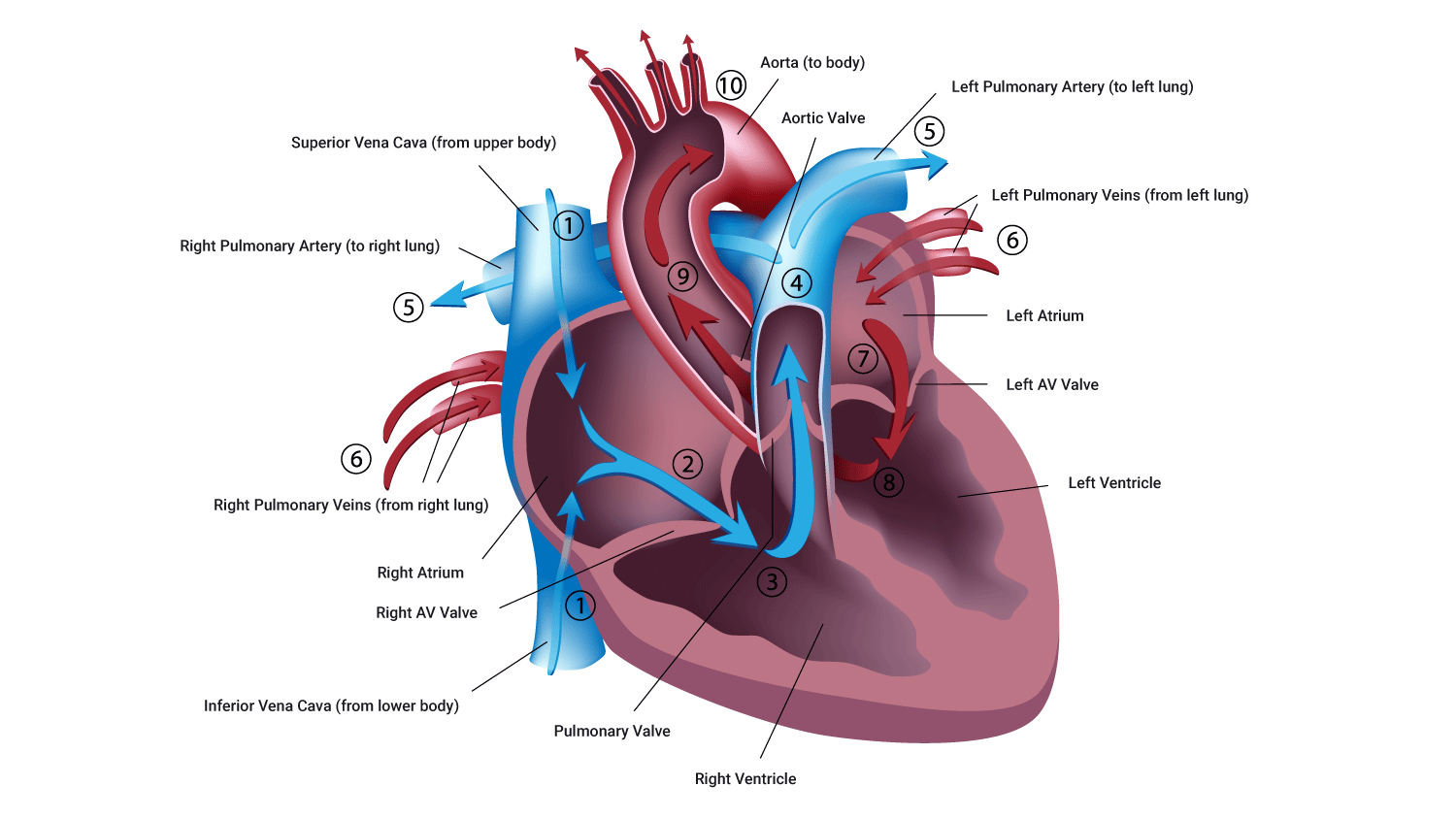
Remember that when you are looking at a picture of a heart front-on, the left is on the right and the right is on the left...right?
The pathway of blood through the heart is of great physiological importance when working in industries such as health and fitness. Becoming comfortable with the direction of blood and the factors involved in moving blood through the heart and the body is valuable for working with different clients and designing the best programs for their needs. This knowledge plus your understanding of the two circuits of the circulatory system and ability calculating capacities suitable for your clients (both of which we will cover in this topic) are incredibly valuable tools to draw on when you design a tailored routine for your clients.
Let's look at the pathway of blood through the heart.
Deoxygenated blood flow (right side of the heart)
- Deoxygenated (oxygen-poor) blood arrives into the right atrium (receiving chamber) from the superior vena cava ( upper body) and from the inferior vena cava (bringing blood from the lower body).
- Blood gathers in the right atrium which applies pressure to the atrium walls and the tricuspid valve.
- When a sufficient volume of blood arrives in the right atrium, the tricuspid valve opens, and blood then enters the right ventricle.
- When the ventricle is full, pressure is applied to the rear of the tricuspid valve which in turn, closes the tricuspid valve (preventing backflow of blood while the ventricle contracts).
- The right ventricle contracts, pushing blood out of the ventricle, up the pulmonary artery which is enabled by the opening of the pulmonary valve.
- This deoxygenated blood then arrives, via the pulmonic artery to the lungs where gas exchange takes place and the blood is refreshed with oxygen, and carbon dioxide is removed (through exhalation).
***AT THE SAME TIME***
Oxygenated blood flow (left side of the heart)
- Oxygen-rich blood arrives via the pulmonary vein and empties into the left atrium.
- When sufficient blood is gathered here, producing sufficient pressure on the mitral valve, the mitral valve opens.
- Blood flows from the left atrium into the left ventricle via the mitral valve.
- When the left ventricle is full of blood, the pressure of this blood pushes back on them mitral valve, forcing it closed and protecting against backward blood flow into the atria while the ventricle contracts.
- As the ventricle contracts, blood is propelled into the aorta via the aortic valve where it then travels into the veins and onwards to complete its journey to the cells of the body.
Two Circuits
You may have worked out by now that this system is essentially two interconnected (closed) circuits. These two circuits are arranged in a series, with the output of one being the input of the other. When we talk about blood flow through the heart, to be specific the two pathways involved ( blood in and blood out of the heart essentially) are referred two as either one of two 'circuits'.
- The pulmonary circuit: The term pulmonary refers to the lungs so that gives us a little clue.
- The systemic circuit: Systemic, think system, whole body circuit.
When working in the world of fitness, these two circuits are of physiological importance therefore it is of great value that you become familiar with these. Let's look at these in more detail.
Whole-body blood flow
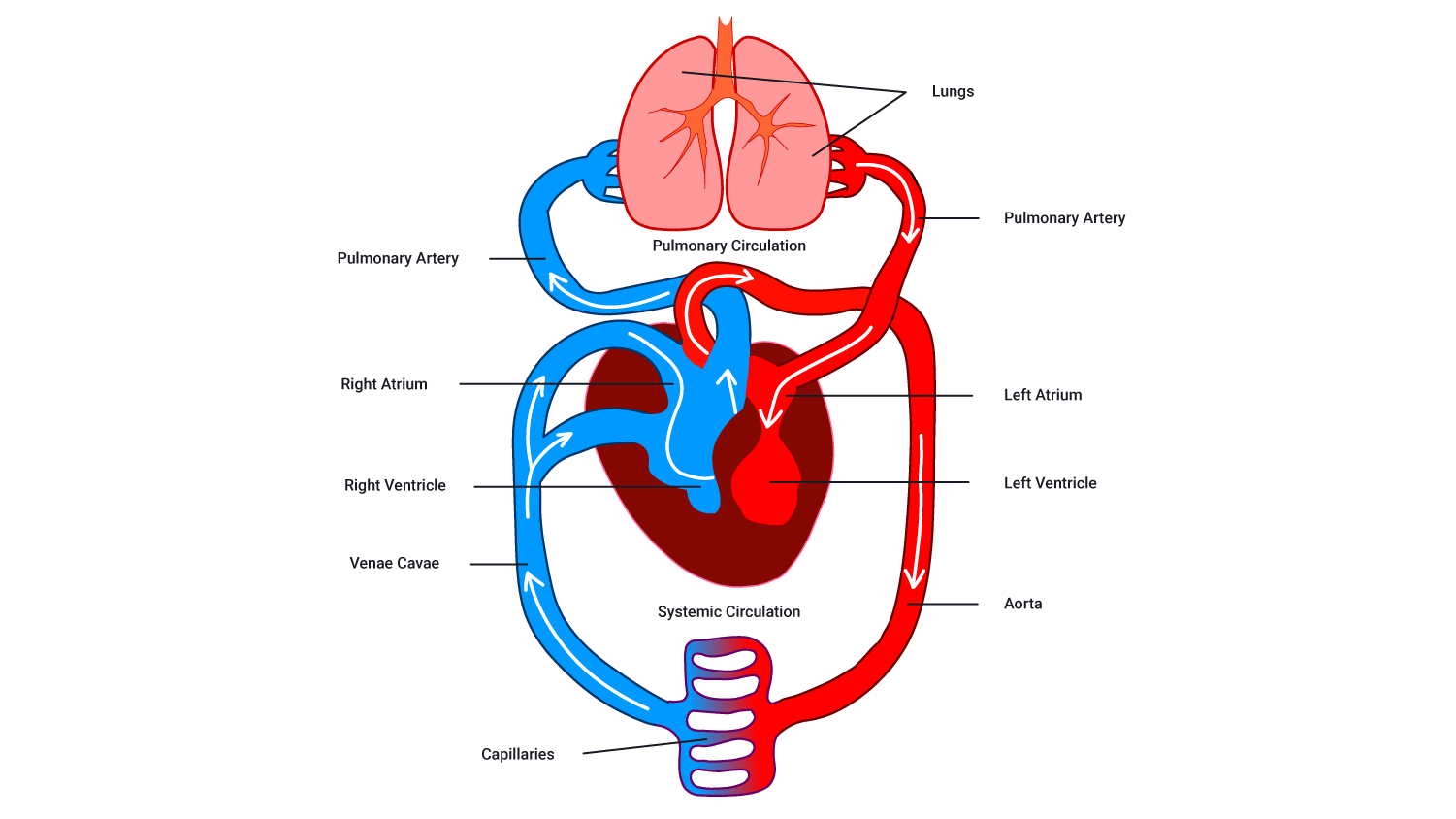
The pulmonary circuit
- The pulmonary circuit receives deoxygenated blood from the superior and inferior vena cava (large veins).
- Blood moves from the right atrium into the right ventricle and is pumped up through the pulmonary trunk.
- Blood then divides to enter the left and right pulmonary arteries (which deliver blood to the left and right lungs respectively).
- Blood flows through the pulmonary arteries which branch into smaller vessels called arterioles and again into capillaries (the smallest outward vessels).
- Capillaries deliver blood to the alveoli of the lungs where carbon dioxide and oxygen are exchanged. Capillaries (receiving oxygenated blood) unite into venules and then transfer blood into veins.
- The oxygenated blood flows back to the left side of the heart via the left and right pulmonary veins.
There are two key structures involved in the pulmonary system:
- The heart: Right atrium, right ventricle, and pulmonary trunk.
- Blood vessels: Pulmonary arteries, arterioles and capillaries, pulmonary venues, and veins.
The systemic circuit
- The systemic circuit receives oxygenated blood (from the pulmonary veins) which flows into the left atrium and moves into the left ventricle.
- The ventricle pumps the oxygenated blood up into a large artery known as the aorta (top of the heart).
- The blood is then supplied to all body regions and organs via systemic arteries, arterioles, and capillaries.
- Nutrients and oxygen are exchanged with CO2 and other wastes.
- Systemic capillaries unite with venules (which start the process of bringing deoxygenated blood back to the heart).
- Deoxygenated blood returns to the right side of the heart via superior and inferior vena cava and the wh0le process repeats.
There are two key structures involved in the systemic system:
- The heart: The left atrium, left ventricle, and aorta.
- Blood vessels: The systemic arteries, arterioles, and capillaries, along with the systemic venules and veins. Supplies blood to every organ of the body (including the heart and lung tissue).
Now is a great time to have a look at this video, it nicely sums up what we have discussed so far, exhale, take a break, and enjoy the next few minutes.
The following picture is an important one for you to become familiar with. You should be able to identify all the structures on it and the direction of blood flow as it would move through these structures.
Blood distribution at rest
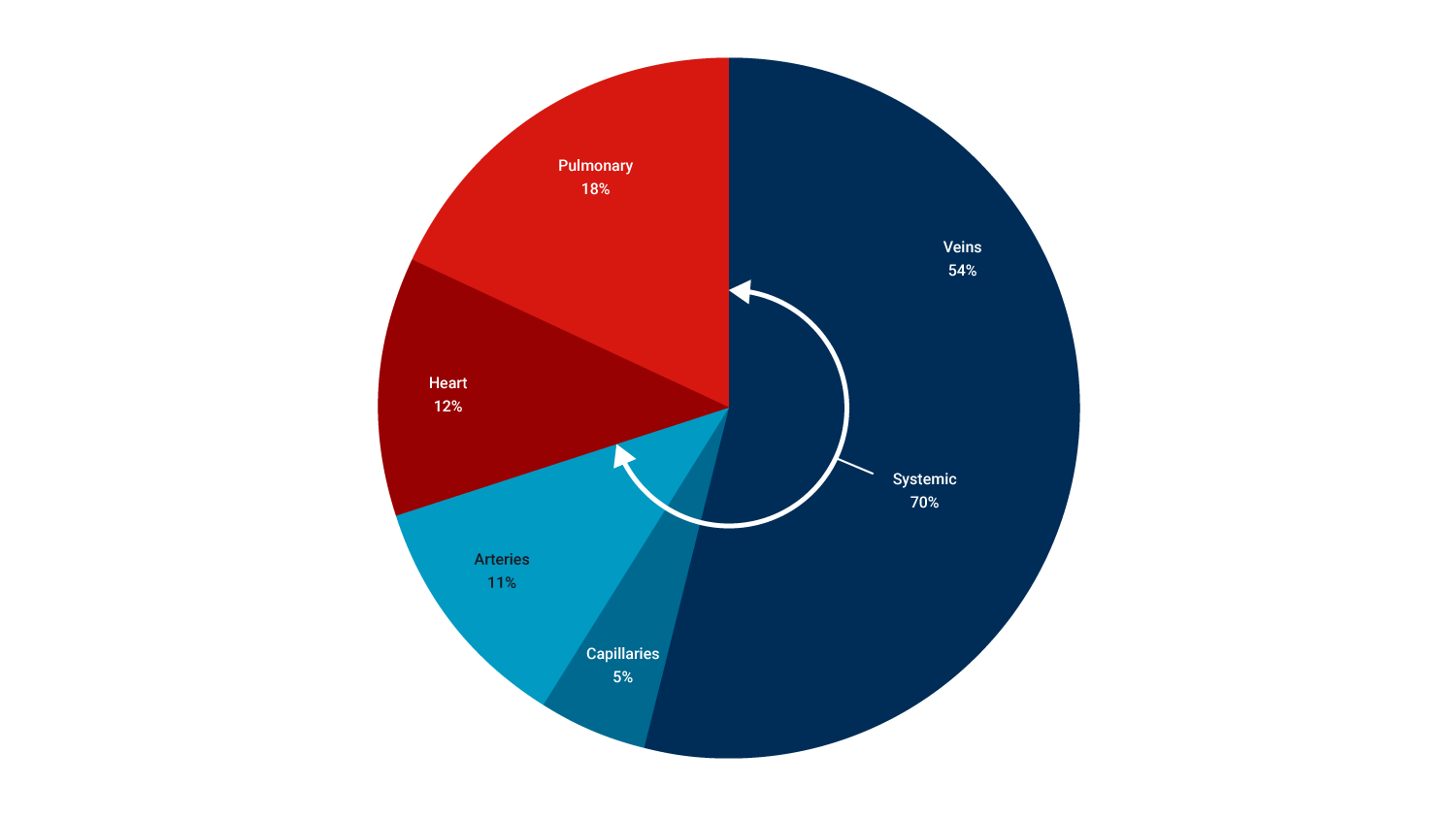
As the pie graph shows, when you are resting, most of the blood in your body is trying to make it back to the heart via veins. The majority of this blood would be in your legs fighting gravity to slowly return. About 30% of your blood is moving to and from the heart and lungs, or being processed by the heart. Only 16% of your blood is heading out to tissues or actively exchanging with cells.
Functions of the blood
Within the human body, our cells can not move around to obtain the oxygen, energy, and nutrients that they require. Therefore, they need a 'friend' to help them and this is the blood. Blood is a liquid connective tissue transporting essential goods such as oxygen, and nutrients to cells for their metabolic processes, and carbon dioxide and other wastes for excretion. This is just one of four general functions.
Homeostasis of fluid balance
To maintain fluid balance, the cardiovascular system works in conjunction with the lymphatic system to remove excess fluid from tissues, passing it to the urinary system for excretion in the urine. This plays a vital role in maintaining blood volume and also the body’s fluid/water balance.
Thermoregulation (temperature control)
This term refers to the homeostatic regulation of the body’s temperature; that is, the mechanisms installed to maintain our body at its optimum temperature of 37.5 degrees Celsius. This is achieved by receptors in the body's skin detecting changes in heat which then either:
- stimulates the muscles to produce heat should our temperature fall below our optimum
- should our temperature rise, the blood then carries heat to the skin's surface via the sweat glands allowing our body to cool (think of flushed cheeks after running).
In order to achieve this, our blood vessels need to expand to accommodate the increased volume of blood travelling through them. This expansion is referred to as vasodilation (dilation of vessels) and in turn, our heart rate typically increases to speed up the journey of the blood to the skin and sweat glands.
Alternatively, vasoconstriction, when our vessels constrict (become narrower) when we are cold in order to assist in retaining heat.
Protection
Our blood plays a huge role in protection. If you think about a time where you have cut yourself, the blood stops when a clot forms, thanks to the platelets in our blood. Thanks to the gel-like properties of blood, the plug type function prevents severe blood loss form our body. Excess blood loss can result in conditions such as shock which can, in worst-case scenarios lead to full body shut down and death. Therefore the clot-forming properties of blood are vital in preventing large volumes of blood loss.
In addition to this, the individual components of blood (which we shall look at a little later) also play a role in protection. The white blood cells prevent disease by identifying any 'nasties' and remove them by breaking them down and then carrying them away in the blood for removal. As discussed above, the blood also transports heat for elimination from our bodies.
Transportation
Our blood is a very important 'courier' of vital nutrients and disposing of waste products. Blood is the sole distributor of oxygen in our bodies. Oxygen binds to hemoglobin and is transported from the lungs to the tissues in the body and picks up carbon dioxide (a waste product) from the tissues. It then delivers it to the lungs for exhalation and removal from the body.
Blood carries nutrients (from our gastrointestinal tract) and hormones (from the glands) to the body cells. Blood also carries wastes to the kidney and liver for detoxification and removal. Finally, blood carries heat to the skin.
Structure of blood
Blood
The medium by which vital gases, nutrients, hormones, and other factors are transported around the human body.
This short video explains the components of blood and their functions:
Components of blood
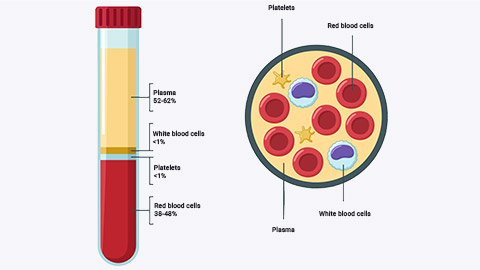
Composed of two principal components:
- Plasma: A watery straw coloured liquid containing:
- ions
- proteins
- hormones.
- Cells
- red blood cells (erythrocytes) which contain hemoglobin (O2 carrying)
- platelets (thrombocytes) which cause blood clotting
- white blood cells (leukocytes) which prevent infection.
The proportion of blood made up of cells is known as hematocrit. An average college-aged male has a hematocrit level of approximately 42%. An average college-aged female has a hematocrit level of approximately 38%. Hematocrit is largely determined by red blood cell numbers.
Blood pressure
This refers to the force exerted by circulating blood on the walls of blood vessels during the heart contraction cycle (both contraction and resting phases).
A minimum of blood pressure is required to ensure blood flow to all parts of the body (especially the brain). The term blood pressure generally refers to arterial pressure, that is, the pressure in the larger arteries.
Blood pressure is measured in two parts:
- Systolic BP
- Diastolic BP.
Systolic arterial pressure is maximum pressure reached in the arteries during the ventricular contraction phase of the heartbeat.
Diastolic pressure is the minimum pressure recorded just prior to ventricular contraction (resting phases). It is generally recorded as systolic/diastolic (this means systolic over diastolic). The desirable blood pressure is approximately 120/80 mmHg in adults.
Factors affecting blood pressure
Cardiac output: As an increase in stroke volume (SV) will create a greater contraction of the heart and thus increase pressure in the arteries it feeds.
Peripheral Resistance
This depends on different factors:
- Length of the vessel: Longer vessels take more pressure to push blood through.
- Radius of the vessel: A small change in vessel diameter can have a dramatic impact on resistance! For example, if your vessels become narrower (this may be due to vasoconstriction or cholesterol), blood pressure (BP) will rise.
- Viscosity of the blood: The thicker the blood, the harder the heart has to work to move it, thus BP rises.
Effects of exercise on blood pressure
One of the acute effects of exercise on the body is an increase in systolic blood pressure. Diastolic blood pressure should remain relatively unchanged as it represents the resting phase of the heart cycle.
A chronic effect of endurance exercise is a gradual lowering in BP due to a reduction in sympathetic nervous system activity and reduced peripheral resistance.
The acute effect of strength training on BP is a sharp rise in systolic BP while lifting. This can often can be made worse due to the Valsalva maneuver (this is a long version of what you might do on a plane to pop your ears).
During intense lifting, the glottis may close as you hold your breath. This increases pressure in abdominal and thoracic cavities inhibiting blood return. It can be very dangerous for those with cardiovascular disease, known high blood pressure, or the elderly.
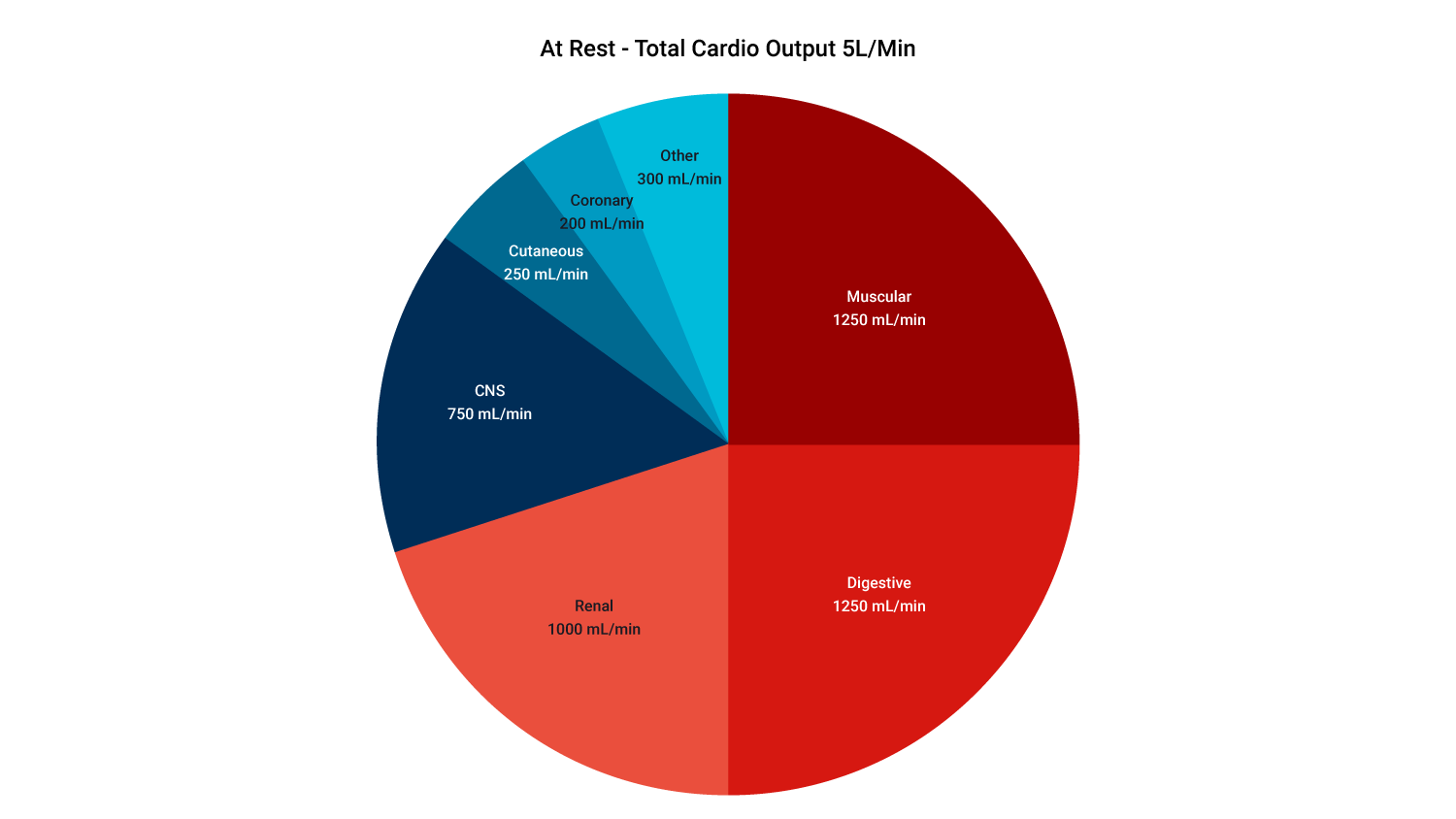
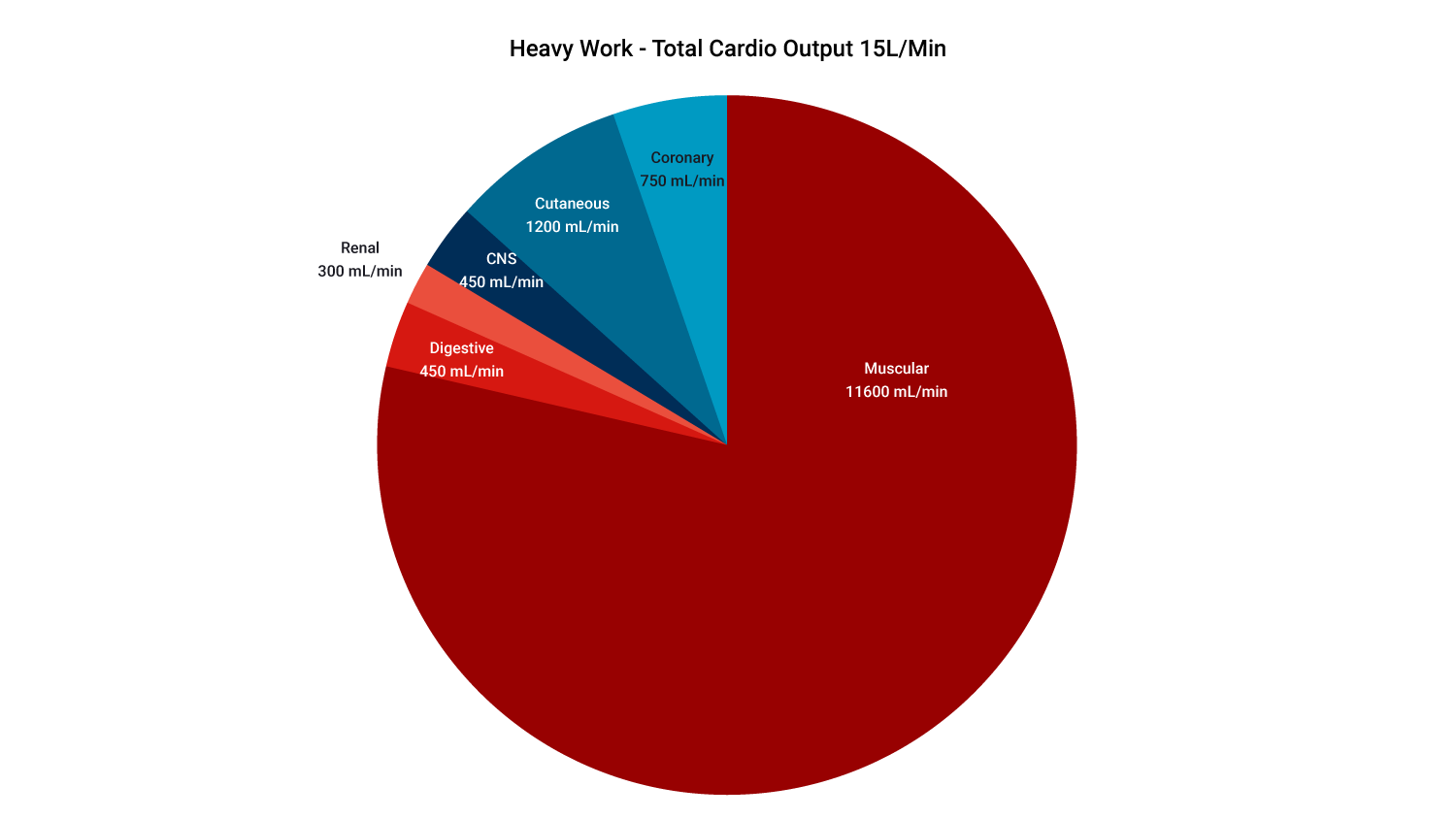
Blood distribution at rest vs during exercise
Beginning exercise, or increasing exercise intensity, usually requires rapid adjustments in blood flow that affect the entire cardiovascular system. The main differences in blood distribution when transitioning from rest to exercise are:
- increased blood flow to working skeletal muscles and skin
- reduced blood flow to less active organs (for example, digestive system)
- at rest 15% - 20% of total Q (cardiac output) goes to muscles (postural)
- during exercise 80% - 85% of total Q (to muscles).
This is illustrated in the following diagrammes:
There are many methods available to assess/determine heart function; some are invasive, requiring invasive technology or instruments which enter the body. Non-invasive techniques exist which is how heart function is determined within a health and fitness environment.
Let's have a look at some calculations below which will aid your program design greatly.
Cardiac output
Cardiac output (Q) is the amount of blood ejected from the left ventricle (to the body) in one minute.
Cardiac output is worked out using the following equation:
Cardiac output (Q)(L/min)= Stroke Volume (SV)(mL/beat) x Heart Rate (HR)(beats/min)
- Heart rate = the number of beats per minute (average 60-85 bpm at rest).
- Stroke volume = amount of blood ejected in each beat (average 70 mls at rest).
At rest, cardiac output is about 5L/min but during max exercise, it can exceed 35L/min!
Example
In a typical adult resting male, stroke volume averages 70mL/beat, heart rate is approximately 75 beats/min, using the equation above:
CO (Q) = SV x HR
CO= 75mL/beat X 70neats/min
CO= 5250mL/min
CO= 5.25 L.min
Why does cardiac output increase during exercise? Cardiac output increases due to:
- increased HR: This is typically a linear increase to max to match increased demands of tissues for blood flow.
- increased SV: This rises initially due to heart stretch as more blood is returned to the heart from working muscles. Plateaus at ~40% VO2max (effort). After this, all increases are due to a rise in HR.
Stroke Volume
The amount of blood pumped from each ventricle in one beat (mls). Governed mainly by three factors:
- Preload: The amount of stretch on the heart, before it contracts (think of a stretched elastic band right before you let it go).
- Contractility: The strength/forcefulness of the contraction.
- Afterload: The blood pressure outside the arteries vs inside the ventricles and heart vessels. As we know, blood flows from an area of high blood pressure to an area of low blood pressure. Therefore it is the balance of these pressures assisting in the speed of blood flow.
During exercise: stroke volume increases due to an increase in venous return (blood flow returning to the heart from working muscles). This leads to a more complete filling of the heart followed by a more forceful ejection and therefore greater stroke volume.
Heart Rate
During exercise: HR increases due to the increased demand for blood flow by working muscles. Muscles require more oxygen and nutrient delivery and more waste removal (heat, CO2).
Newborn infants have higher heart rates (often 120bpm or greater). This is due to smaller stroke volume (and less total blood).
Maximum HR (A.K.A- HRmax or MHR)
This is simply defined as the maximum number of beats your heart can pump per minute under maximum stress.
There are several different methods to calculate MHR we will look at the most popular below.
220 - age (years)
Example, if you were 36 the calculation would be:
HRmax= 220-36
HRmax= 184bpm
Having a grasp on these calculations enables you to design expertly calculated heartbeat based training programs. This will especially relate to cardiovascular training but not specifically, as all exercise has the physiological effect of increasing the heart rate. Therefore, it is important to be aware of which training zone to be focused on reaching when designing a goal-specific program.
Heart rate and exercise
HR increases linearly with exercise intensity up to a maximum- At VO2max HR levels off.
During prolonged exercise: There will be an initial rise in HR which will reach a steady-state after two to three minutes, if the intensity is constant and at a sub-maximal level.
A chronic effect of exercise is a decrease in HR at any given exercise intensity.
Cardiac output and exercise
| Subject | HR (bpm) | SV (ml)/strong> | Q (L/min) |
|---|---|---|---|
| *REST | |||
| Untrained male | 72 | 70 | 5.00 |
| Untrained female | 75 | 60 | 4.50 |
| Trained male | 50 | 100 | 5.00 |
| Trained female | 55 | 80 | 4.50 |
The table above shows that while untrained and trained males of the same size require the same amount of blood (Q=5L/min), they get it in different ways. Note that the trained male achieves his 5L/min with a much lower resting heart rate. This is due to having a much stronger heart, capable of ejecting more blood per beat higher SV. The same is also true of females.
| Subject | HR (bpm) | SV (ml) | Q (L/min) |
|---|---|---|---|
| *MAX EXERCISE | |||
| Untrained male | 200 | 110 | 22.0 |
| Untrained female | 200 | 90 | 18.0 |
| Trained male | 190 | 180 | 34.2 |
| Trained female | 190 | 125 | 23.9 |
The table above shows that a major advantage of being fit is when working at high intensities you can deliver far more blood to working muscles (34L compared to 22L in fit vs unfit males). This is a huge advantage allowing you to deliver more oxygen and fuel to working muscles, and crucially, to be able to remove waste more effectively, so you can maintain higher intensities for longer. The same is true in females but to a lesser extent. This is mainly due to them having a slightly smaller heart to body size ratio.
During prolonged exercise:
- Q (CO) stays the same
- HR increases
- SV decreases.
SV decreases due to loss of sweat causing a dehydration effect as blood plasma is lost in sweat (unless rehydration is adequate). This means less blood is returned to the heart causing a lower SV. HR must climb to compensate.
This is even more pronounced in warm conditions and is known as 'cardiovascular drift'.
Heart Rate Reserve (HRR) and training zones
The Karvonen Formula
The Karvonen method, also known as the heart rate reserve (HRR) formula, takes your resting heart rate into consideration and analyses the difference between this and your maximum heart rate in order to calculate what is known as your 'Heart Rate Reserve' in accordance to calculating individualised target heart rate parameters, for example, 60% max intensity.
In short, the heart rate reserve is the sum of the difference between your maximum heart rate and your resting heart rate. To produce a more accurate calculation, your resting heart rate should be calculated as the average sum of three consecutive readings, (ideally three mornings in a row directly after getting up out of bed). This is not always possible in a gym setting, so to avoid sending your clients home three days in a row, simply measure three consecutive readings.
Target Heart Rate = [(max HR − resting HR) × %Intensity] + resting HR
For example, a 36-year-old female with a resting heart rate of 56 bpm wishing to work out at 60% of her maximum capacity would need to be working at...
Lets pause and look at the math, according to the equation above, this lady would begin to look like this:
Target Heart Rate = [(220-36) − 56) × %0.6] + 56
Target Heart Rate = [184 − 56) × %0.6] + 56
Target Heart Rate = [128 × %0.6] + 56
Target Heart Rate = [76.8] + 56
Target Heart Rate: 60%= 132.8 bpm ( 133 bpm)
Generally, the rough rule of thumb for a guide to training zones would consider the flowing a guide to training intensities:
- Moderate training intensity to be approximately: 50%-70% MHR.
- Vigorous exercise intensity: 70%-85% MHR.
Watch this brief yet informative video for an overview of the Karvonen method. This will be used frequently within your training program design so it is important to become familiar with it.
In this topic, we focused on the structure and function of the components of the cardiovascular system. You learnt about:
- an overview of the cardiovascular system
- structure and function of the cardiovascular system, including heart, blood and blood vessels
- circulatory system of the blood
- structure and function of blood
- physiology of blood pressure
- measurements of heart function.
Congratulations for processing a lot of information in this topic, take a short break to complete the final activity for this topic.

