In this topic, we focus on the structure and function of the components and mechanics of the respiratory system. You will learn:
- an overview of the structure and function of the respiratory system
- the structure and divisions of the respiratory system (for example, upper and lower conduction respiratory zones)
- respiratory system structures and their functions
- the mechanics of breathing (muscles of respiration, pressure differences)
- gas exchange and transportation (O2 and Hb, CO2 and Mb)
- measurements of respiration (lung volumes and capacities and their calculations)
- exercise and its effects on respiration (receptors involved in ventilation).
Terminology and vocabulary reference guide
As an allied health professional, you need to be familiar with terms associated with basic exercise principles and use the terms correctly (and confidently) with clients, your colleagues, and other allied health professionals. You will be introduced to many terms and definitions. Add any unfamiliar terms to your own vocabulary reference guide.
Activities
There are activities throughout the topic and an end of topic automated quiz. These are not part of your assessment but will provide practical experience that will help you in your work and help you prepare for your formal assessment.
Function
The respiratory system provides oxygen for cellular metabolism and removes waste. The respiratory system contributes to the maintenance of homeostasis by providing a method of gas exchange between the atmospheric are and the cells of the tissues. This requires the synchronisation between all the components of the respiratory system. We will look at the different structural components of the respiratory system throughout this topic. Let’s begin with an overview of the mechanics behind the function, that is, how does it do what it does?
Mechanics of function
- Step 1: Inhalation (breathing in) occurs. Breathing in results in oxygen-rich air being drawn into the lungs.
- Step 2: Gas exchange occurs. This is an exchange of gases between air and blood and between the blood (haemoglobin) and tissue.
- Step 3: O2 transport. Blood carries O2 from the lungs to the organs of the body. Oxygen binds to the haemoglobin molecules which then transport the oxygen around the body.
- Step 4: Waste Collection. Blood carries CO2 back to the lungs to be expelled.
- Step 5: Exhalation (breathing out) occurs. This enables CO2 (a waste material form cellular metabolism) to be expelled from the body. Co2 can become toxic when levels become high enough therefore its removal is essential.
- Step 6: Repeat step 1.

Your body’s cells continually use oxygen for the metabolic reactions which they conduct; nerve transmission, cell to cell communication, muscle contraction, and many more. This means that oxygen is constantly in high demand.
When something is 'used' there is generally a waste product, the bits that aren’t fully needed. In the case of metabolic reactions and the respiratory system, this waste product is carbon dioxide (CO2). CO2 can become toxic to the cells of the body when present at high levels. Therefore, as well as supplying our cells with oxygen, the equally important role of the respiratory system is to remove carbon dioxide.
Fun fact: This process is one of many processes in the human body which require the combination of more than one body system. In this case, the removal of carbon dioxide and uptake of oxygen cannot be fully conducted without the support of the cardiovascular system. The lungs and additional respiratory structures do indeed inhale oxygen and exhale carbon dioxide; however, these cannot be transported to and from the cells of the tissues without the support of the heart, blood, and blood vessels (the cardiovascular system).
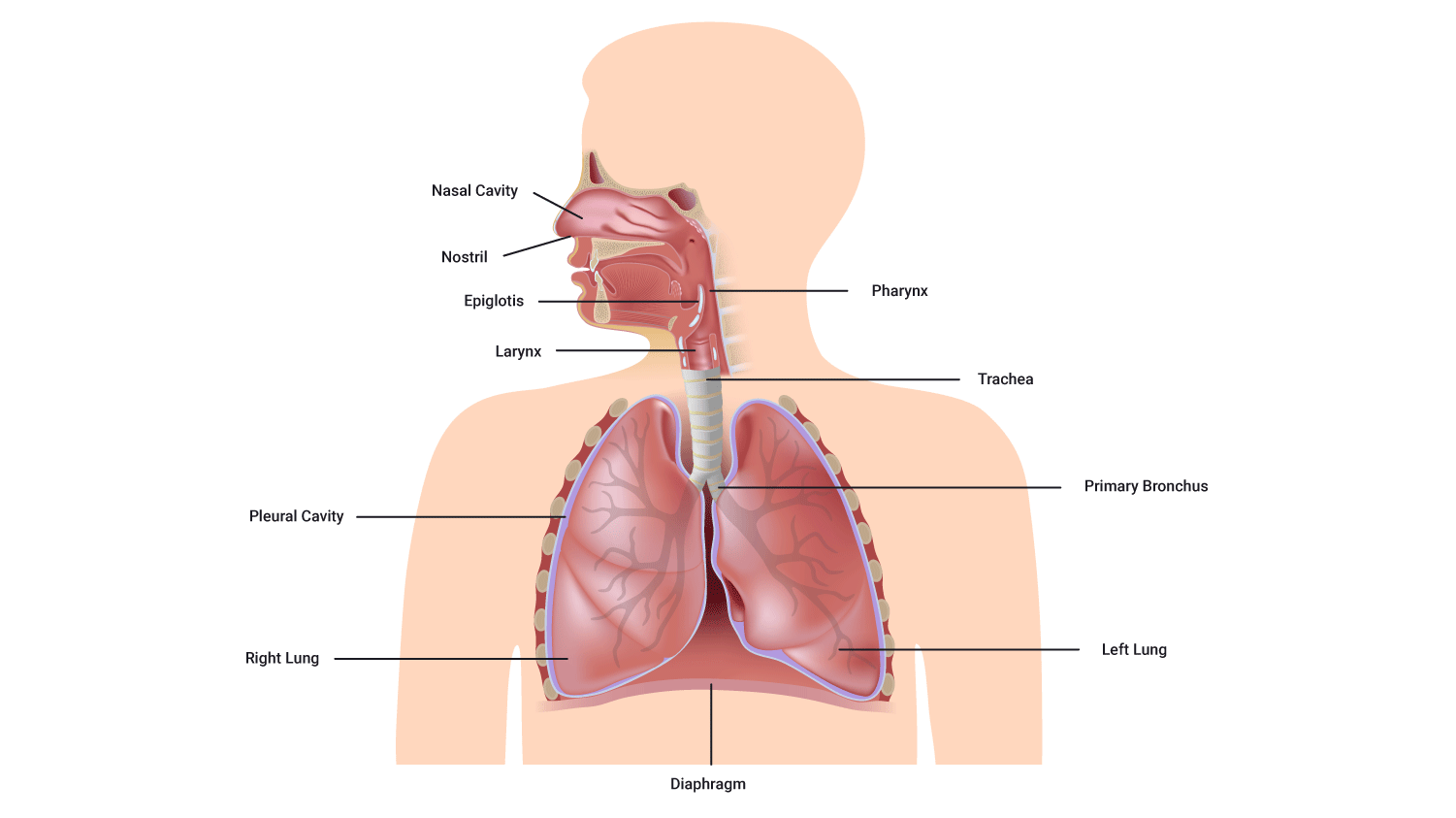
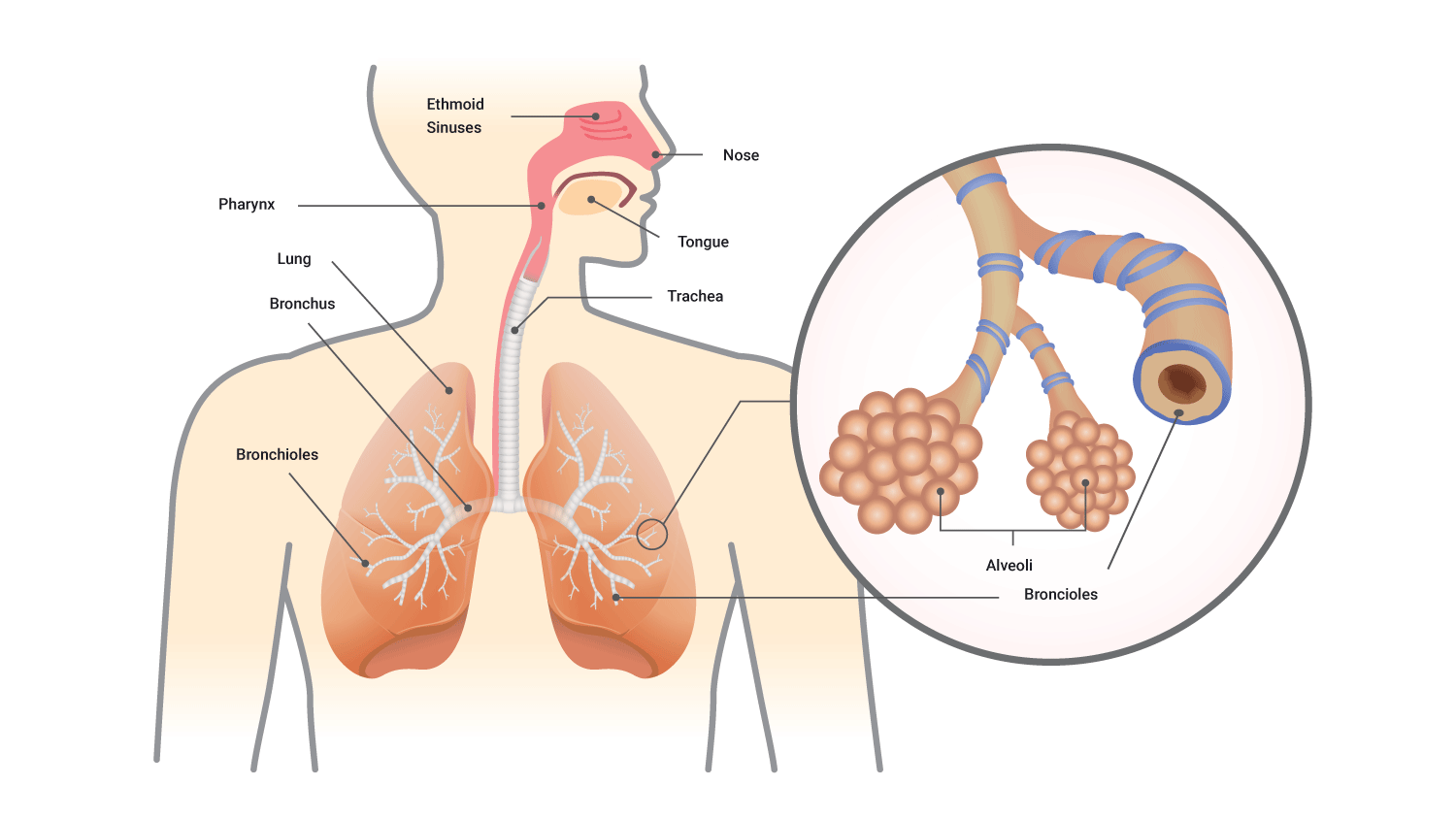
As a whole, the respiratory system is comprised of the:
- nose
- pharynx (throat)
- larynx (voice box)
- trachea (windpipe)
- bronchi (tubular branches which lead to the lungs)
- lungs.
However, in anatomy and physiology, because subdividing things seems really enjoyable and structure mirrors function, so the respiratory system can be classified both structurally and functionally. It is important that you are comfortable with both classifications and the structures with these divisions as well as their function. Let’s take a closer look at these.
Classifications of the respiratory system
Structural classification of the respiratory system
Structurally the respiratory system consists of two parts (based on their structural location). These are referred to as the upper respiratory system and the lower respiratory system.
- The upper respiratory system
- Nose
- Nasal cavity
- Pharynx
- Associated structures (for example, glands, hairs).
- The lower respiratory system
- Larynx
- Trachea
- Bronchi
- Lungs.
Functional classification of the respiratory system
Functionally, the respiratory system is also subdivided into two parts (based upon what they do). These are referred to as the conducting zone and the respiratory zone.
1. The conducting zone
Structures
- Lungs and their network or tubes both inside and outside of the lungs
- Nose
- Basal cavity
- Pharynx and associated structures.
Function
The function of the conducting zone is kind of like what it sounds like on the tin; the main role of these structures is to conduct the air in. However, they do a lot more than just conduct; they moisten, filter, and also warm the air we breathe in.
2. The respiratory zone
Structures
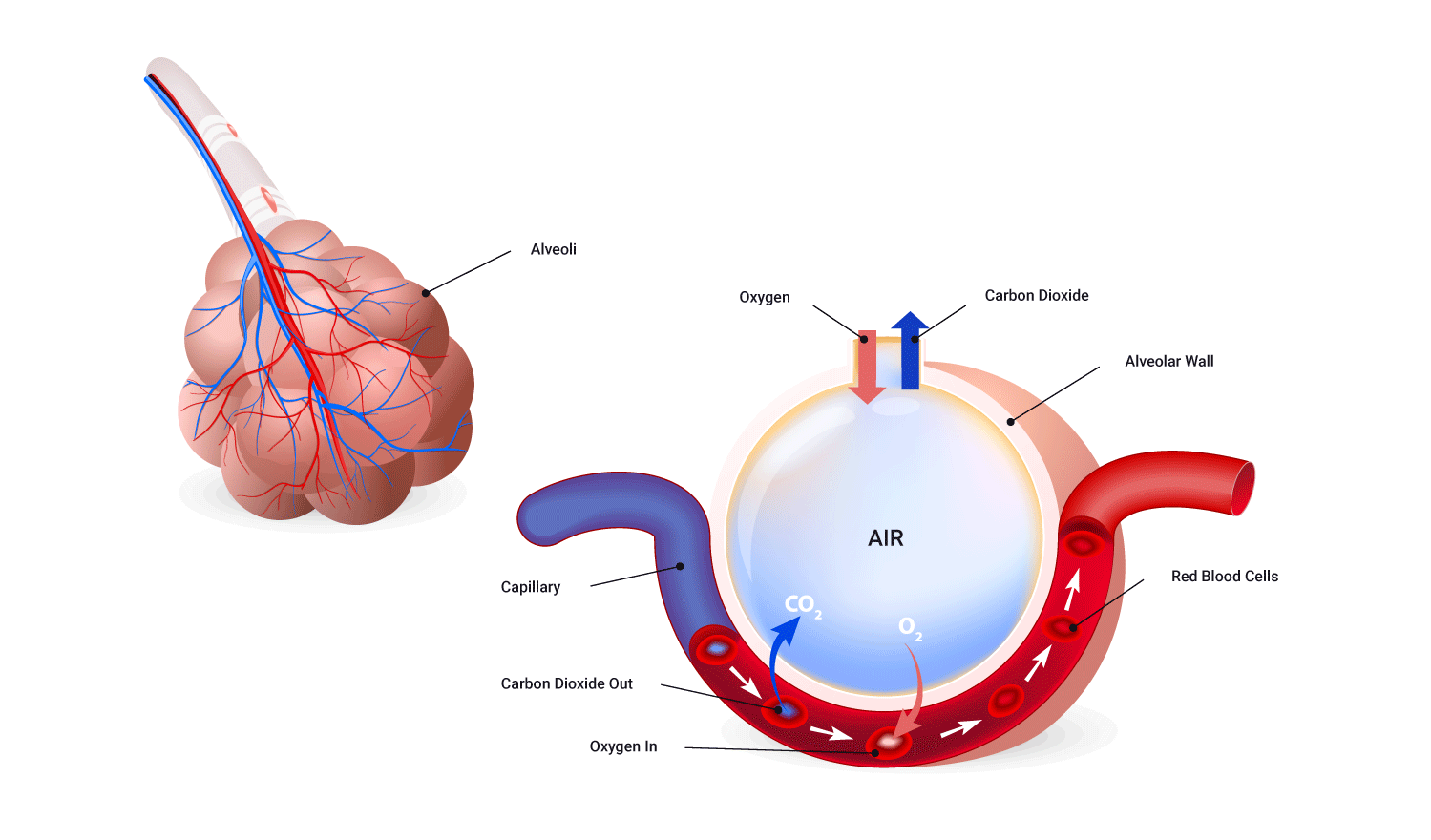
The tubes and tissues within the lungs where gas exchange occurs, include the:
- respiratory bronchioles
- alveolar ducts
- alveolar sacs
- alveoli.
Function
The function of the respiratory zone is to actually take part in/facilitate gas exchange.
Now we are comfortable with the overall function, let’s take a closer look at the structures involved.
We have mentioned all the structures involved in the functions of the respiratory system, but how do they do what they do, and why? Let’s take a look at them individually.
The nose and mouth
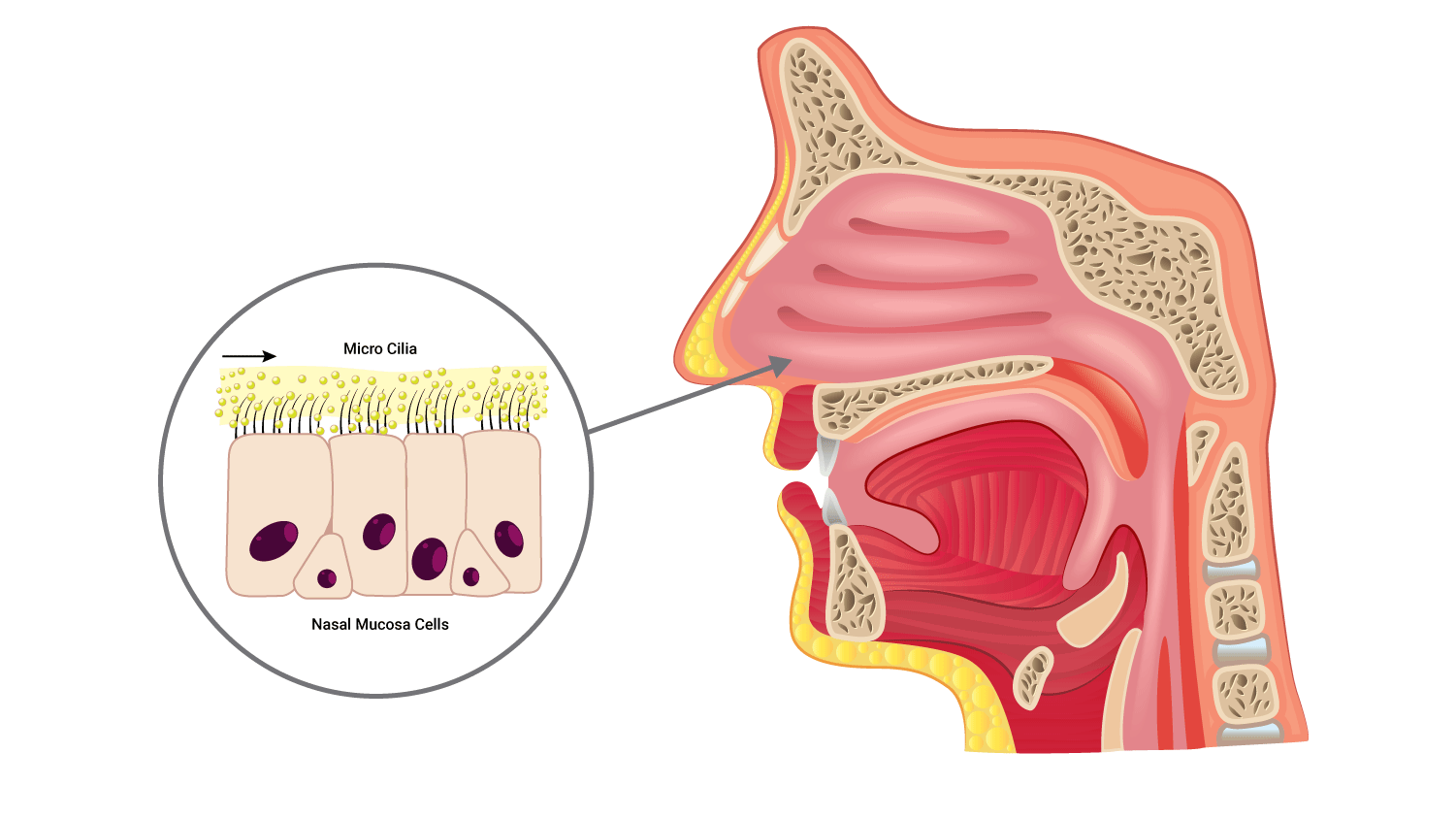
The mouth and nose have several functions pertaining to the respiratory system:
- Filters/cleans inhaled air: These functions are performed by the nasal passage which contains hairs (cilia) which trap unwanted particles. The cells of the nasal passage also produce mucus which is a sticky substance which further aids in filtering inhaled air from foreign particles.
- Detects odours (nose only): These specialised cells in the nose (olfactory sensors) communicate with the brain in order to assist us in detecting odours. It’s tricky to smell when you have a blocked nose.
- Humidifies inhaled air: As air passes through the nose and mouth, droplets of water combine with the air and humidify the air.
- Warms air: As inhaled air swirls around the nasal cavity, it is warmed by the neighbouring blood capillaries. The additional temperature and moisture facilitate a smooth(er) journey of air through the remainder of the respiratory system without drying or temperature 'shocking' them en route.
Much more filtering of inhaled air occurs when we breathe in through our nose. The mouth has far less filtering apparatus to assist in these functions, therefore it is generally recommended to breath in through the nose and out through the mouth.
The pharynx
The pharynx (throat) is:
- a funnel-shaped, muscular tube approximately 13 cm (5 inches) long
- located posteriorly to the nasal and oral cavity and superiorly to the larynx
- composed of skeletal muscle and lined with a mucous producing membrane.
The pharynx can be divided into three anatomical regions called the nasopharynx, the oropharynx and the laryngopharynx.
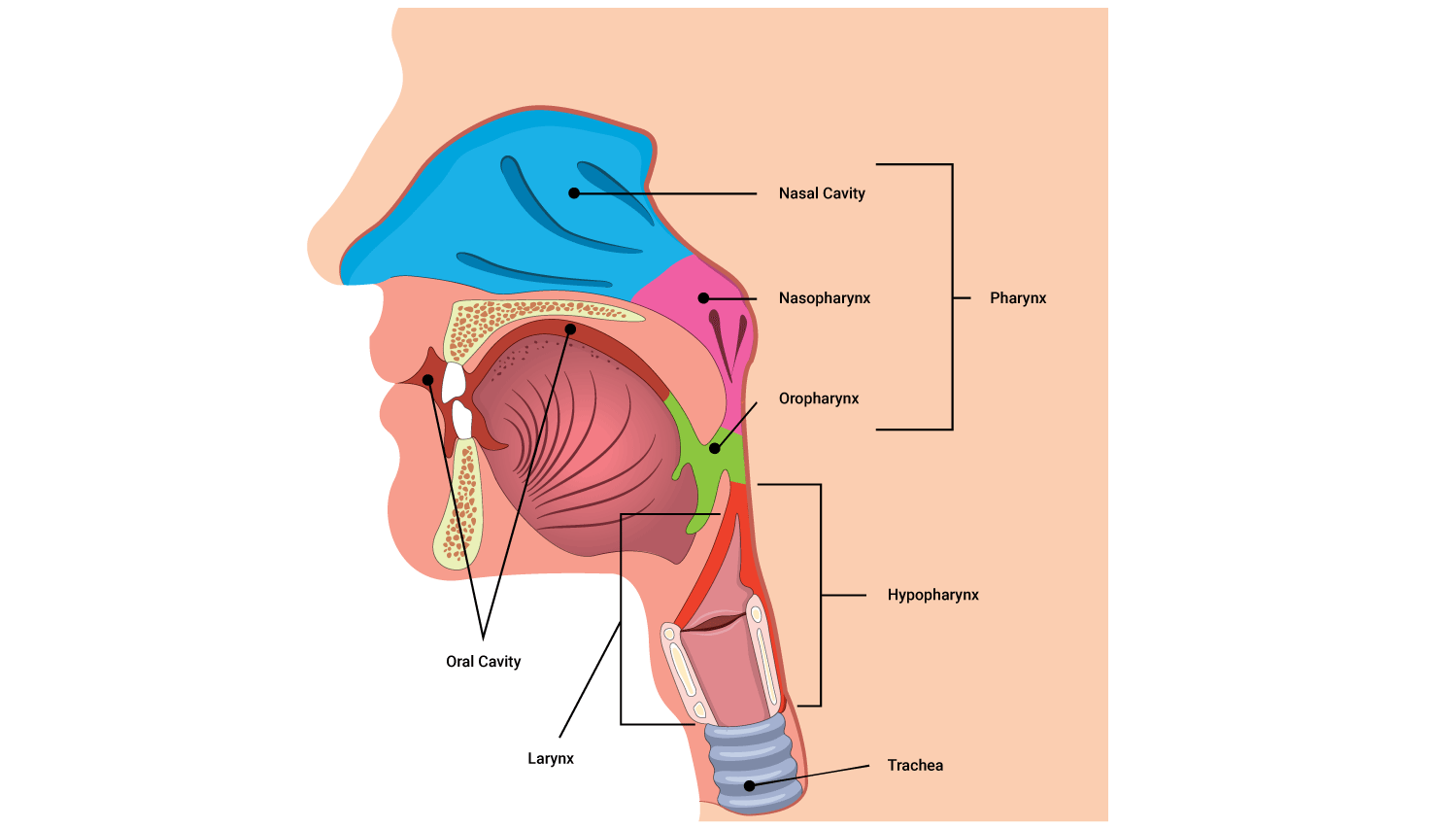
- Nasopharynx: The mucous and cilia (little hairs) help trap particles entering the respiratory system. The nasopharynx also exchanges a small amount of air with the auditory tubes which aid in equalising air pressure, think of this next time you 'pop your ears'.
- Oropharynx: This portion of the pharynx have both respiratory and digestive functions. It is a common passageway for air, food and drink. We also find the tonsils within this region of the pharynx.
- Laryngopharynx: The most inferior portion of the pharynx (also referred to as hypopharynx due to its location). Similar to the oropharynx, this region also has both digestive and respiratory functions because it connects with both the larynx (voice box) and the oesophagus (food tube). This portion aids in swallowing.
The larynx
The larynx also referred to as the 'voice box' is a short passageway which connects the pharynx (via the laryngopharynx) to the trachea (windpipe). The main function of the larynx is to produce our sounds; structural changes which occur during sound production, enable different pitches and tones to be produced.
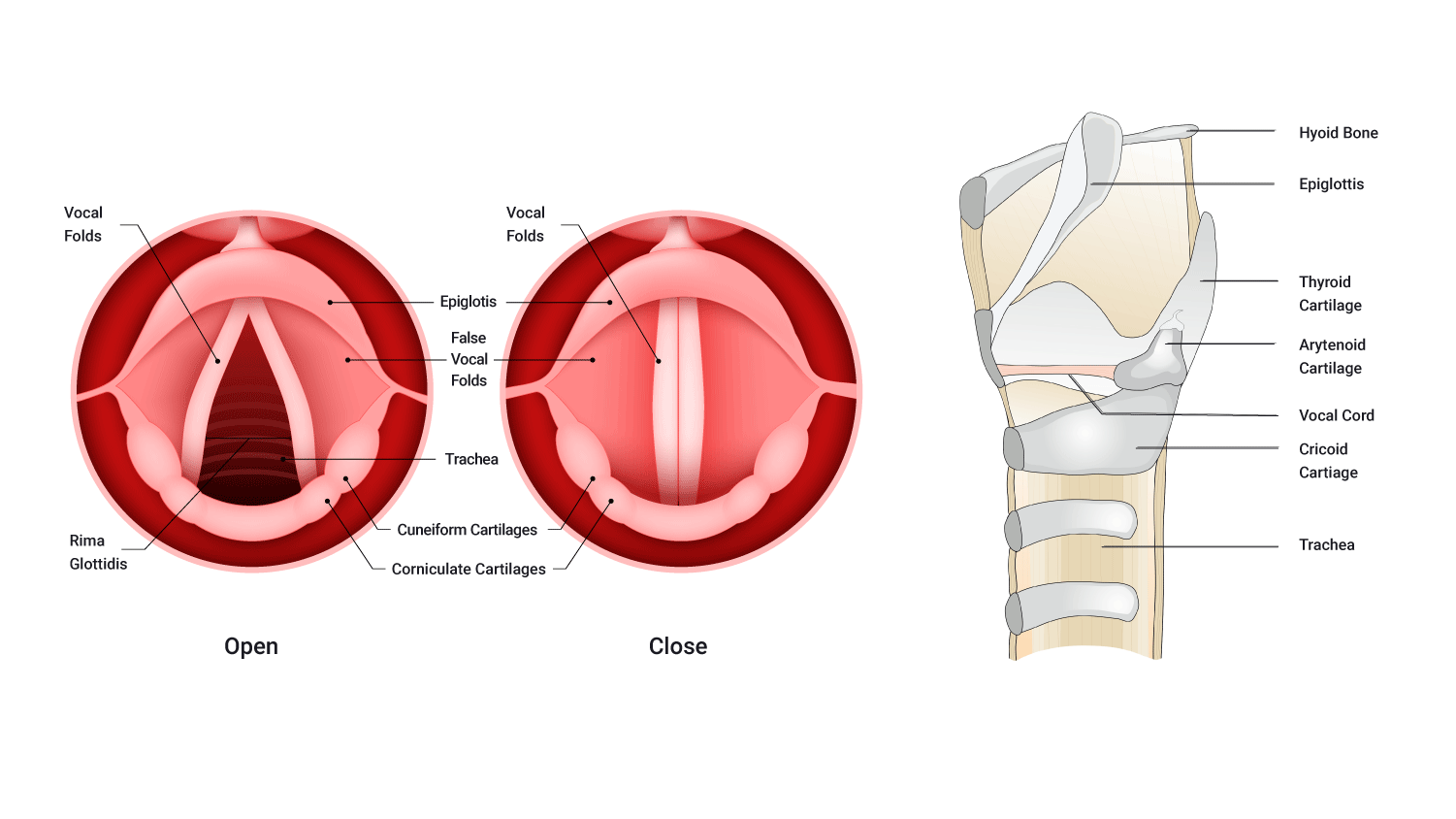
The larynx also plays a key role in the transit of food and drink and acts as a form of a security guard. A structure, known as the epiglottis (found within the larynx) can move up and down like a trap door. This action enables food and drink to pass through at an optimum rate and time, ensures food and drink transit on towards the oesophagus, and keeps them from entering the larynx and airways.
The trachea
The trachea also referred to as the 'windpipe' is located anteriorly to the oesophagus. The primary function of the trachea is to deliver air to the lungs.
The trachea is composed of both muscular tissue and connective tissue in the form of cartilage. The shape of the trachea arises from C-shaped rings of hyaline cartilage (like a vacuum cleaner pipe) which enable the trachea to remain open and not collapse on itself. The C-shaped rings accommodate the neighbouring oesophagus in a Tetris-like fashion.
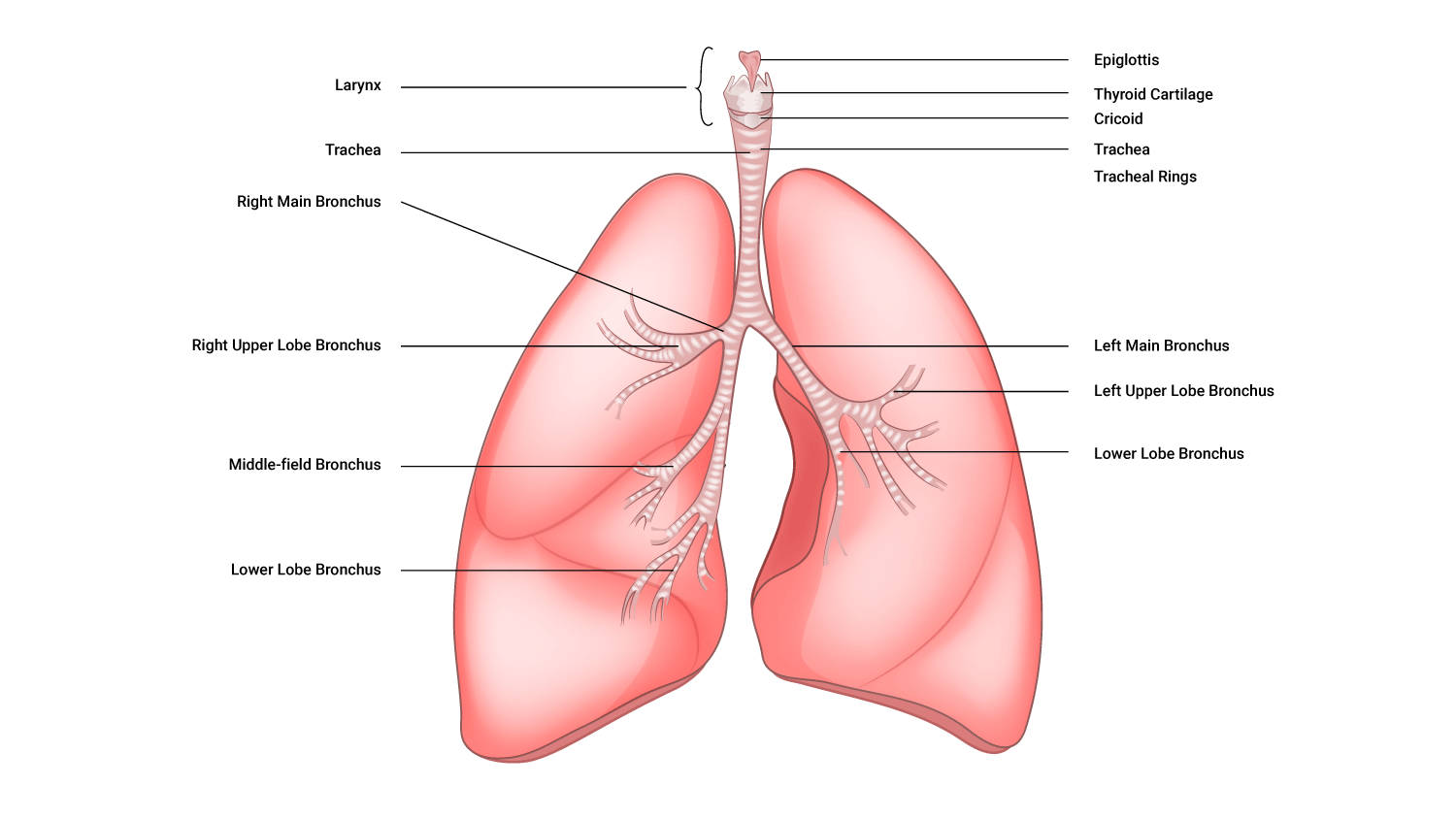
The bronchi
The bronchi are referred to as the 'bronchial tree' because anatomically they represent a tree-like structure with its dense network of attached branches.
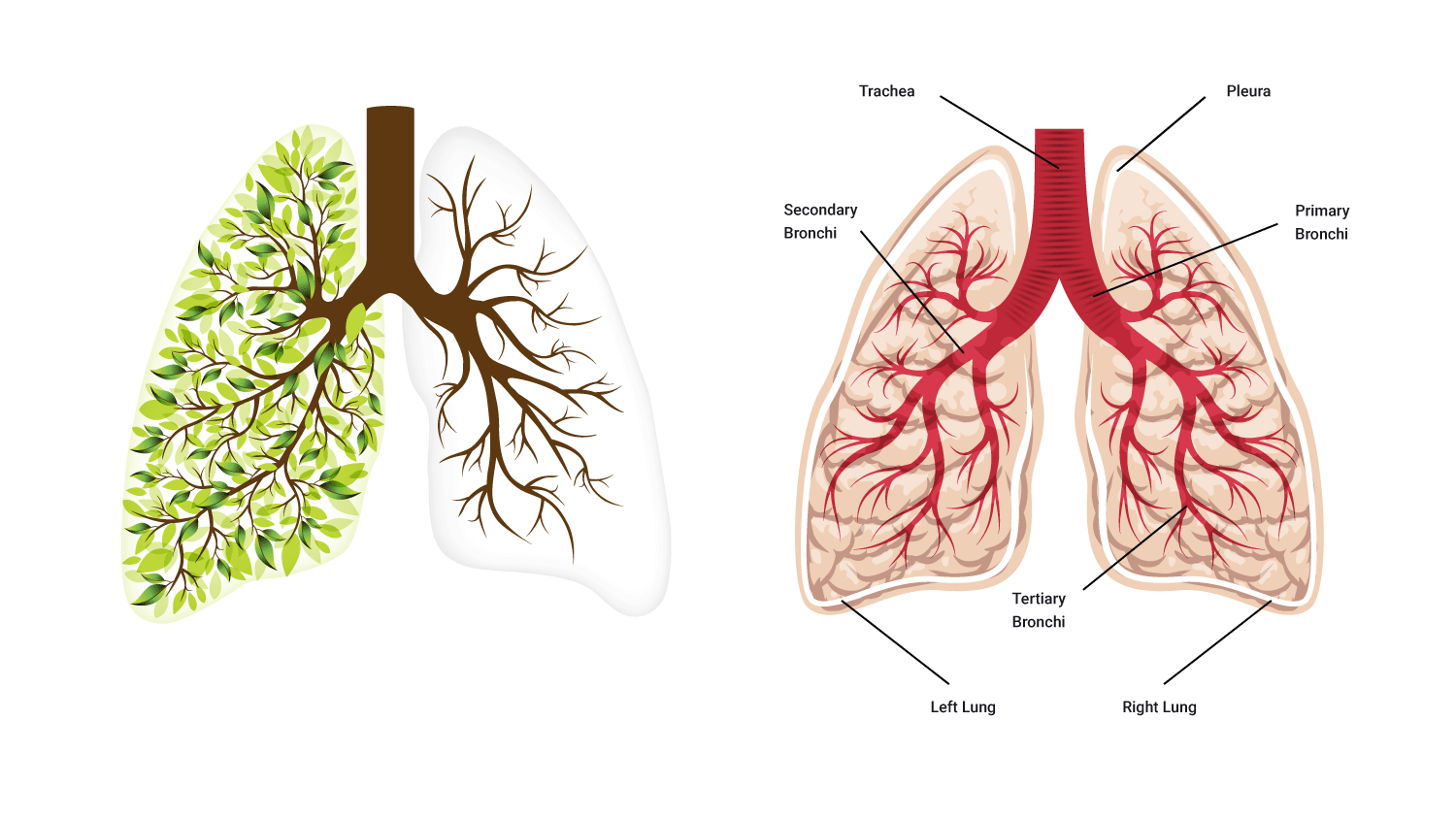
The bronchi are a highly branched system which can be further sub-divided by its tree-like structure. Let’s look at these from superficial to deep to the lungs:
- Primary bronchi: These are the initial portions of the bronchial tree which enter the lungs, the right primary bronchi into the right lung and the left into the left lung.
- Secondary bronchi: The primary bronchi further divide into secondary bronchi. These are smaller and narrower than the primary bronchi however they are greater in number (slightly) with three (3) secondary bronchi in the right lung and two (2) in the left.
- Tertiary bronchi: The secondary bronchi divides and branches into smaller tertiary bronchi which supply a segment within each lobe of each lung.
- Bronchioles: The tertiary bronchi continue to subdivide and branch into smaller vessels referred to as bronchioles (right and left bronchiole)
- Terminal bronchioles: Bronchioles themselves also branch into even smaller tubes referred to as terminal bronchioles. And as the name suggests are the last stop on the bronchial tree; the end of the conducting zone of the respiratory system. Fun fact: There are approximately 65,000 terminal bronchioles in total.
We can, 'unofficially' continue the bronchial tree in a sense as we look at the structures which can be found after the terminal bronchioles. To continue with the subdivision:
- Respiratory bronchioles: Terminal bronchioles then branch into two or more respiratory bronchioles; these then branch off into:
- Alveolar ducts: Each respiratory bronchiole branches off into 2-10 alveolar ducts
- Alveolar sacs: The alveolar ducts end with irregularly shaped sacs named alveolar sacs, holding bunches of alveoli in clusters.
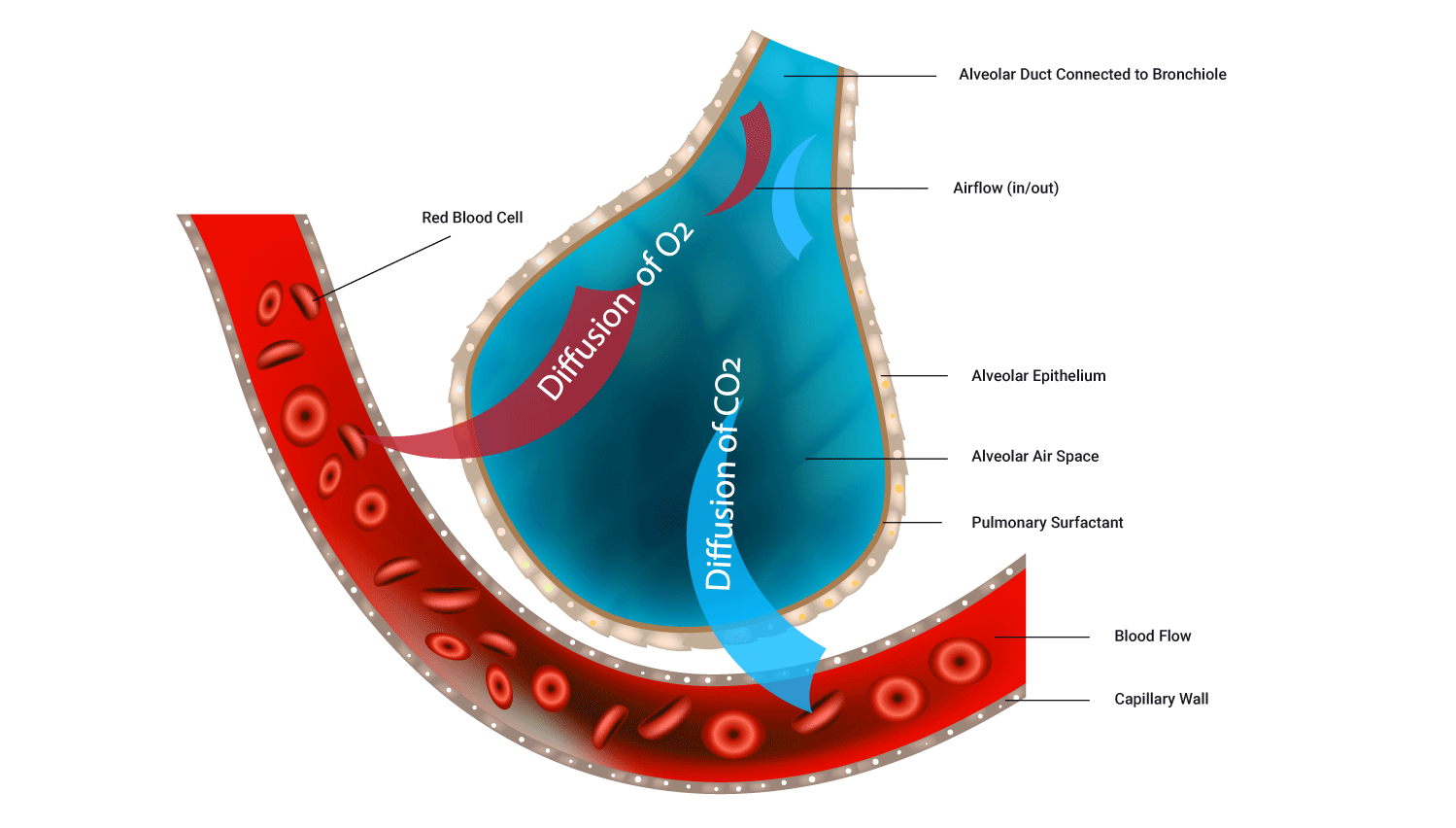
- Alveoli: Each Individual circular/balloon-like structure which is the site for gas exchange with the blood.
The lungs
The right and left lungs are cone-like structures. They are wider at the bottom where they rest onto the diaphragm, and narrower at the top where they form a point in the collarbone region. The part of each lung that rests on the ribs is referred to as the costal surface of the lungs.
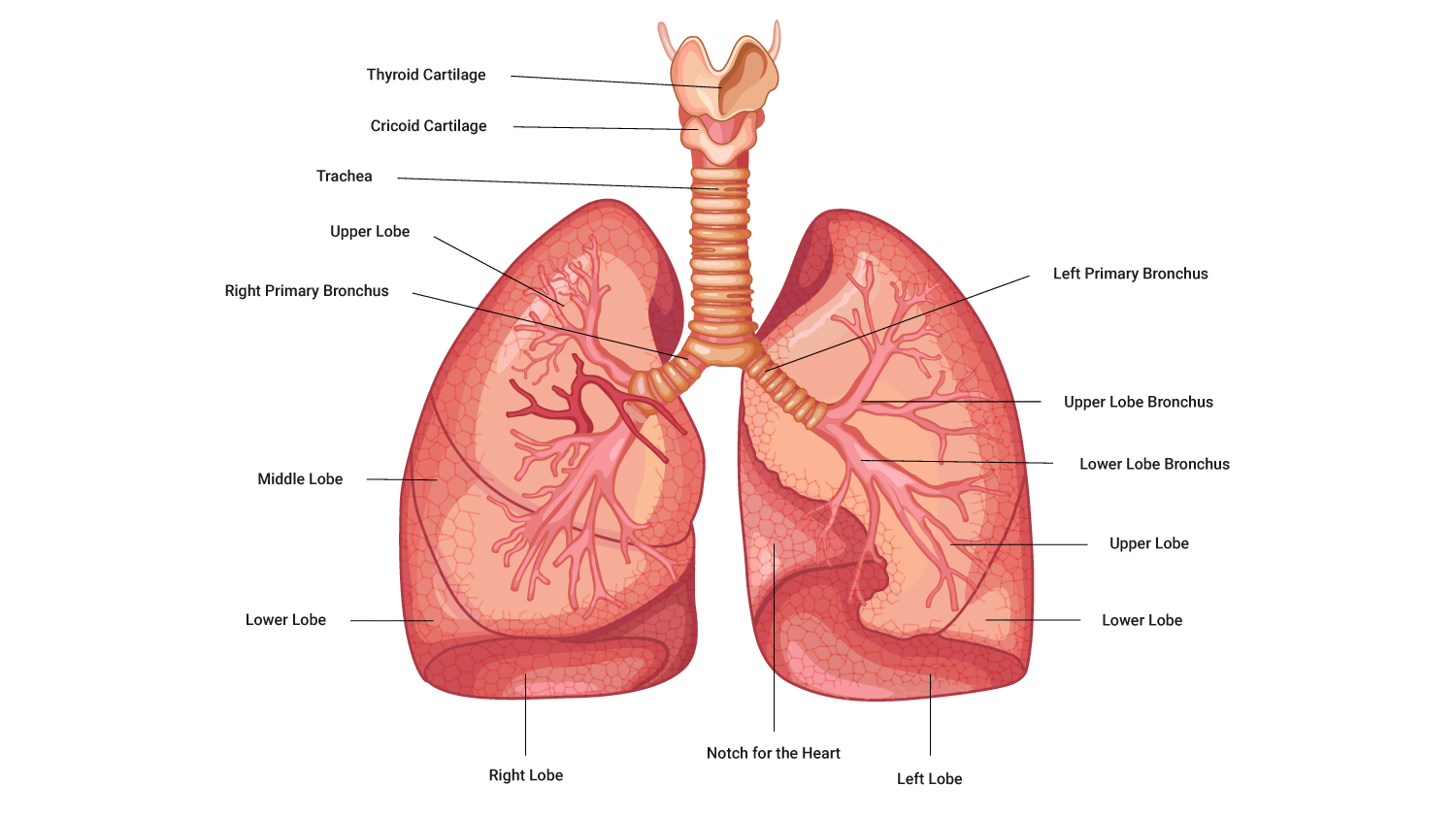
Note that the left and right lungs are structurally different:
- The left lung is slightly smaller than the right:
- this is to accommodate the heart (in a region called the 'cardiac notch')
- the smaller size results in the left lung being composed of two lobes (inferior and superior) and the right of three lobes (inferior, middle and superior).
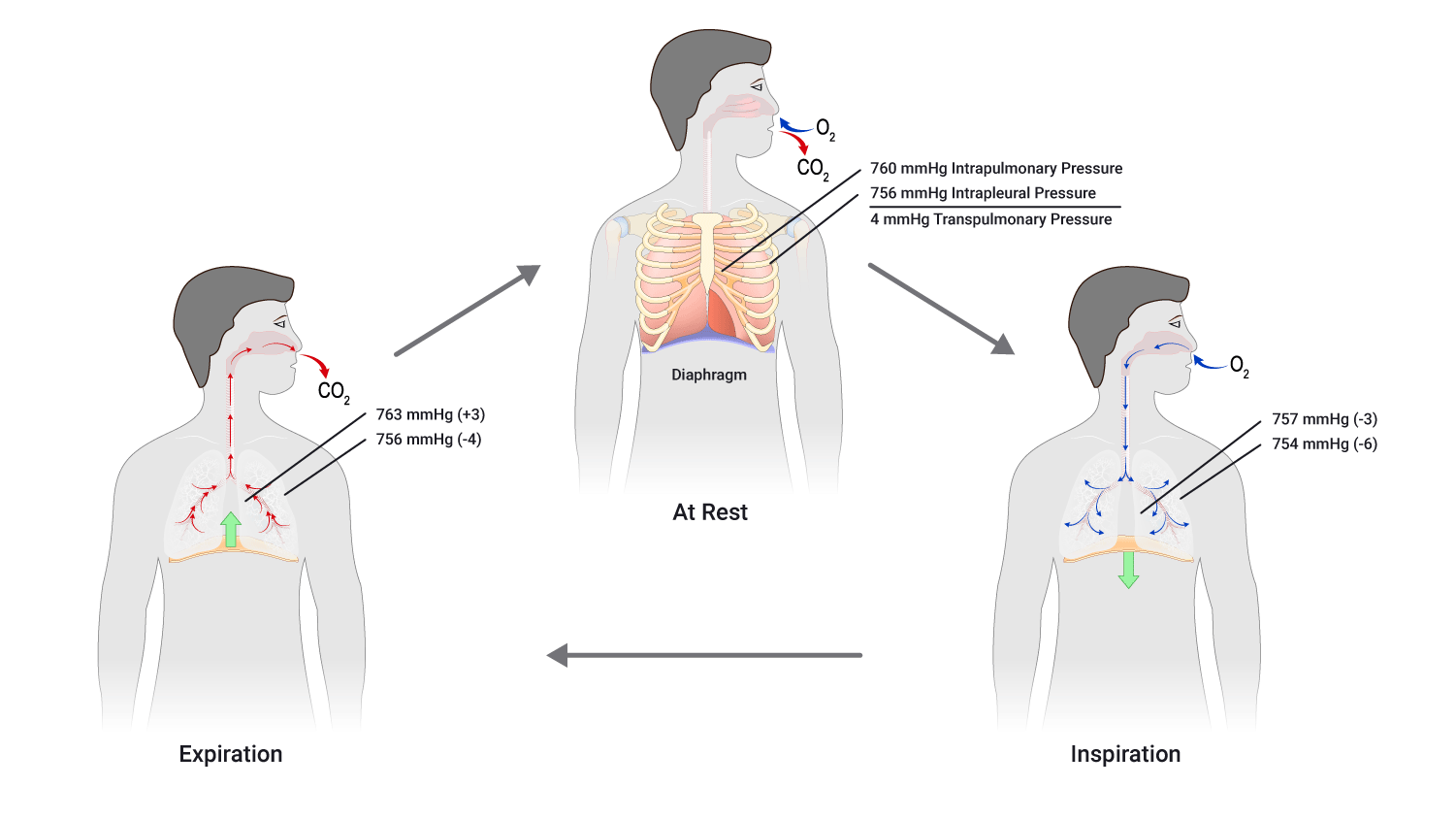
As we know, the lungs are responsible for airflow, however, it is important to note that two aspects are involved in establishing and maintaining airflow:
- Muscular action
- Pressure differences.
The basic rule of airflow is that air will move from an area of high pressure to an area of low pressure (think of a balloon deflating).
Breathing (also known as ventilation) is the mechanism by which we get air in and out of our lungs. The ability to do this relies on the manipulation of pressure.
Respiratory pressures
In the context of the respiratory system, the pressures that are being referred to are the pressure within the lungs versus the pressure of the external atmosphere (atmospheric pressure). Obviously, we do not have the option/possibility to manipulate the atmospheric pressure, but we can manipulate the pressure within our lungs by either increasing or decreasing their size.
Respiratory pressure facts
- To initiate airflow in (inspiration) it is necessary to lower intra-pulmonary pressure below atmospheric pressure.
- Increasing lung volume (space) reduces intra-pulmonary pressure (pressure in the lungs).
- Decreasing lung volume (space) increases intra-pulmonary pressure.
- To initiate airflow out (expiration) it is necessary to raise intra-pulmonary pressure above atmospheric pressure
Atmospheric pressure at sea level is around 760mmHg. In order to draw air into our lungs, we have to reduce the pressure inside the lungs to below 760mmHg. In order to move it out, we need to increase the pressure in the lungs to above 760mmHg.
Let’s take look at the muscles involved in breathing (inhalation and exhalation, as well as forced exhalation).
Muscles involved in breathing: Ventilation
In order to manipulate lung size and therefore pressure inside the lung cavity, we must recruit muscle to assist. The key muscle involved in breathing is the diaphragm which is a flat, dome-shaped muscle that lies beneath the lungs.
Accessory muscles of breathing
The diaphragm is the main muscle of breathing, however, several other muscles also offer their services in certain circumstances. These are referred to as 'accessory muscles of breathing'. These muscles work, in addition to or replacing the diaphragm, should it become injured.
- Abdominal muscles: Rectus abdominis, external/internal obliques, transversus abdominis.
- Internal/external intercostal muscles: These are located between the ribs, they assist in living and expanding the rib cage.
- Scalenes: These run from the neck to the first rib and lift the upper ribs and thoracic cavity around the ribs which in turn affect the pressure within the lungs. They also provide a method for inspiration to continue should the diaphragm be injured and unable to contract normally.
- Trapezius: These muscles are located in the neck/shoulders and retract/pull back the scapula and expand the upper part of the thoracic cavity.
- Sternocleidomastoid: A muscle that is connected to both the neck and the sternum which turns the head. These muscles can also lift the upper ribs, similar to the scalenes.
Mechanics and muscles of inspiration
- The diaphragm drops scalenes (neck muscles), and fixes the first rib in place.
- The external intercostal muscles elevate the rest of the ribs.
- The above actions lead to an increase in lung space, thus reducing the pressure in the lungs below the atmospheric pressure.
- Air flows in from the now higher atmospheric pressure, due to the rule of airflow (from an area of high pressure to an area of low pressure).
- Deep inspiration sees extra muscles recruited to further increase the thoracic cavity (pectoralis minor, sternocleidomastoid, erector spinae).
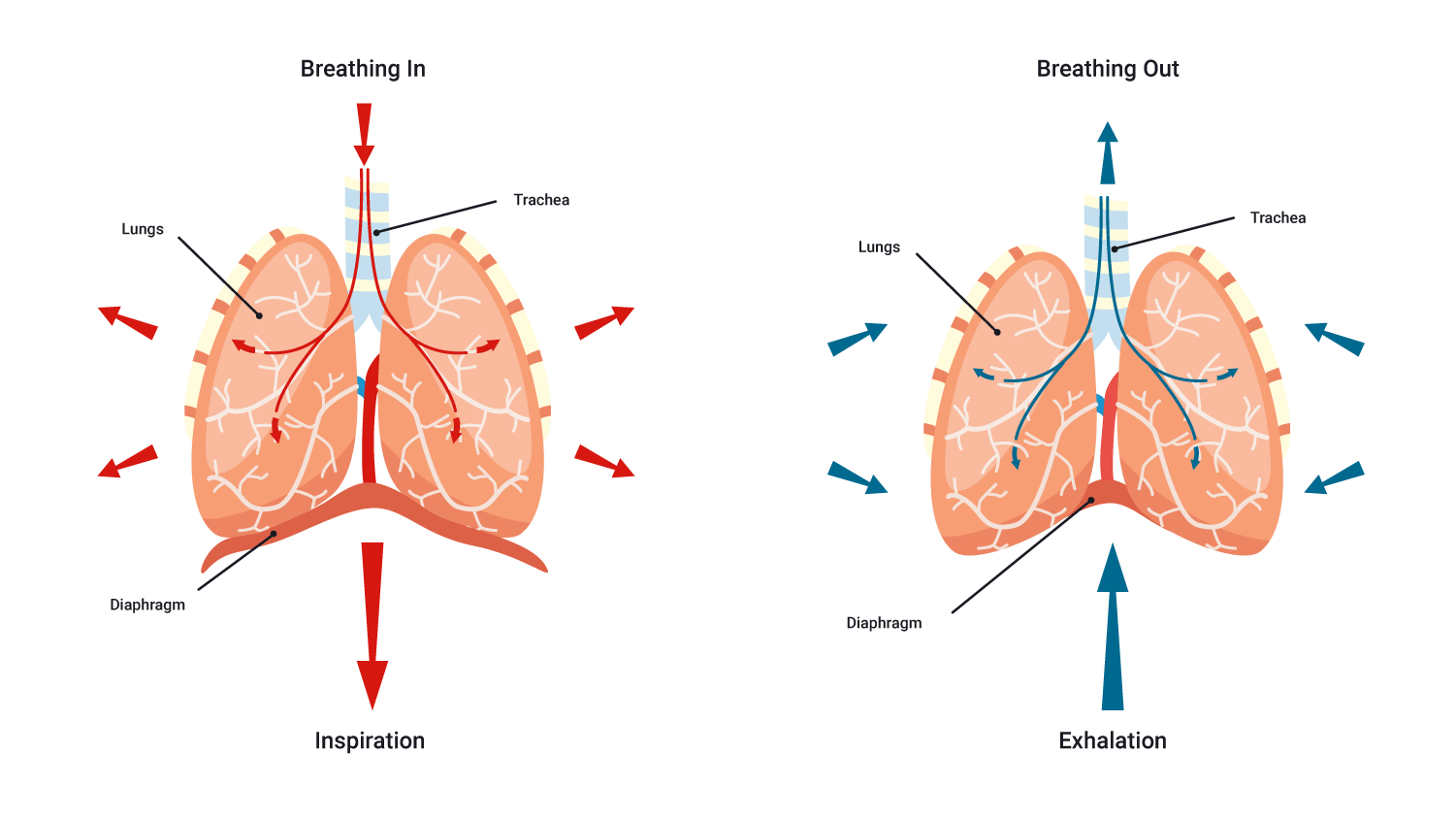
Mechanics and muscles of expiration
Expiration begins as inspiration ends.
Expiration also occurs as a result of a pressure difference/pressure gradient but conversely, the gradient is reversed; the pressure in the lungs is greater than the atmospheric pressure which in turn encourages air to flow out of the lungs.
Fun fact: In passive/regular expiration, there are no muscles used as such; rather, the muscles which were innervated for inspiration to occur simply undergo what is referred to as elastic/muscular recoil and return to their resting position. For this reason, expiration is referred to as a 'passive process' implying no energy is required.
The diaphragm relaxes, the external intercostals relax, the ribs are depressed. The combination of these results in the volume of the lungs decreasing and thus increasing the pressure within the lungs, getting ready for the next inhalation.
Mechanics and muscles involved in forced exhalation/expiration
Having said this, expiration, can, at times, be an active and forced process. This is typically referred to as 'forced expiration'. For example, think about when you have been exercising hard and are breathing very hard, coughing, or playing a wind instrument.
There we see the recruitment of the abdominal and the internal intercostal muscles. These muscles contract, increasing the pressure within the abdominal region and thorax, depressing the rib cage and forcing the diaphragm up. This further reduces the volume (and in turn increases the pressure) within the thoracic cavity (in comparison to passive expiration).
Take a moment to watch the following video which provides a brief summary of breathing thus far.
Now we have learned, in detail, the mechanics involved in breathing, we will now wrap up the process by looking at the main event, gas exchange!
Summary of what we know so far:
- O2 rich air is breathed in through either the mouth or nose (air is warmed, humidified, and foreign particles trapped).
- Air travels through the pharynx to the larynx and on through the trachea (more foreign particles trapped).
- Air enters the primary, secondary, and finally tertiary bronchi and moves through to the bronchioles. Alveoli on the walls of the respiratory bronchioles, alveolar ducts, and alveolar sacs are the site of gas exchange with the blood.
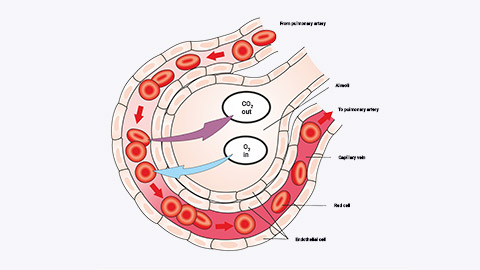
Gas exchange process: Diffusion
When discussing gas exchange within the respiratory system, the gasses referred to are oxygen and carbon dioxide; the process of gas exchange occurs is referred to as diffusion. Diffusion occurs in two phases within the body:
- Between the lungs and blood.
- Between the blood and tissues.
The rule that governs gas exchange is the same as the one that governs airflow. That is that gases diffuse from high to low pressure.
The pressure of oxygen is represented by the term PO2. It is known as the partial pressure of oxygen. The 'partial' term comes from the recognition that oxygen only makes up part of the total air pressure.
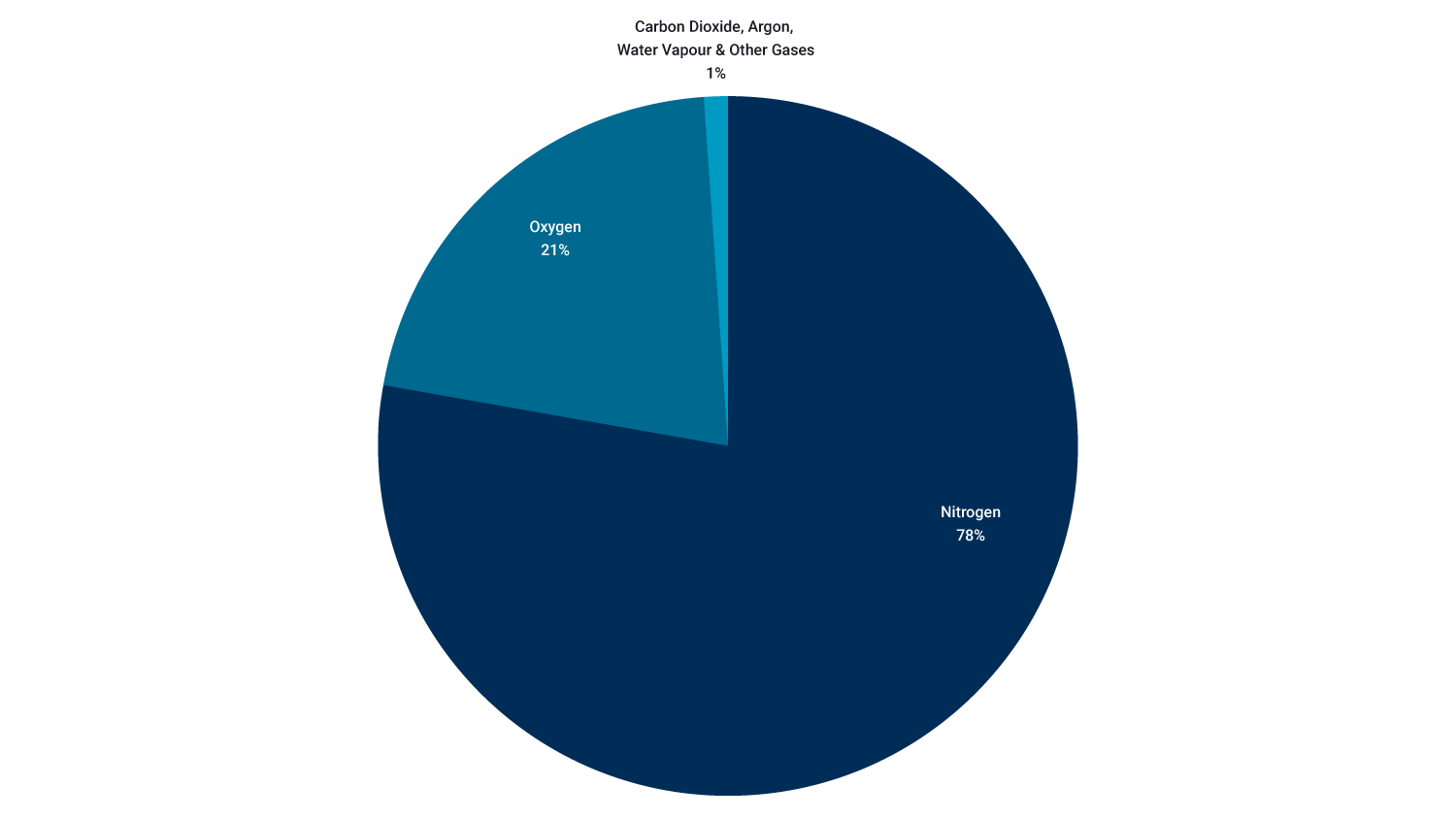
Air consists of:
- 78% nitrogen
- 21% oxygen
- 1% carbon dioxide, argon and other gases (approximately 0.003% CO2)
Air has a total pressure of 760 mmHg so the partial pressure of oxygen (PO2) is:
PO2= 0.21 x 760mmHg = 159mmHg
Phases of Diffusion
Let’s now take a closer look at each of the two phases of diffusion.
- Diffusion of oxygen from lungs (alveoli) to blood (hemoglobin)
- In order for oxygen to move out of the alveoli and into the blood, there needs to be a higher concentration of oxygen in the alveoli than in the blood.
- Blood returning to the lungs has a lower PO2 as it has delivered some of its oxygen to cells of the body.
- PO2 in blood entering the lungs is 40mmHg (low). PO2 in the lungs is 105mmHg (high), so O2 diffuses out of the lungs into the blood due to the rule of gas flow.
- Diffusion of Gases between blood and tissues
- At tissues (cells), O2 diffuses from the blood to tissues, and CO2 diffuses from tissues to the blood.
- PO2 in blood reaching the muscles is 100 mmHg (high). PO2 in muscle tissue is 40 mmHg (low). O2 diffuses from blood to tissues due to the rule of gas flow.
The following image shows the PO2 and PCO2 values at different points along the pathway of blood through the body.
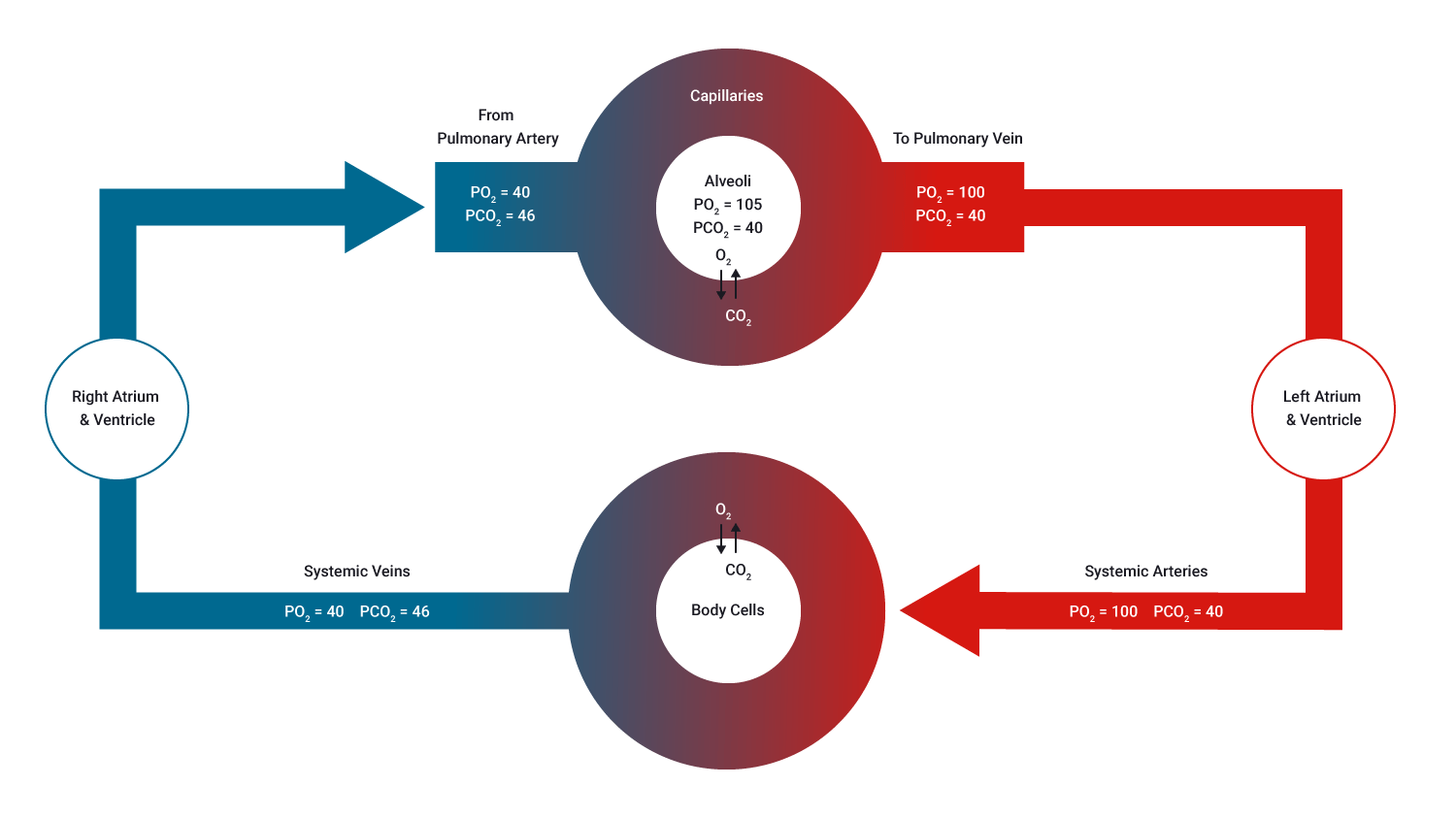
At the body cells, the PO2 has not been stated. It would be 40 mmHg in this instance as gas exchange occurs until gas proportions on both sides are even.
As the PO2 in the systemic veins is 40 mmHg, it tells us what the PO2 in the body cells is; as O2 would have diffused across the membrane until the concentrations were even in both the blood and cells.
Watch the following video which provides a great overview of gas exchange in the alveoli.
How the blood transports oxygen
Oxygen Transport in Blood
Haemoglobin (Hb), present in red blood cells carries about 98.5% of O2 within the cells of the blood (one haemoglobin molecule can carry four O2), the remaining 1.5% is dissolved in blood plasma.
Fun Fact: It is only the dissolved O2 that is free to diffuse out of the tissue capillaries and into the tissue cells. This means it is crucial to be aware that this binding relationship between oxygen and haemoglobin can be over, quicker than a heartbeat.
O2 carrying capacity
- 201 ml O2/L blood in males
- 174 ml O2/L blood in females.
Myoglobin (Mb) is an iron/oxygen-binding protein found in the muscle cells that shuttles O2 from the cell membrane to the mitochondria within the muscle cell.
Mb has a higher affinity (binding desire, think of stronger magnets) for O2 than haemoglobin, which allows Mb to store a limited amount of O2 'on-site'.
For haemoglobin to become fully saturated (that is, carrying four O2 per molecule) it doesn’t require much time. Thankfully, this is the case, because in times of an increased heart rate (for example, exertion, fright, or illness) which results in the RBCs (red blood cells) spending less time at the alveoli, (as little as 0.3 secs), there is still enough time for haemoglobin to become fully saturated with O2. Phew!
Carbon dioxide carrying capacity
So, let’s not ignore our waste product, carbon dioxide. As with oxygen, it is only the dissolved carbon dioxide (the smallest percentage of CO2, approximately 7%) which is free for diffusion when it reaches the lungs during expiration.
The greater percentage of carbon dioxide (approximately 70%) is transported in the blood as bicarbonate ions (HCO3-). These ions are broken into three parts when it reaches the alveoli, and once again CO2 is freely available to be exhaled.
Lung volumes and capacities
Lung volume is measured by a spirometer and displayed in a graph (like the following) called a spirogram. The following image shows the lung volumes of a typical male (5800mL) and female (4200mL)
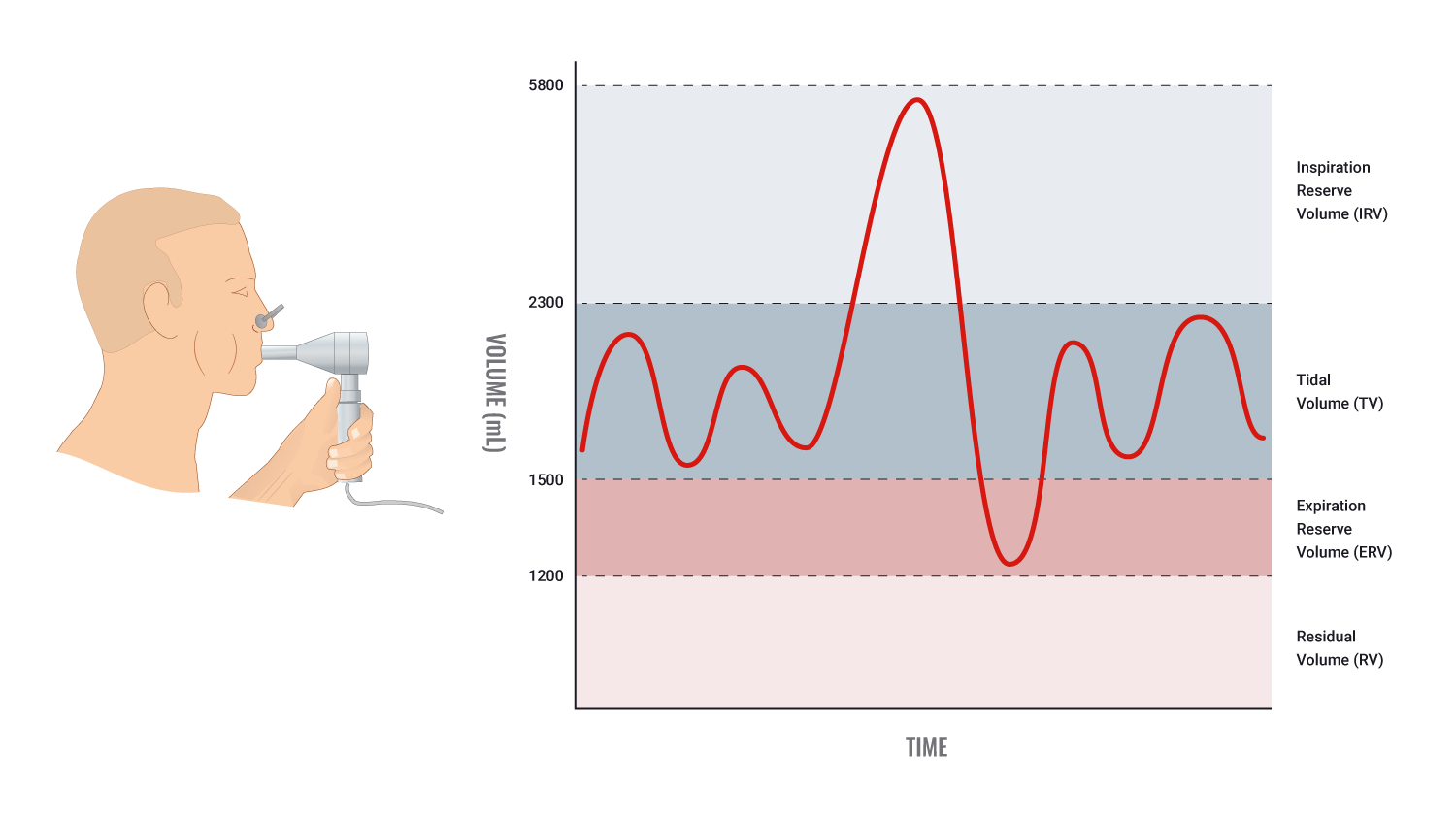
| Lung Volumes | Typical Adult Male | Typical Adult Female | Description |
|---|---|---|---|
| Tidal Volume (TV) | 500mL | 500mL | The volume of air inhaled or inhaled in one breath during quiet, relaxed breathing. |
| Inspiratory Reserve Volume (IRV) | 3000mL | 1900mL | The volume of additional inhaled air( when taking a very deep breath) |
| Expiratory Reserve Volume (ERV) | 1100mL | 700mL | If you inhale normally then forcibly exhale, the additional air, above the 500mL during quiet relaxed expiration, is known as expiratory reserve volume. |
| Residual Volume (RV) | 1200mL | 1100mL | Even after ERV is exhaled, a large volume of air remains in the lungs. This volume cannot be measured by spirometry. |
| Total Lung Volume (TLV) | 5800mL | 4200mL | The total volume of the lungs |
Note: Lung capacity is determined by combining certain lung volumes. See below for an overview of lung capacities the formulas used to calculate them.
| Lung Capacities | Typical Adult Male | Typical Adult Female | Description |
|---|---|---|---|
| Inspiratory Capacity (IC) | 3500mL | 2400mL | IRV+TV |
| Vital Capacity (VC) | 4600mL | 3100mL | IRV+TV+ERV Or IC+ERV |
| Functional Residual Capacity (FRC) | 2300mL | 1800mL | ERV+RV |
| Total Lung Capacity (TLC) | 5800mL | 4200mL | All lung volumes (IRV+TV+ERV+RV) Or IC+FRC |
Acute effects of exercise on ventilation
During exercise, ventilation (VE) increases immediately and then levels off at sub-maximal intensities to a steady-state value.
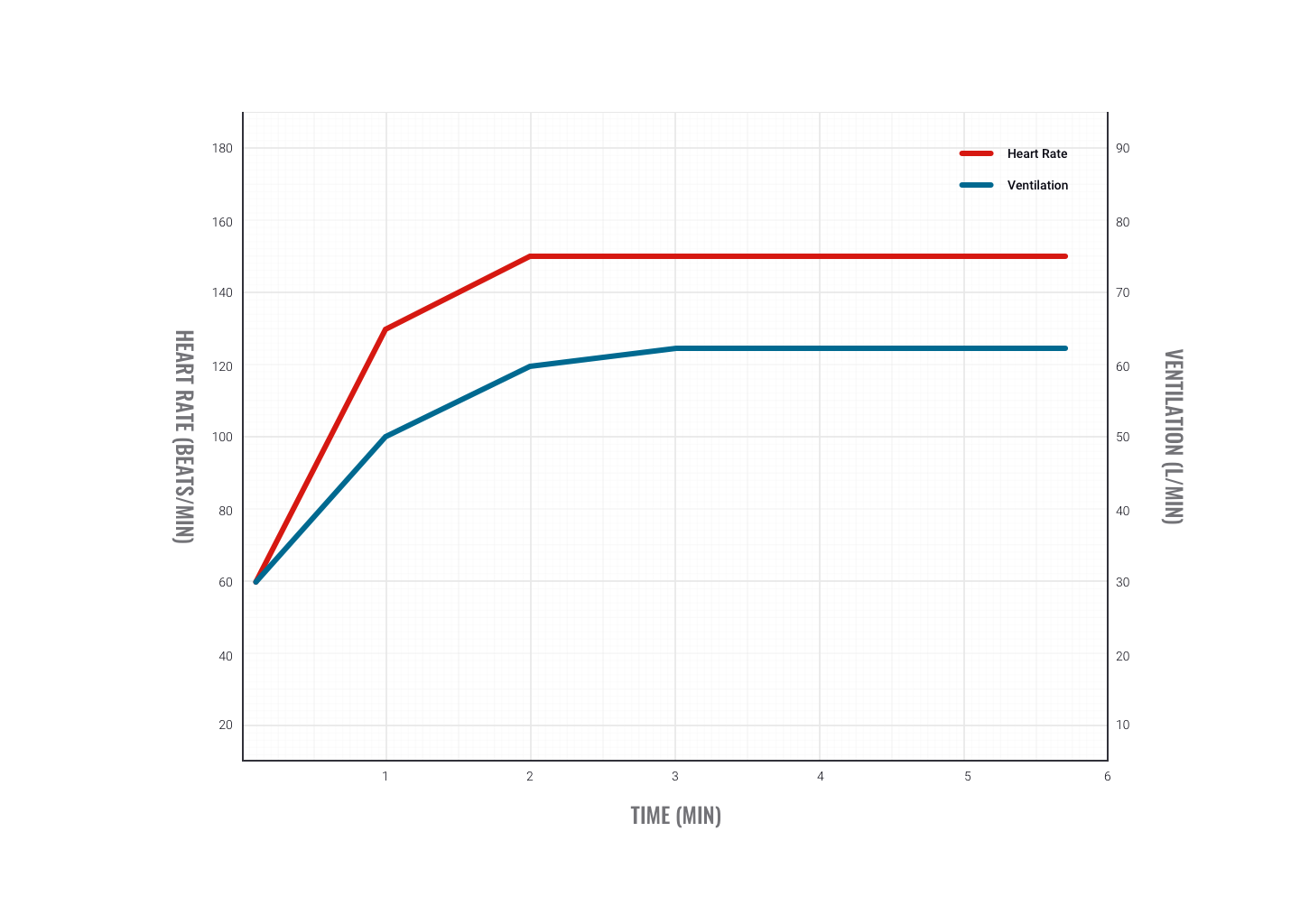
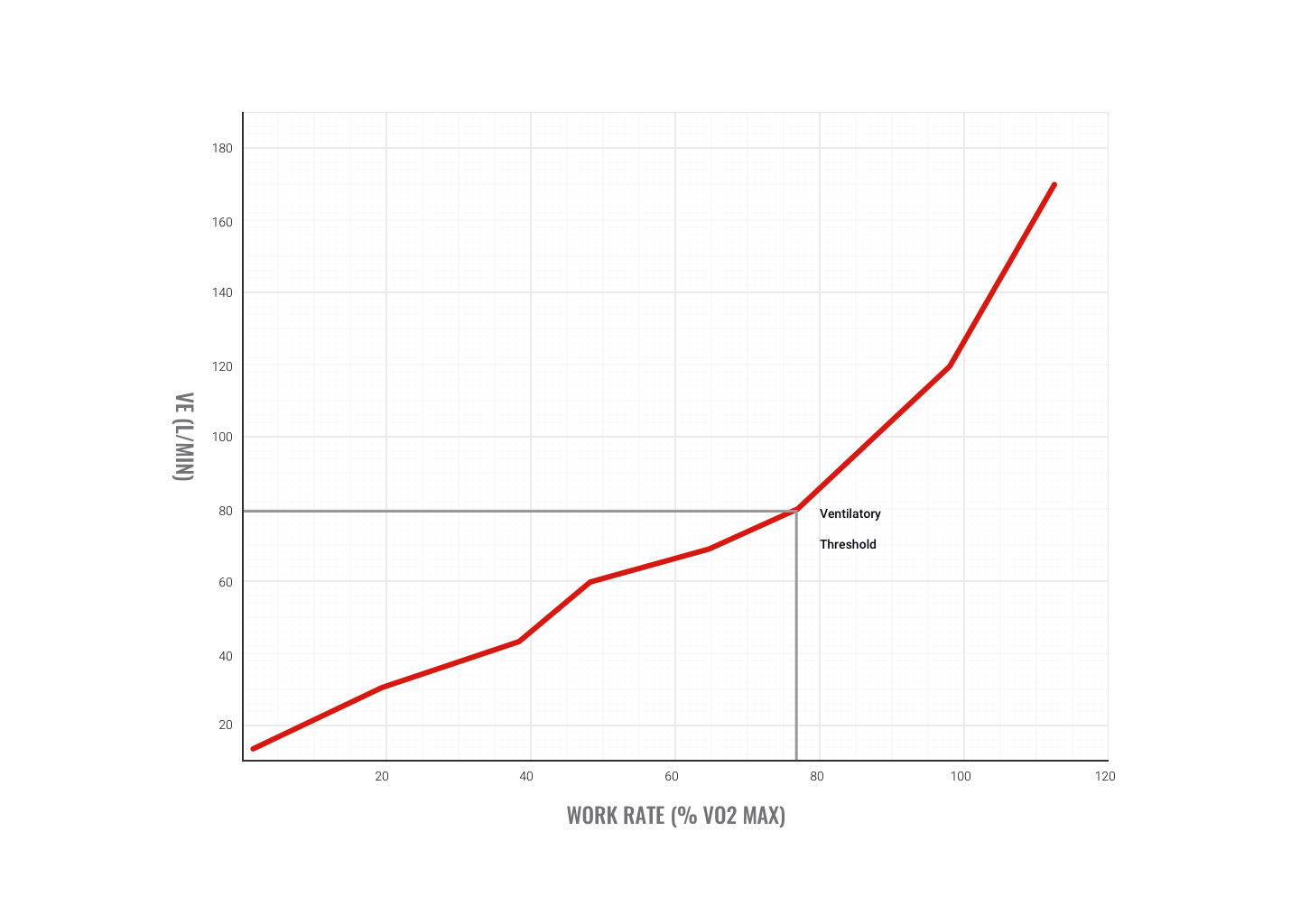
During incremental rises in exercise intensity (for example, raising intensity every minute), ventilation rises linearly in the initial stages. As exercise intensity increases towards maximum, VE increases exponentially. This is called the ventilatory threshold. The fitter you are, the higher the intensity you can work out at before you reach this point.
Why does ventilation increase during exercise?
- Muscles metabolism increases due to increased demand for work. Metabolism requires O2, thus greater amounts are required. As CO2 is a by-product of aerobic exercise, the demand for CO2 removal is also increased.
- Heart rate (HR) increases to match the gas and nutrient delivery needs of working muscles and to transport waste away from muscles. This triggers an increase in VE to provide the increased requirement of O2 and eliminate the increased amounts of CO2 being produced.
- The ventilatory threshold indicates the needs of muscle are no longer being met and the ventilation rate increases sharply in an attempt to off-load greater amounts of CO2 production. This is a strong indication that a switch from aerobic to anaerobic energy system use has occurred.
How does the brain know to increase breathing during exercise?
- The respiratory system relies on both central and peripheral chemoreceptors (chemical messengers), which give input to the respiratory control centre in the brain (hypothalamus).
- At rest, 'neural' input is sent to the control centre to stimulate the desire to breathe.
- During exercise, the information from 'humoral' chemoreceptors (gathering information from blood) is of greater importance.
- Increases in breathing depth are usually in response to increased O2 demand in the body. Increased breathing rate is more likely to be in response to increasing CO2 levels within the blood.
Receptors involved in ventilation
- Central: These are located in the medulla (brain stem) and stimulated by changes to PCO2 in spinal fluid. They send messages to the respiratory control centre to increase ventilation rate.
- Peripheral: These are found in the aorta and carotid artery and respond to increases in H+ and PCO2 in arteries. They send a message to the respiratory control centre to increase the ventilation rate.
Hyperventilation
- Hyperventilation refers to an increased rate of ventilation in excess of what is required by the body. This results in CO2 being expelled/removed at a rate faster than the body is producing it. This lowers CO2 levels in the blood and lowers pH.
- Changes to blood pH can have serious effects and will have a negative effect on gas exchange.
- This is why it is important to try and regulate your breathing during exercise.
- The method of breathing into a bag is thought to be effective as it recirculates CO2 back into the body.
Chronic effect of aerobic training on ventilation
Improvements in ventilation efficiency are mainly due to improved strength of breathing muscles, enhanced elasticity of the lungs, and higher red blood cell counts. This leads to the following improvements:
- Increase in maximum pulmonary ventilation: that is, an increased amount of air in and out of lungs.
- Increase in maximum pulmonary diffusion: more complete exchange of gas from alveoli to blood and from blood to tissues.
- Increase in a-VO2diffusion: that is, more O2 carried per litre of blood. Therefore at sub-maximal exercise rates, the heart doesn’t have to work as hard to deliver the same amount of O2.
Increased aerobic fitness leads to...
- Lower breathing rate at any intensity following training.
- This may also in part be due to lower blood lactic acid levels (enhanced waste removal due to cardiovascular improvements).
- This results in less feedback to stimulate breathing (that is, to remove waste).
Summary of the respiratory system and exercise
- Working muscles require more O2 delivery and CO2 removal than at rest.
- Receptors in the arteries and brain stem notice increases in PCO2 and alert the control centre in the brain to increase ventilation.
- Due to differences in pressure between lungs and atmosphere, oxygen-rich air is drawn in through airways.
- Gases are exchanged at the alveoli (O2 and CO2) with the blood (hemoglobin) due to differences in pressure.
- Blood carries O2 from lungs to organs of the body, where (due to pressure differences) O2 is exchanged for CO2 .
- Blood carries CO2 back to lungs to be expelled.
- Lungs expel the air high in carbon dioxide, due to change in intra-pulmonary pressure.
- With regular training, ventilation becomes more efficient meaning fewer breaths are required to deliver the same amount of oxygen.
In this topic, we focused on the structure and function of the components and mechanics of the respiratory system. You learnt about:
- an overview of the structure and function of the respiratory system
- the structure and divisions of the respiratory system including the upper and lower, conduction and respiratory zone
- respiratory system structures and their functions
- the mechanics of breathing, including the:
- muscles of respiration
- pressure differences
- gas exchange and transportation, including:
- O2 and Hb
- CO2 and Mb
- pressure differences
- measurements of respiration including lung volumes and capacities and their calculations
- exercise and its effects on respiration including receptors involved in ventilation.
This slightly longer video below provides a fun and informative overview of respiration and gas exchange. Not all of the information is required at this stage however understanding the process behind the gas exchange and the effects of hyperventilation will provide dividends to your program design and client care. There is also a 'Part 1' which you may wish to view in your own time.
WARNING
This material has been reproduced and communicated to you by or on behalf of UP Education in accordance with section 113P of the Copyright Act 1968 ( the Act ).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act.
Do not remove this notice.

