Introduction
Mauri, greetings, and welcome back to Professional Practice 2, where we continue to discuss ward management. Last week, we explored the imprest system for managing ward stock and touched briefly on the Pyxis ward stock management system. We will shift our focus to the Pyxis system and e-prescribing this week and will also look at other methods to manage pharmaceutical ward stock effectively and efficiently.
Me ruku ki te kaupapa, let’s dive into the topic.
E-prescribing
E-prescribing is where a prescription is written on a computer, transmitted electronically to the pharmacy and stored on patient records, which can be accessed electronically on the wards. It takes the place of faxed prescriptions and paper charts.
How does it work?
The electronic charts are created and updated online and can be accessed by computer anywhere in the hospital. At the same time as prescribing, doctors also have electronic information available, such as drug interactions and the preferred medicine choice within the hospital guidelines.
There are some cool features of e-prescriptions, including:
- automated alerts when patients have a documented allergy to a prescribed medicine.
- drug interaction alerts from the New Zealand Formulary.
- dose range alerts for prescriptions outside the usual minimum or maximum dosage.
Benefits of e-prescribing
Electronic prescribing has many advantages for patients and the healthcare team treating them. Based on your understanding and what you’ve just read, consider two advantages of this system. When you’re ready, select the (+) symbol to expand the list of advantages.
- Complete legibility of prescriptions
- Reduced transcription errors
- Transcribing is where a doctor’s prescription is copied onto another record. It may involve copying onto new charts or copying onto discharge summaries or discharge prescriptions. E-prescribing eliminates this area of potential error.
- Ease of access to prescription information
- Improved clinician decision-making around the choice of medicines and other therapies
- Reduced the risk of patients experiencing avoidable issues with their medication, such as allergies or adverse reactions to certain drugs.
Pyxis system

Pyxis is an automated system used to store and dispense medication for patients in the wards. It interfaces with the electronic prescribing system in the hospital, the dispensing system in the pharmacy, and the electronic patient records. In the image above, you can see the Pyxis “MedStation” model, which has a touch screen on top, medication dispensing drawers and a secure metal cabinet.
How does it work?
In the Pyxis ward system, prescriptions are transmitted electronically to the pharmacy and checked by a clinical pharmacist before being loaded into the Pyxis MedStation. This is called profiling.
Here is the process for using the system on the ward:
- Users can access the Pyxis MedStation via a unique login and fingerprint scan.
- When entering the system, the nurse can select a patient from a list populated by the patient management system.
- The nurse is then presented with a list of medications for that patient.
- The nurse enters the number of tablets or injections that are needed. These will be removed from the system.
- The appropriate MedStation drawer that contains secure medication compartments will open.
- The lid on the correct compartment will open, allowing the nurse access to the selected medicine.
Watch: The Pyxis Effect: Dispensing Pills and Practical Solutions (3:55 minutes)
On a busy ward, it’s vital that patients get their medications quickly and safely. Watch this video for an overview of how the Pyxis system is used in a hospital setting and how it dramatically reduces the time it takes to provide patients with medications. Then, complete the following five questions to ensure you understand the key points.
Advantages
What do you think are the advantages of the Pyxis ward stock management system? Consider the patients, pharmacy staff, ward staff and the hospital before reading on.

Improved medication safety
- On-screen alerts, information and warnings are given. For example:
- “Too close” warnings where a medication dose may be too close to the time of the last medication dose (eg Paracetamol, Warfarin). The system can be overridden, but the nurse must enter a reason why (e.g. the last tablet was dropped onto the floor).
- Special administration instructions or warnings such as not giving quinolone antibiotics with calcium and giving flupentixol by IM injection only.
- Clozapine requires the blood results to be entered into the machine before dispensing.
- Allergy and drug interaction alerts.
- There is less chance of administration errors because the MedStation will only open the drawer where the patient’s medication is.
- Different dosage strengths of the same drug can be kept in different drawers to avoid dosage errors.
improved workflow
- Allows pharmacy and nursing staff to manage their time more efficiently.
Improved accessibility to medication
- There is a greater range of medication stored on the MedStation, so the emergency drug cupboard is accessed less often.
- Medicines are available to patients faster than with individual dispensing.
- Controlled drugs are recorded electronically, and registers are no longer needed.
Ease of Ordering and Minimisation of stock losses
- Inventory top-up requirements are electronically transmitted to the pharmacy and processed through the computer without a manual imprest, which saves significant time.
- The system provides real-time visibility of medication inventory levels. It can be set to print out a report when stock levels fall below a set amount, allowing for better inventory control and reducing the likelihood of stockouts, overstocking and expiry dates.
- A pharmacy technician loads the unit with the medications. This system minimises stock losses.
Tracking of costs and cost savings
- It's easy to find how much a patient costs the hospital, as 100% of their medication costs can be attributed to them.
- The costs of different clinical practices to treat diseases can be easily evaluated, as well as doctors' prescribing habits.
- Less waste and medication are going missing from wards.
Improved security
- The Pyxis MedStation accurately records who has dispensed medication.
- With user authentication and audit trails, the Pyxis system enhances security by restricting access to authorised personnel only.
- The majority of the ward's medicines are kept in the secured MedStation, which also gives the advantage of medicines being secure.
Disadvantages
As wonderful as the Pyxis ward stock management system is, there are also a few disadvantages to this system. Again, take a minute to whakaaro (consider) at least one of these before continuing.
Initial cost and maintenance
- Implementing and maintaining the Pyxis system can be costly, requiring investment in hardware, software, and ongoing maintenance and support.
Staff training and workflow
- Proper training is essential for pharmacy and ward staff to use the Pyxis system effectively, which may require additional time and resources.
- Introducing the Pyxis system may require adjustments to existing workflows and processes, which can temporarily disrupt staff routines and productivity until they adapt to the new system.
Technical issues and downtime
- Like any electronic system, the Pyxis system is susceptible to technical glitches or downtime, which can disrupt medication dispensing processes and affect patient care.
- Hospitals may become overly reliant on the Pyxis system, potentially leading to challenges if the system malfunctions or experiences connectivity issues.
Stock management for Controlled Drugs (CDs)

Each hospital will have its own procedures and protocols for managing controlled drugs in accordance with the Misuse of Drugs Act 1975 and Misuse of Drugs Regulations 1977.
Ordering CDs
A registered nurse orders CDs. A specific order form is used in hospitals where an automated ward management system is not used. This is filled out and sent to the pharmacy according to the individual hospital protocol.
The order form will require the following information:
- The date of request
- The ward number
- The name and signature of the person requesting the stock
- The name and form of the medication
- The quantity required.
Sometimes, the nurse in charge will countersign them.
CD stock is not normally ordered for individual patients as the ward may have limited space in the ward safe. Registered nurses can measure doses and administer medications from the original pack.
Urgent requests
Most hospitals will have specific days and times by which they order CDs. However, urgent requests can be made, in which case the nurse may have to uplift the CD from the pharmacy themselves.
Delivering and receiving CDs
Here are the processes for delivering and receiving CDs:
Delivering CDs
- CDs designated for ward delivery are enclosed in a sealable bag, which is fastened with a numbered security seal.
- The seal number is recorded on the original order form and the delivery slip or accompanying documentation.
- Controlled drugs may be transported by security personnel, pharmacy assistants, technicians, or pharmacists, depending on hospital policy.
- CDs are typically delivered using an unmarked trolley or package.
Receiving CDs
- A registered nurse on the ward receives and signs for the controlled drugs.
- On receipt of the package, the security seal will be checked with the delivery slip or book to ensure it corresponds.
- The stock is locked in the ward safe, entered into the register and checked according to hospital protocol.
Note: Generally, only stat doses of controlled drugs are dispensed to an individual patient (e.g. a stat dose of oxycodone on a ward that does not usually keep it). In this case, the chart is faxed down to the pharmacy as usual, and it is collected by the nurse or delivered by a technician or pharmacist.
Journal post
Delivery of CDs
- Create a new journal post titled ‘Delivery of CDs’.
- Answer the following question. You may wish to do some rangahau (research) to guide your answer.
- Why are CDs delivered from the pharmacy to the ward using an unmarked trolley or package?
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts so you can check back for tutor feedback.
Record keeping and stocktaking for CDs
Record keeping and regular stocktakes of CDs are legally required and extremely important.
It is so important, in fact, that CDs are counted daily, weekly, monthly and twice a year. It’s a lot! Here are some key points to remember:
- Two pharmacy technicians or pharmacists sign the CDs.
- All in-goings and out-goings of CDs need to be written in a CD register.
- An inventory of all the medications in the safe may be done once a week to check that the stock levels reflect what is written in the register. This involves counting all tablets and measuring all the liquids.
Solid-dose CDs
- Three times a day, the solid dose CDs are counted at the start or end of a shift change.
Liquid CDs
- On the wards, nurses measure and record the overage of a liquid-controlled drug when the bottle is first opened.
- Some hospitals conduct monthly measurements of any leftover liquid CD medication. Any surplus is recorded and documented on the ‘Drugs for destruction’ page for appropriate disposal.
All CDs
- Once a week, all CDs are counted and measured.
- A physical stocktake (where everything, including liquids, is measured, counted and recorded) is carried out twice a year in accordance with legal requirements.
Storage of CDs
There are strict storage requirements for all Class A and B controlled drugs as per the Misuse of Drugs Regulation 1977, Regulation 28: Custody of controlled drugs. If these regulations are not met, this will result in a breach of the legislation and prosecution.
The storage requirements are as follows:
- CDs must be kept in a key or combination locked compartment or safe.
- The safe or compartment must be constructed of concrete or metal.
- The safe or compartment must be securely fixed to or part of the building.
- The key or combination to the safe or compartment must be kept in a safe place when not being used.
Some hospitals may also store high-risk medications in the safe and have them distributed with the CD drug deliveries, such as potassium chloride ampoules, as they can be easily confused with sodium chloride ampoules, resulting in death.
Distribution of stock
CD and non-CD stock can be distributed to the wards from a hospital pharmacy in two ways:
- Orderlies
- Lamson tube system.
Orderlies
Orderlies pick up the stock from the pharmacy and deliver it to the ward.
An advantage of this is that it saves pharmacy staff time as they don’t need to deliver it themselves.
Distribution via the Lamson tube system
This is an old school system that has been around for over 100 years! This system of tubes is installed throughout the hospital building, connecting various departments, including the pharmacy, to the wards. Medicines are placed into canisters and propelled through a system of tubes using air pressure.
The advantage of this method is a fast delivery time without requiring staff to hand-deliver stock, saving time for orderlies and staff.
Stock security
CDs and non-CDs need to be kept safe and secure at all times. Although we always like to think the best of people, in hospitals, there can be a risk of medications being stolen or diverted for personal use by staff, tampering with medications, or theft by external parties.
The following actions should be taken to maintain the security of CD and non-CD stock:
- Keep medicines out of public or patient-accessible spaces.
- Do not leave containers of medicines open or unattended.
- Have a lock on the ward storage door or cupboard.
- Do not use signage on the stock door or cupboard.
- Do not have medicines visible during distribution transport.
- Limit and control who has access to the medicine ward storage area.
- Carry out regular inspections of medication storage areas to identify any potential security vulnerabilities or breaches.
- Train and educate staff members regarding the importance of medication security protocols and procedures.
- Observe for and report any suspicious activities related to medication security promptly.
Knowledge check
Phew, you’ve been bombarded with a mountain of information about CD management, stock distribution, and security protocols during ward management processes. Complete this five-question pātaitai (quiz) to have some fun and test your retention of this content.
Self-directed learning activities
Once again, you have the freedom to choose how to spend your SDL time this week. For some guidance or inspiration on how to spend this precious time, you may like to do some or all of the following:
- Learn more about Pyxis by exploring the manufacturer's website here: BD Pyxis™ MedStation™ ES System
- Review your learning from the last few weeks. This may include re-reading your online learning, aiming for 100% on the quizzes, and updating your study notes and glossary.
- For an added challenge, you may like to create and share your own study materials (such as notes, flashcards, or quizzes) with your fellow ākonga (students) in the forum. SDL: Review Learning. Remember, if you use your peers' materials, think critically about the information you read. Is it accurate, relevant, and reliable? If you think something is a bit off, chat with them about it!
- Prepare for upcoming assessments. Ensure that you understand what is required of you, and chat with your tutor or pharmacy colleagues if you require clarification or support.
That’s this session of Professional Practice done and dusted. Tino pai, very good.

Introduction
Kia ora, and welcome back to Dispensing 2! This week, we leave aseptic compounding behind and detour into parenteral nutrition, the method of getting nutrition into the body through the veins (intravenously). In this topic, we discuss what nutrition is required to keep humans healthy and strategies for meeting these requirements.
We'll examine various forms of nutritional support and dive into the practices and procedures for preparing and administering parenteral nutrition. By the end of this topic, you will be equipped with the basic knowledge to assist pharmacists in ensuring patients receive optimal nutritional care.
Tip
Remember to add to your personal glossary as we progress through this topic. Doing so will help reinforce your understanding of key terms and concepts and enhance your overall comprehension of the topic.We’ll start with an overview of human nutrition. While some of this content may be familiar from your previous learning, it serves as a valuable refresher and expansion of your existing knowledge. Let’s bite into it.
Human nutrition overview
Human nutrition refers to the complex process by which individuals acquire and use nutrients from food for the proper functioning of the body. If people don’t eat enough food or the right type of food, they are in danger of being malnourished, which can impact their brains, immune system, and physical development (to name a few!).
As you will remember from earlier in the course, when we consume food, it enters the body through the mouth and travels down the gastrointestinal (GI) tract, where digestion begins.
Draw on your previous learning to complete the following description of what happens in the digestive process.
Types of nutrients
Nutrients fall into two groups:
- macronutrients
- micronutrients.
You probably know more than you realise about these two groups. Complete the following documentation tool to reflect on your current knowledge. You don't need to do any research, the purpose of this activity is to reflect and draw upon what you already know.
Kia haere tonu tatou, let’s continue to compare your answers and confirm your understanding.
Macronutrients

Macronutrients are the essential nutrients the body requires in large quantities to maintain proper health and function.
Select the (+) symbols to view more about these macronutrients.
- Carbohydrates are the body's primary source of energy. They include complex carbohydrates such as starches and simple sugars such as glucose, lactose, fructose and sucrose.
- They are found in foods like grains, fruits, vegetables, and dairy products.
- They are essential for providing the energy needed for physical activity, brain function, and the functioning of vital organs.
- The recommended daily intake of carbohydrates varies depending on factors such as age, sex, weight, and activity level.
- Generally, carbohydrates should make up about 45% - 65% of total daily calorie intake.
- Fibre refers to certain types of carbohydrates that our body cannot digest. These carbohydrates pass through the intestinal tract intact and help to move waste out of the body.
- Foods that are rich sources of fibre include lentils, beans, chickpeas, oats, and brown rice.
- Fibre-rich foods also contain powerful protective agents, such as antioxidants and phytochemicals.
- High-fibre diets can also help in weight control and managing diseases such as diabetes.
- Proteins are molecules made up of amino acids, which are the building blocks of the body's cells, tissues, and organs.
- They are found in foods like meat, fish, poultry, eggs, dairy products, beans, and legumes.
- They are crucial in muscle growth and repair, immune function, enzyme production, and hormone regulation.
- The recommended daily intake of protein varies based on individual factors.
- Generally, protein intake should make up about 10-20% of total daily calorie intake.
- Fats are a concentrated source of energy and are essential for absorbing fat-soluble vitamins (A, D, E, and K), maintaining healthy skin and hair, and providing insulation for organs.
- They are found in foods like avocados, nuts, seeds, olive oil, fatty fish (such as salmon and mackerel), cheese, and butter.
- They serve as a long-term energy reserve, help regulate body temperature, and are necessary for proper brain function and cell membrane structure.
- The recommended daily intake of fats also varies based on individual factors, but generally, they should make up less than 30% of total daily calorie intake.
Micronutrients

Micronutrients are essential nutrients required by the body in smaller quantities compared to macronutrients, but they are equally important for maintaining overall health and well-being. Select the (+) symbols to view more about these micronutrients.
- Vitamins are organic compounds that are essential for normal growth, development, and metabolic processes in the body. They are classified into two categories:
- fat-soluble vitamins (A, D, E, and K)
- water-soluble vitamins (B-complex vitamins and vitamin C).
- They are found in foods like fruits, vegetables, whole grains, dairy products, eggs, meat, fish, and fortified foods.
- Vitamins are crucial in supporting immune function, promoting healthy vision, skin, and bones, facilitating energy metabolism, and acting as antioxidants to protect cells from damage.
- The recommended daily intake of vitamins varies depending on the specific vitamin and individual factors such as age, sex, and overall health. It is typically measured in micrograms (mcg) or milligrams (mg).
- Minerals are inorganic compounds (naturally occurring compounds found in the earth's crust) that are essential for various physiological functions in the body. They include:
- Macrominerals: These are typically needed at levels higher than 100 mg/day. They include sodium, potassium, calcium, phosphorus, and magnesium.
- Trace minerals (microminerals): These are typically needed at levels less than 100 mg/day. They include iron, zinc, copper, selenium, and chromium.
- Minerals are found in foods like leafy greens, nuts, seeds, dairy products, seafood, whole grains, and legumes.
- They are involved in processes such as bone formation, muscle contraction, nerve transmission, fluid balance, enzyme activation, and oxygen transport. They are essential for maintaining proper cellular function and overall health.
Watch: GCSE Biology – What are Nutrients? […] (7:05 minutes)
This wonderful video from Cognito helps summarise the different types of nutrients, their role in the body and the foods they are found in. Āta whakaaro (think carefully) as you watch and take notes on any information that is new to you or you had forgotten. There is a quiz that follows.
Journal post
Malnutrition and its consequences
When people don’t meet their nutritional requirements, they can become malnourished.
- Create a new journal titled ‘Malnutrition’.
- Pop on your rangahau (research) hat to answer the following questions in your journal.
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts so you can check back for tutor feedback.
Questions
- What is malnutrition?
- What are the causes?
- What are the consequences/results of malnutrition?
Nutritional support
Sometimes, malnourished people cannot maintain their body weight by food intake alone. This could be due to a range of reasons, such as infections, diseases, age-related factors, medical conditions (like cancer), and psychological factors (like eating disorders). In situations like these, nutritional support is recommended.
Nutritional support can be provided via either the enteral or parenteral routes, as you can see here.
Choosing the correct nutritional support
The type of nutritional support chosen for a patient will depend on factors such as:
- their ability to tolerate oral intake
- the integrity of their gastrointestinal tract
- their overall medical condition.
Enteral nutrition
Whenever possible, enteral nutrition should be considered as the first option. This approach is beneficial because it protects the integrity of the gut, thereby preventing mucosal atrophy and maintaining the mucosal barrier, reducing the risk of pathogens entering the bloodstream. Enteral nutrition also leads to fewer septic complications and better preservation of gut villi by supplying nutrients directly into the GI tract.
Parenteral nutrition
Parenteral nutrition should not be routinely administered to patients with an intact GI tract. Unlike enteral nutrition, parenteral nutrition is associated with increased complications, less preservation of gastrointestinal structure and function, and higher delivery costs. Let’s take a closer look at enteral and parenteral feeding methods.
Enteral feeding
This delivers a nutritionally complete feed containing protein, carbohydrate, fat, water, minerals and vitamins. The route can be either oral or via a feeding tube. It is generally for patients with an intact or minimally impaired GI tract who cannot ingest enough nutrients orally to meet their current needs.
As you can see in the diagram above, there are two enteral feeding methods: oral and via the enteral tube. Expand each heading below to read more about these methods.
As this feeding method is the common way of eating (via the mouth and GI tract), the focus is on supporting the patient with what and when they should eat. The following may be provided to assist with this.
- Dietary counselling: Food and meal planning advice such as how often to eat, what to eat, what to drink (such as high-nutrient drinks), and ways to maximise appetite.
- Oral nutritional supplements: Nutritionally complete liquid supplements that contain a mix of macro and micronutrients. You may have seen these types that are available from pharmacies:
- Powder form, which is reconstituted with water or milk to make 1 kcal/mL or 1.5 kcal/mL liquid. For example, Ensure powder and Sustagen Hospital Formula.
- Ready-mixed liquid forms. For example, Ensure Plus and Fortisip.
Enteral tube feeding involves delivering essential nutrients in liquid form directly into the gastrointestinal system through a thin plastic hollow tube. This method bypasses the oral cavity and oesophagus, making it useful for patients with difficulty swallowing or who cannot swallow safely.
There are different types of tubes used for enteral feeding. Three common types include:
- Nasogastric
- Percutaneous Endoscopic Gastrostomy (PEG)
- Jejunostomy.
Journal post
Enteral Feeding
It’s rangahau (research) time! In this tūmahi, you will investigate these different types of tubes to deepen your understanding of enteral feeding.
- Complete the following Documentation tool activity.
- Upload the completed activity to a new journal post titled ‘Enteral Feeding’.
- Publish to ‘All course users’.
- Save the permalink to your Index of Journal Posts. Make sure to check back for tutor feedback.
Parenteral feeding
This method involves intravenous delivery of either a portion or all of a patient's daily nutritional needs directly into the bloodstream, bypassing the GI tract. It is typically used for patients who cannot tolerate enteral feeding or have conditions that prevent adequate absorption of nutrients through the GI tract.
For example, premature babies, those with inflammatory bowel disease, intestinal obstruction, injury to the bowel or congenital abnormalities of the GI tract. When you refer to the nutritional support diagram at the beginning of this section, you can see the two types of parenteral feeding methods:
- Partial Parenteral Nutrition (PPN)
- Total Parenteral Nutrition (TPN)
Quick pause… If you haven’t already, add these terms to your glossary and complete their explanations as you read the following section.
Partial Parenteral Nutrition (PPN)
As the name suggests, Partial Parenteral Nutrition (PPN) supplies only part of the daily nutritional requirements, supplementing oral intake. It is prescribed for patients with a functioning GI tract who cannot take in enough nutrients via the oral route to meet their daily nutritional requirements. It is often given temporarily to people who need an immediate boost of calories before transitioning to a longer-term solution, such as enteral feeding or gradually resuming mouth feeding.
As you can see in this image from the National Cancer Institute, PPN is administered through a peripheral intravenous (IV) line.
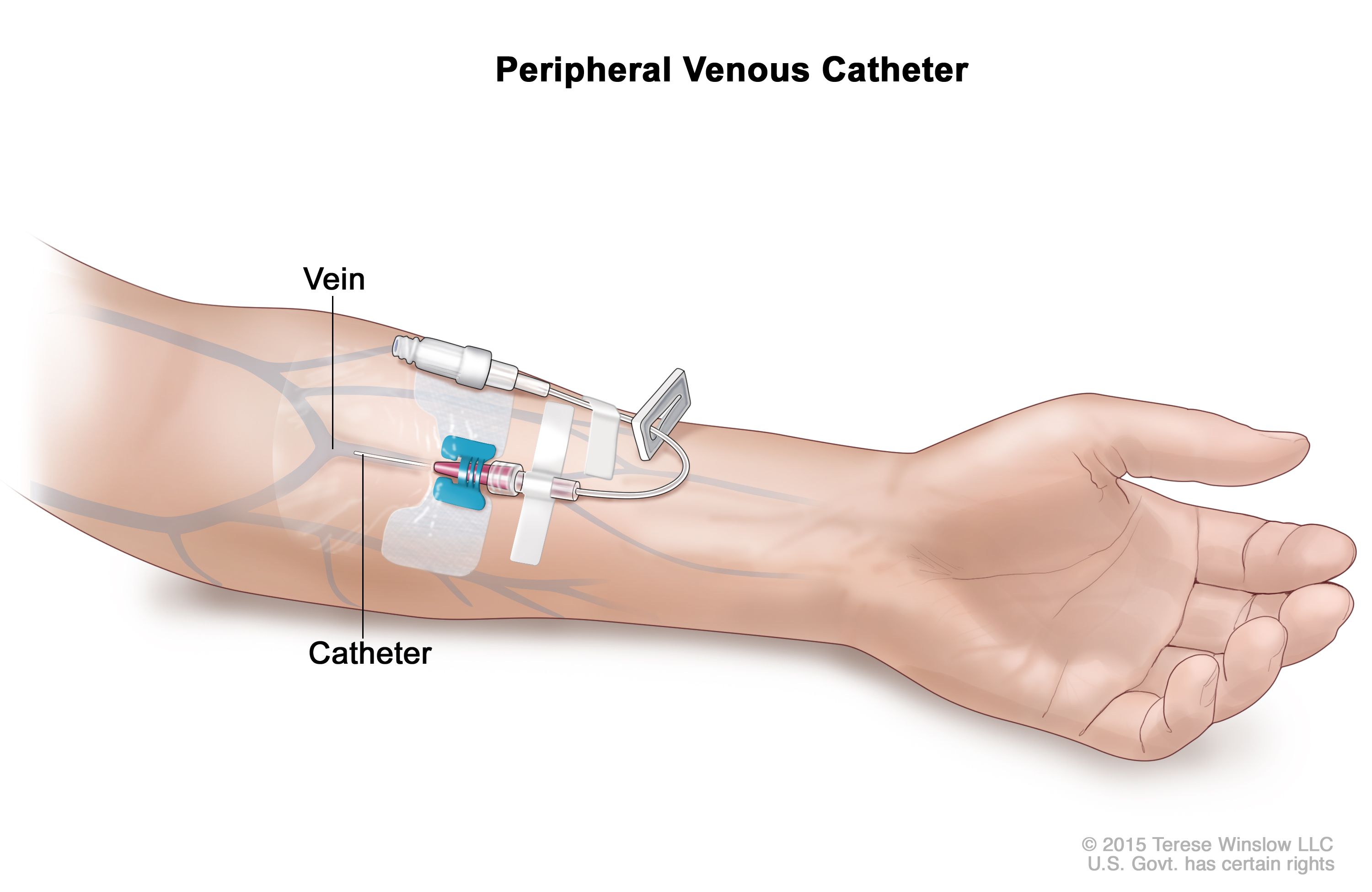
This involves inserting an IV catheter into a peripheral vein, usually in the arm. The solution delivered through this line typically contains a combination of dextrose and amino acids, providing a partial supplement to the patient's daily nutritional requirements.
As with all things, this method of parenteral feeding has both its advantages and disadvantages. Challenge yourself to think of at least two advantages and disadvantages before you select the (+) symbol to read more.
The advantages of PPN include the following:
- As it is administered through a peripheral IV line, access is quicker and less invasive than administration through a central IV line.
- There are reduced risks of complications such as infection and blood clots when delivering feeding via a peripheral vein.
- The integrity of the GI tract is maintained as oral feeding is continued alongside the administration of nutrients via the bloodstream. This concurrent oral intake helps prevent mucosal atrophy and preserves the normal physiological processes of digestion and absorption in the intestines. As a result, patients may find it easier to resume oral feeding when appropriate.
The disadvantages of PPN include the following:
- PPN can only provide a limited amount of nutrients compared to Total Parenteral Nutrition, as peripheral veins have limited capacity to tolerate hypertonic (concentrated) solutions.
- Prolonged administration of PPN solutions can lead to vein irritation and inflammation at the insertion site.
- Peripheral IV lines can still pose risks such as inflammation of the vein (phlebitis), leakage of solution into surrounding tissue causing swelling (infiltration), and damage (extravasation).
- It is unsuitable for long-term use due to the limited availability of peripheral veins and the risk of vein damage over time.
Total Parenteral Nutrition (TPN)
 Image: Fresenius
Image: Fresenius
Total Parenteral Nutrition (TPN) is where all the patient’s daily nutritional requirements are delivered directly into the bloodstream. TPN is chosen over PPN when the patient's nutritional needs cannot be met adequately through partial supplementation. This may be due to factors such as the inability to tolerate oral or enteral feeding, severe malabsorption, or extensive bowel disease.
Depending on the patient’s requirements, TPN can be prescribed to a patient for the short or long term.
Short-term
If a patient is prescribed short-term TPN, the treatment goals are to:
- return the patient back to enteral feeding as soon as possible
- provide adequate nutritional support for the duration of when the patient cannot take food by enteral route.
Long-term
If a patient is on long-term TPN, the treatment goals are to:
- provide adequate nutrients to the patient.
- minimise the risk of complications.
Regardless of the length of time that TPN is prescribed to a patient, providing TPN therapy for patients requires a cohesive and collaborative multidisciplinary healthcare team.
The hospital staff involved in TPN therapy include the:
- clinical team managing the patient
- dietician
- pharmacist.
Let’s find out more about each.
The clinical team managing the patient
Their role is to assess and manage the patient. Medical staff prescribe the TPN therapy based on the patient's nutritional needs and medical condition, while nursing staff will monitor the patient, administer the TPN solution as prescribed, and assess for any complications or adverse reactions.
The dietician
They will carry out a formal assessment of the patient's nutritional needs and develop a suggested customised TPN formula tailored to meet those needs. They will also educate the patient about their TPN.
The pharmacist
They will liaise with the dietician and will order and prepare the TPN solution, ensuring accurate compounding of ingredients and adherence to sterile compounding procedures. They advise on pharmaceutical issues such as stability and compatibility of TPN components (including medications and additives) to prevent drug interactions or adverse effects. They are also involved in patient education.
Self-directed learning activity
Watch: What is Parenteral Nutrition? (4:58 minutes)
Ask yourself this question as you mātakitaki (watch) this patent education video. Then, complete the following five-question pātaitai (quiz) to gauge your understanding of TPN and the different forms of nutritional support.
Pay special attention to the pharmacy clean rooms and laminar airflow cabinets demonstrated in the video, concepts you've previously learned about in our aseptic compounding topic!
What have you absorbed from this topic? Put your knowledge to the test.
Ka pai temahi, good work. You now have a basic understanding of human nutrition and the different types of feeding support. Next week, we will continue to explore TPN, including the pharmacy practices and procedures for preparing prescribed TPN solutions.
