To finish off Professional Practice 2, this week, we discuss medication management services, clinical trials and commonly used medicines in the hospital. Me tīmata tatou, let’s get started.
Medicine reconciliation recap
During last week's dive into medicine reconciliation, we highlighted what happens when a patient is discharged from the hospital. Use your knowledge of this to complete the short activity.
It's important to note that for some patients, this regime may differ from the one they arrived at the hospital with.
What happens when patients return home?
Although pharmacists and pharmacy technicians are crucial in educating patients who are being discharged about their new medication regimen, it's important to recognise that some patients may require extra assistance with their medications once they return home.
In such instances, pharmacy staff can refer patients to an appropriate medication management service to ensure they receive their medications safely and adhere to their prescribed regimen. This additional support can significantly enhance patient outcomes and medication adherence.
This leads us to the first topic of this week…
Medication management services

You may already be familiar with some of the medication management services from your previous studies. These services are designed to provide comprehensive support to patients in managing their medications effectively.
Journal post
Medication management services
Wā rangahau, research time!
As a pharmacy technician, you must know about medication management services so you can guide patients to the appropriate services or make referrals as needed.
- Research to complete the following Documentation tool activity.
- You may like to team up with a classmate to complete the activity.
- Upload the completed activity to a new journal post, ‘Medication Management Services’.
- Publish to ‘All course users’.
- Save the permalink to ‘All course users’ so you can return to the post for tutor feedback.
Clinical trials
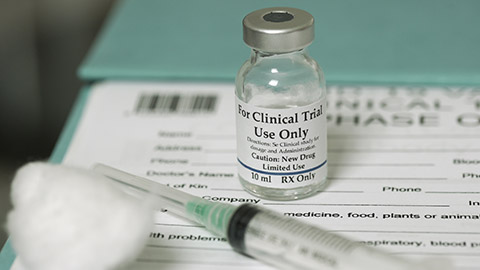
Hospital pharmacy technicians are commonly involved in clinical trials carried out in hospital settings. Their involvement often revolves around the dispensing and managing of medications used in clinical trials conducted within the hospital.
What is a clinical trial?
Reflect on what you know about clinical trials - their purpose, the processes to follow and the types of participants involved. Try to jot down at least one thing about each point before reading the information below. You might be surprised by what you already know (or can guess!)
- A clinical trial is a research study conducted to evaluate the safety, efficacy, and/or effectiveness of a medical intervention, such as a new medication, medical device, diagnostic test, or treatment procedure.
- These trials are designed to gather scientific data and evidence to determine whether the intervention/medicine is beneficial for patients and whether it should be approved for wider use in clinical practice.
Clinical trials typically follow a carefully planned protocol or study plan, which outlines the following:
- The trial's objectives
- The methods for recruiting participants
- The treatment procedures or interventions to be tested
- The parameters for measuring outcomes.
- Participants in clinical trials may include patients with a specific medical condition, healthy volunteers, or both, depending on the study's objectives.
- The results of clinical trials are used by regulatory agencies, healthcare professionals, and policymakers to make informed decisions about the approval, adoption, and use of new medical interventions.
Pharmacy technicians’ roles in clinical trials
Pharmacy technicians may be involved in the following aspects of a clinical trial.
- Medication dispensing: Pharmacy technicians may dispense the medications or study drugs required for the clinical trials. They ensure accurate preparation, labelling, and dispensing of medications according to the study protocols and regulatory requirements.
- Inventory management: Pharmacy technicians are responsible for managing the inventory of the medications used in clinical trials. This includes maintaining appropriate stock levels, tracking expiration dates, and ensuring compliance with storage requirements.
- Documentation: Pharmacy technicians assist in maintaining accurate documentation related to the dispensing and use of medications. They may document medication transactions, monitor medication usage, and ensure adherence to study protocols.
- Quality assurance: Pharmacy technicians may participate in quality control processes to ensure the integrity and safety of investigational drugs throughout the trial.
- Collaboration: Pharmacy technicians collaborate with pharmacists, research coordinators, and other healthcare professionals involved in clinical trials to ensure the smooth execution of study protocols and adherence to regulatory guidelines.
Ināianei (now), we move on to our final topic for Professional Practice 2.
Commonly used medications in hospitals

When pharmacy technicians working on hospital wards are confident and familiar with the names of commonly used medications, this promotes:
- Patient safety
- Efficiency
- Effective communication
- Adherence to protocols
- Patient education.
So, why is this important?
Self-directed learning activity
Commonly Used Medicines
Usually, medication is charted generically. However, trade names may still be used, so pharmacy technicians should know both. As you have learned in the previous content, it is also helpful for the technician to become familiar with what the drugs are used for.
Take the first step to familiarity in this week’s SDL.
- Create a new journal post titled ‘Commonly Used Medicines’.
- For each of the following medicines, record the following in your journal:
- The trade name.
- What the medicine is used for.
- Publish to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
Medicines
- alendronate
- bendroflumethiazide
- carbamazepine
- diazepam
- enoxaparin
- erythromycin
- fluoxetine
- gentamicin
- haloperidol
- levodopa
- metoclopramide
- metoprolol
- metronidazole
- omeprazole
- phenytoin
- simvastatin
- sumatriptan
optional level-up activity
The names of medicines can sometimes send your tongue into a twist when you say them out loud. As a pharmacy professional, it's OK to trip up on the pronunciation sometimes, but to avoid confusion, miscommunication and embarrassment, it's a good habit to work on this skill.
From the medicines listed, choose one that is new to you and find out how to pronounce it. You may like to search online or ask someone in person (such as a classmate, tutor or workmate). Practice makes perfect, so keep practising it until it rolls off your tongue!
If you find any great online resources to help with medicine pronunciations, share them in this week's forum so everyone can benefit: Tongue Twister.
Kei runga noa atu! Outstanding work! You have one more week of Professional Practice 2 to complete!

Nau mai, haere mai. Welcome back! In this week of Dispensing 2, we continue to discuss parenteral nutrition with a focus on the smallest and newest patients, babies. Although you will find a lot of similarities with what we’ve covered so far in this topic (which is great for confirming and strengthening your knowledge), pay close attention to the little details, as there are some differences when it comes to caring for neonates.
Parenteral nutrition for neonates
A neonate refers to a baby from birth to 28 days of life. Neonates might require parenteral nutrition when they cannot receive adequate nutrition through enteral (oral or tube feeding) means. This can occur for several reasons:
- Immaturity of the gastrointestinal tract: Neonates, especially preterm infants (those born before 37 weeks gestation), may have an immature digestive system that is incapable of effectively digesting and absorbing nutrients from milk or formula.
- Gastrointestinal dysfunction: Some neonates may have gastrointestinal conditions or disorders that impair their ability to tolerate enteral feeding, such as necrotising enterocolitis (NEC) or short bowel syndrome.
- Critical illness: Neonates with critical illnesses such as sepsis have increased metabolic demands, requiring rapid and readily available nutrition directly into the bloodstream.
- Surgical interventions: Neonates undergoing surgical procedures involving the gastrointestinal tract may temporarily require parenteral nutrition while their intestines heal and regain function.
Parenteral nutrition usually starts within the first two days of life to provide essential nutrients swiftly. At the same time, if appropriate, enteral feeding may also be started at a very slow rate. This is to help maintain the integrity of the GI tract and to transition the neonate to enteral feeding gradually.
Administration of parenteral nutrition

Neonates are typically administered parenteral nutrition through a Central Venous Catheter (CVC) (which you can see in the image above).
A Peripherally Inserted Central Catheter (PICC) is only used in the following situations:
- If it would avoid a delay in starting parenteral nutrition.
- If it would avoid interruptions in giving parenteral nutrition.
- If short-term use of peripheral venous access is anticipated, for example, less than five days.
- If central venous access is impractical.
Parenteral Nutrition (PN) solution for neonates
Neonatal PN and adult PN contain similar components, but there are often differences in concentration, composition, and formulation.
Neonatal TPN will have the same seven essential components as adult TPN. Although you’ll be familiar with these now, expand each label to see how the composition of each may differ slightly.
- Carbohydrates in neonatal TPN solutions typically consist of glucose, a simple sugar.
- They provide a readily available energy source for the neonate's metabolic processes, supporting growth and development.
- Neonates require more energy per kg of body weight than adults as they are constantly growing!
- Proteins in neonatal TPN solutions are essential for tissue growth, repair, and various metabolic functions.
- They are typically provided in the form of amino acids, which are the building blocks of proteins.
- These amino acids are carefully balanced to meet the neonate's specific nutritional requirements and their rapid growth rate.
- Fats in neonatal TPN solutions are a crucial energy source.
- Lipids, such as soybean oil or medium-chain triglycerides, are commonly used to provide these fats.
- Essential fatty acids are vital for developing the neonate's brain and nervous system.
- Electrolytes, including sodium, potassium, chloride, calcium, magnesium, and phosphorus, are important for maintaining fluid balance, nerve function, and muscle contraction.
- These are required in higher doses in babies per kg or body weight than adults.
- Vitamins and trace elements are necessary for various metabolic processes and overall growth and development.
- The dose of vitamins and minerals depends on the neonate's weight rather than a standardised dose.
- As neonates have fewer vitamin reserves and their bodies are still developing, they require higher levels of vitamin A than adults do.
- Water is a crucial component of neonatal TPN solutions, serving as a solvent for other nutrients.
- Water helps various metabolic reactions in the body.
- The amount of water in the TPN solution is carefully calculated to ensure proper hydration and to meet the neonate's fluid requirements.
Note: Neonates who are on enteral feeds in addition to parenteral nutrition will be prescribed Total Parenteral Nutrition (TPN) solutions that have reduced amounts of energy as enteral feeds increase.
Neonatal PN bags
Neonates may be prescribed a ‘starter’ bag of PN when they first begin PN therapy. The name is just that - the starter bag is used initially to provide basic nutritional support, starting the baby off in their nutritional journey. Standardised bags are then used for ongoing therapy with a more tailored approach to meet specific nutritional requirements.
Neonatal complications of PN therapy
As with adults, complications can occur as a result of PN therapy. Complications may include the following:
- Infection and catheter-related issues
- Hyperglycaemia
- Electrolyte imbalances
- The long-term use of PN in neonates can lead to a serious and life-threatening liver disease called Parenteral Nutrition-Associated Liver Disease (PNALD).
As with adults, neonates receiving parenteral nutrition are closely monitored for complications and adverse reactions.
Knowledge check
Ka pai, you've almost come to the end of parenteral nutrition. Check that you've taken this week's content on board with this 5-question pātaitai (quiz). Aim for 100%!
Self-directed Learning Activities
Now that you have come to the final week of your programme, it is time to whakaaro (reflect on) your learning journey and envisage where you want to go next.
Can you imagine if you never caught sight of your reflection? You would miss the good things (your smile lighting up your face) and the bad (like lettuce stuck between your front teeth). Self-reflection is like this. It’s about taking the time to stop and deliberately and objectively consider your experiences, which helps you to gain insight and self-awareness about your strengths and areas for development.
This skill is essential for your professional growth and something that we encourage you to carry in your learning toolbox (and take out to use often) as you progress in your career.
Kei a koe te rākau ināianei (it’s your turn now) to give yourself the gift of self-reflection.
Activity 1 – Whakaaro (Reflect)
Grab a cuppa, get yourself comfortable, and spend some time answering the reflection questions in the following Documentation tool activity. Remember, the more effort and consideration you put into your responses, the greater insight you will gain.
Activity 2 – Kōrero (Talk)
Now that you’ve turned inwards to reflect on yourself let’s open up to kōrero (talk) about your learning journey with others. This will help you to gain some outside perspective and deeper insights into your shifts in skills, mindset, attitudes and motivation which are crucial for long-term growth and development. Feel free to use the conversation prompts below to guide meaningful conversations with your whānau, friends and classmates.
You can also use this template if you want to capture these valuable conversations: Dispensing 2: Korero Template.
Conversation prompts
- What aspects of my learning journey stood out to you the most?
- Why do you think they were significant?
- In what ways do you think my skills and knowledge have evolved since I started this course?
- How do you think my attitude towards learning has shifted throughout this journey?
- Can you share any challenges you observed me facing during my studies?
- How did you see me overcome them?
- In what areas do you believe I've shown the most improvement?
- Why do you think these improvements occurred?
- What advice would you give me as I continue in my career and continue learning?
Congratulations! You have one more week of online study to go!