The skeletal system is responsible for 6 main functions.
- Support
- Protection
- Movement (assistance in movement)
- Blood cell production
- Mineral storage and release
- Storage (adipose/fat storage)
You need to be familiar with these functions as this will support you in achieving a more complete understanding of the human body and medical conditions that affect the skeletal system. The skeletal system and its functions impact how you will design programmes.
Support
The skeleton provides a structural framework, like scaffolding, which provides a structure for our body. Without the skeleton, we would essentially be a 'blob'. It also provides an attachment site for muscles, ligaments, and tendons.
For example, the vertebrae supports the torso and head.
Protection
Bone is the hardest substance in your body. It is used in many places to protect the vulnerable organs underneath from outside forces. Examples include the ribs protecting the vital internal organs such as the heart and lungs, and the cranium protecting the brain. Remember, structure mirrors function. There is a reason we are built the way we are!
Movement (assistance in movement)
Bones provide attachment points for ligaments and tendons. Muscles are attached to bones via tendons. The bones act as rigid levers for movement to occur. This movement is articulated by joints. When a muscle contracts, it shortens and pulls on the bone it is attached to. As a result, movement occurs.
What are some everyday movements your body performs? Which bones make this movement possible?
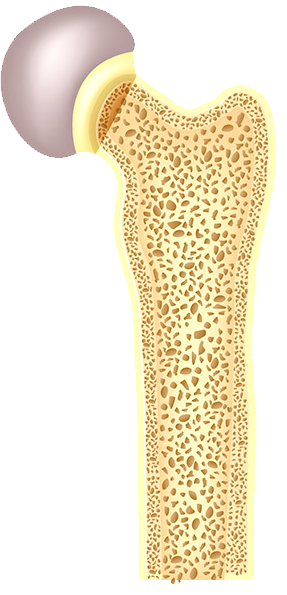
Blood cell production
The soft, spongy material in the middle of bones is called bone marrow. It produces approximately 95% of the body's blood cells.
Both red and white blood cells are formed in the bone marrow. Red blood cells (erythrocytes) carry oxygen from the lungs to the rest of the body. White blood cells fight infections and help the immune system. Platelets are another type of blood cell that is formed in the bone marrow and helps to control bleeding (John Hopkins Medicine, n.d.).
The following picture shows the many blood components produced in the bone marrow.
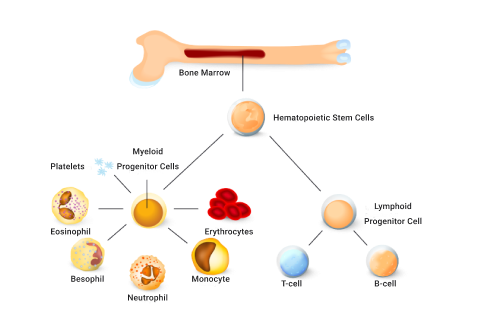
In children, blood cells are created in long bones like the femur. In adults, blood cells are mostly formed in the spine (vertebrae), hips, ribs, skull, and sternum.
Mineral storage and release
Bone is the body’s main storage of calcium. It stores around 99% of the body’s calcium and releases it when needed. Calcium is hugely important for bone growth and development and many other functions in the human body, such as muscle contraction.
Bones also store iron, potassium, and phosphorus and release them into the blood when the body needs to use them.
The pelvis, sternum, vertebrae, and clavicle are all important bones for mineral storage and release.
Storage (adipose/fat storage)
Fat tissue is also stored within the bone in the bone marrow. Bone marrow is primarily located in the ribs, vertebrae, sternum, and pelvic bones. This is additional energy storage and can be released when required to maintain physiological processes.
Watch
The following video provides a good overview of the major functions of bones.
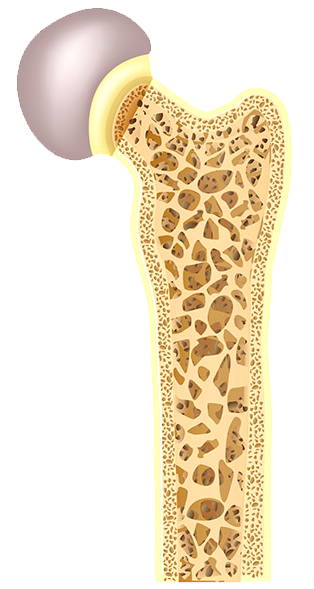
The term 'bone mineral density' refers to the amount of bone mineral (mainly calcium) present in a bone. Bones with high mineral density are stronger, can withstand greater forces, and are less likely to fracture. Bones with low mineral density are weaker and more prone to fracture under stress.
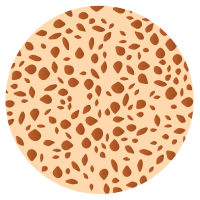
Normal bone
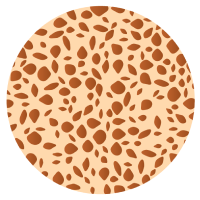
Osteopenia
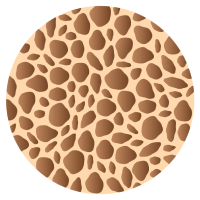
Osteoporosis
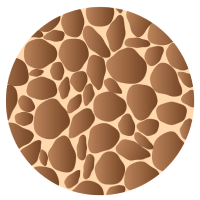
Severe Osteoporosis
Factors contributing to bone density
3 factors are critical in developing bone mineral density:
- Sex hormones: Testosterone and estrogen hormones (among others) stimulate bone deposits.
- Nutrition: Adequate food intake, including regular consumption of calcium.
- Loaded exercise: This refers to exercise that places repetitive stress on bones to encourage bones to adapt (strengthen).
How to enhance bone mineral density
We want to use exercise to improve bone strength via increasing bone mineral density.

Research has clearly shown a direct relationship between exercise and bone health. But not all exercise affects bone the same when it comes to building strong, healthy bones or preventing poor bone health, such as osteoporosis.
Loaded exercise is the key to maintaining bone mineral density and bone health.
Loaded exercise
The term 'loaded' refers to an activity that places at least body weight on bones, such as running, dancing, low-impact aerobics, or skipping. These are weight-bearing aerobic activities on your feet, where bones are supporting your weight.
When placed under mechanical stress, bone tissue becomes stronger. This is due to an increased rate of bone production, which occurs quicker than the bone reabsorption (breakdown) phase of the bone remodelling process. Activities such as jumping and running stimulate the process of bone remodelling more effectively and efficiently than activities such as low-weight-bearing activities (e.g., cycling and water-based activities) because these do not elicit the same response in terms of bone density.
To stimulate bone growth, the exercise must create stress on the bone.
People who do regular loaded physical activity produce denser and more mineralised bones when compared with sedentary individuals.
Occupations and sports that are predominantly one-arm dominant (e.g., tennis players, baseball pitchers, or cricket bowlers) result in more mineralised bones on the dominant side.
Resistance exercises can also strengthen bones, e.g. weightlifting, free weights, body weight, and exercises with resistance bands.
It is also important to include exercises for stability and balance. Improved stability and balance will help prevent falls, and help muscles work together to keep the body stable.
Nutrition
The other key factor in bone health is nutrition. You must provide your body with enough essential minerals to support bone growth and maintenance.
Watch
Dr Jen Gunter explains what you can do for strong, healthy bones in this short video.
Factors to consider when selecting exercises for bone mineral density
3 characteristics of exercises that have the largest impact on increased bone density are:
- Strain magnitude
- Strain rate
- Strain frequency
Strain magnitude
The amount of stress placed on the bones.
This is higher in exercises such as gymnastics and weightlifting, where the force or impact of the exercise is greatest.
Strain rate
This is the velocity over which the strain is placed on the bones.
This is higher in exercises such as jumping or plyometrics, where the rate at which the impact is felt is high.
Strain frequency
This is how often strain is placed on bones during the course of an activity.
This is higher in exercises such as running, where the impact on the bones frequently occurs during the exercise session.
Order of importance
Strain magnitude is the most important of the three factors for bone density. Velocity is the next most important factor, followed by frequency.
- Strain magnitude
- Strain rate (velocity)
- Strain frequency
Cross-training
Athletes involved in sports that have low strain magnitude (such as water-based sports and cycling) would benefit from a form of cross-training that is higher in strain magnitude. E.g., a water polo player may benefit from doing some weight training to ensure their bone density is maintained.
Cross-training is a form of training that typically incorporates multiple training systems through various exercises to develop and enhance overall performance.
It is important to have the correct balance of these when designing training programmes. Consider a thorough pre-screening session when working with new and existing clients.
It’s important in developing a safe and effective exercise programme design, to take the time to sit down with your client, take them through a pre-screening questionnaire and consider providing an example. Break the ice with the client to gain a thorough (but not intrusive) medical history to ensure you are aware of any potential risks you can avoid, by selecting the correct exercise and exercise frequency. This comes under the mindset of programme design and pre-screening. We'll look at this in greater detail in future modules.
Poor Bone Health
If only little stress is placed on bones, bones will demineralise.
Use it or lose it!
Bone demineralisation can happen for a variety of reasons:
- Sedentary lifestyle
- Low-impact endurance exercise
- Becoming bedridden
Nutritional deficiency can also contribute.
Normal bone
Osteopenia
Bone wasting conditions
Bone growth is dependent on sex hormones. As the levels of these hormones reduce with age, bone mineralisation decreases, and bone atrophy (wasting) can start to occur.
All of us will eventually suffer from osteopenia which is a natural de-mineralisation of bones as we get older.
If this gets to the point where daily living is compromised, it is known as osteoporosis.
Osteoporosis is a disease where new bone generation does not keep up with old bone removal. The bones become weak and brittle and more at risk of breaking. Risk factors for developing osteoporosis include:
- being over the age of 50.
- being physically inactive.
- having low levels of micronutrients such as calcium and vitamin D.

Introduction
Joints or 'articulations' are formed at the point where two bones meet. They are the connection between bones in the body and link the skeletal system as a functional whole system. Without joints, our skeleton would be a rigid deck structure unable to move. Have you ever been unfortunate enough to have a limb in a cast? If so, you know how this limited functional movement.
Joints and connective tissue hold the bones of our skeletal system together while still allowing some degree of movement.
A joint is a point of contact:
- between two bones.
- between bone and cartilage.
- between bone and teeth.
Joints have 2 main functions:
- Hold the skeleton together
- Give the skeleton mobility
Translating joint names
The scientific joint names are derived from the names of the bones involved. Let's break down "sternoclavicular joint".
- "sterno" = the sternum
- "clavicular" = the clavicle
So the sternoclavicular joint is where the clavicle meets the sternum. In the image, you can see this also applies to the acromioclavicular joint. It is located between the acromion and the clavicle.
- Sternoclavicular joint
- Clavicle
- Acromiaclavicular joint
- Acromion
- Concaid process
- Sternum
- Scapula
- Humerus
- Supraspinatus m.
- Subscapularis m.
- Infraspinatus m.
- Teres minor m.
Can you figure out which bones are involved in the following joints? Expand the accordion to check.
The tibiofemoral joint is where the femur meets the tibia. In this situation, the joint (synovial) is made complete by the patella (knee cap). Note, the patella completes the knee structure and is not classified as a component of a synovial joint.
The glenohumeral joint is where the humerus meets the glenoid cavity of the shoulder.
Of course, there are more common names for the key joints of the body.
- Hip joint: Iliofemoral joint (involving the ileum and the femur)
- Knuckle join: Metacarpophalangeal (involving the metacarpal bones and the phalangeal bones)
- Elbow joint: Humeroulnar joint (involving the humerus and the ulna)
- Ankle joint: Talocrural joint (involving the tibia, fibula and the talus (heel bone))
Sometimes it pays to be specific. As you've now seen, there are multiple joints that we could call a 'shoulder joint'. The language you use with clients, colleagues, and other health professionals will differ.
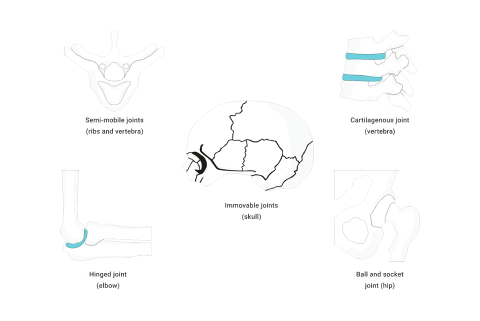
Joint Types and Classifications
The skeletal system contains different classifications of joints based on structural composition and function (degree of movement).
The main joint type we will focus on is the synovial joint.
Synovial joints are diarthrosis
They move freely. These can be further broken down into 6 groups based on how they move:
- Ball and socket joint
- Hinge joint
- Pivot joint
- Gliding (plane) joint
- Saddle joint
- Condyloid (ellipsoidal) joint

As a personal trainer, synovial joints are the joints you should become most familiar with. The risk of injury is generally greater at these joints due to the greater range of movement and subsequent reduction of the strength of the joint. These are the joints where movement happens, so knowledge of these joints and how they move is essential to exercise prescription. Synovial joints are where we will focus the most when studying joints for personal training.
The primary purpose of synovial joints is to prevent friction where two or more bones meet. All synovial joints are diarthrosis joints, but the extent of movement varies and is often limited by the connecting ligaments. Nearly all joints of the limbs and most joints of the body are synovial joints (Physiopedia, n.d.).
Structure
A synovial joint has a synovial cavity between the bones. This cavity is filled with synovial fluid. The synovial fluid:
- allows smooth, frictionless movement.
- provides nutrients.
- removes wastes.
The synovial fluid acts as a lubricant, like oil in an engine, allowing all parts of the joint to move against each other smoothly. A synovial cavity allows significant movement of the joint.
Synovial joints also contain hyaline cartilage, known as articular cartilage. Articular cartilage provides shock absorption and reduces friction.
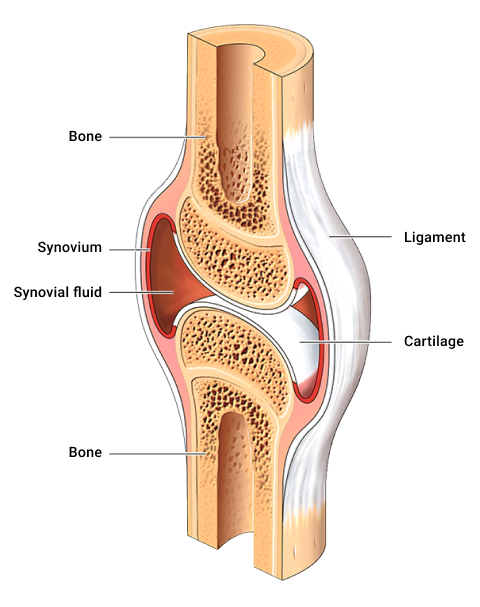
Typical structural components of synovial joints
Synovial fluid is produced by the synovial membrane and housed within the cavity. Synovial fluid is a semi-thick, clear/pale yellow fluid (which resembles the consistency and appearance of an uncooked egg white). This fluid forms a thin covering over the surface of the articular capsule.
The articular cartilage lines the ends of the bones but does not join them.
A fibrous joint capsule surrounds the joint to join the two articulating bones and enclose the synovial cavity.
The synovial membrane (synovium) secretes synovial fluid.
Accessory ligaments are present in the region of the synovial joint, e.g., the medial and lateral ligaments of the knee. They are not part of the synovial joint directly, but they support the joint.
Types of synovial joints
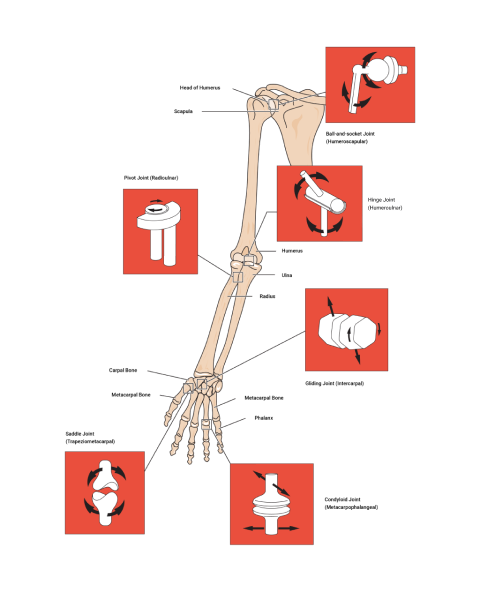
| Type of joint | How it moves | Example(s) |
|---|---|---|
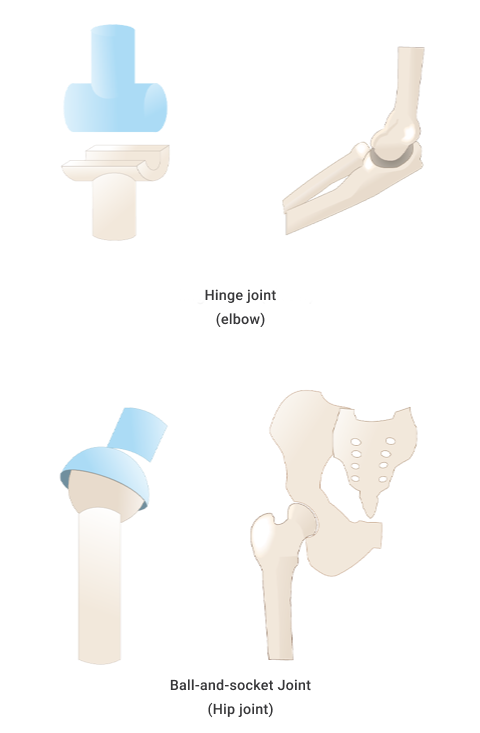
| Ball and socket | Ball and sockets are due to the end of one bone having a 'ball' like end and the other bone having a 'socket' that the ball sits in. They move in multiple planes; for example, to flex, extend, rotate, abduct, adduct, and in circumduction. | Shoulder and hip |
| Hinge | A hinge moves in one plane only, like a door hinge. | Elbow and knee |
| Pivot | A pivot is a pure 'rotating' joint. | Neck, between C1 and C2 |
| Saddle | A saddle is when the end of one bone is like a concave 'saddle' that the other bone sits over, like two legs on a riding saddle. It allows a substantial range of movements. | Fingers and thumbs |
| Gliding (plane) | Gliding occurs when short bones glide along each other in all directions (but not far). Think of it like sliding two coins together between your fingers. | Intercarpal |
| Condyloid (ellipsoidal) | Condyloid refers to shallow ball and socket joints that can do everything a ball and socket joint can do except rotate. | Wrist |
Name that joint!
Practice labelling the joints to get familiar with the names. Use the exact spelling as the list provided in the activity. For example, "Ball-and-socket" contain hyphens.
Movements
The movements provided by synovial joints include:
- Flexion and extension
- Abduction and adduction
- Circumduction
- Rotation
- Supination and pronation
- Lateral flexion
- Elevation and depression
- Protraction and retraction
- Ankle dorsiflexion and plantar flexion
Review Movement Terms in Anatomical Terminology if you need a refresher.
Move your synovial joints corresponding to those circled in the image. Identify the type of joint and the movement(s) for each joint.
Based on your knowledge of movement terms and how the different synovial joints move, can you match the movements to the joint type?
The spine makes up approximately two-fifths of your total height.
The spine is both strong and flexible. It is strong enough to support the head, neck, and body whilst being flexible enough to facilitate movement. It also protects the spinal cord, a very delicate and fragile structure that runs down the hollow passages of the vertebral column.
Vertebrae
The spinal column is composed of 33 independent bones referred to as vertebrae. These vertebrae are divided into 5 sections where the structure of each vertebra is slightly different due to the functions each performs. The vertebrae are held together by a strong network of ligaments and cushioned by vertebral disks.
Each of the following regions of the vertebral column has a specific number of vertebrae.
The cervical
This has 7 cervical vertebrae in the neck region. From the topic vertebrae to the bottom vertebrae in this region, these are named C1- C7.
The Thoracic
This has 12 thoracic vertebrae in the chest/thorax region. From the topic vertebrae to the bottom vertebrae in this region, these are named Th1-Th12.
The Lumbar
This has 5 lumbar vertebrae in the lower back region. From the topic vertebrae to the bottom vertebrae in this region, these are named L1-L5.
The Saccrum
There is 1 sacrum, which consists of 5 fused sacral vertebrae. This is referred to as the S1.
The Coccyx
There is 1 coccyx, which consists of 4 fused coccygeal vertebrae. This is referred to as the S2.
This amounts to having 33 irregular independent bones in total.
You need to know:
- the regions
- their order
- the names of each vertebrae. (C1-C7), (Th1-Th12), (L1-L5), (S1), (S2).
- the bones in each region
- the structural changes between the vertebrae of each region
This knowledge may not be called upon daily, but it underpins the rest of your anatomy, physiology, and exercise-based knowledge.
Here is a handy mnemonic to remember the regions and the number of vertebrae:
You have Cereal at 7, Tea (cuppa) at 12, Lunch at 5 (ok, it’s a late lunch) and then a Cuddle on the Sofa at 11 (11 = 1 + 1 of the sacrum and coccyx)
Try it out
Imagine you have a client that, in pre-screening, reveals they have back pain. They share with you a referral from their sports physician to their physio. The referral includes the following:
MRI showing mild loss of disc height in T10-T11 and T11-T12 and also minor loss of disc height in T2-T3 but no changes seen in the T7 area.
Before moving to the next topic, check that you have a good grasp of joints.
Watch
The following video provides a summary of joint types and classifications.
