In this topic we’ll look at common conditions that are special population groups. These conditions include children and adolescents, the elderly, pregnant individuals, individuals with obesity, diabetes, cardiovascular disease, arthritis, and asthma.
Each of these special population groups requires a different approach to exercise to ensure their safety and optimise their health benefits.
In this topic, we will discuss an overview of each condition, the benefits of exercise for that condition, signs and symptoms, possible risks associated with exercise, and training recommendations.
In this topic, we’ll cover:
- Children and adolescents
- Elderly
- Pregnancy
- Obesity
- Diabetes
- Cardiovascular disease
- Arthritis
- Asthma

Overview
In this subtopic, we focus on the effects exercise and sport can have on children and adolescents. You will learn about:
- Overview of the special population group children and adolescents
- Benefits of exercise
- Characteristics of children and adolescents
- Possible risks
- Training recommendations
Children and adolescents are a special population group when it comes to health and fitness because they are still growing and developing, and their bodies have unique needs and vulnerabilities. They typically require a greater level of fitness supervision and a different training approach.
Childhood is generally defined as the period of life from birth to 12 years old. During this time, children experience rapid growth and development, both physically and mentally. As they grow, children need a healthy and balanced diet, plenty of physical activity, and good sleep to support their overall health and wellbeing.
Adolescence is the period of life from 13 to 19 years old. This stage is marked by significant physical and emotional changes, including puberty and the transition to adulthood. Adolescents also have specific health and fitness needs, including adequate nutrition, physical activity, and sleep, as well as guidance on healthy behaviours and decision-making. As the body matures adolescents may experience the following changes:
- Increased strength due to the growth of their muscles mass
- Improved motor skills such as coordination and strength
It's important to note that the stages of childhood and adolescence are not always clear-cut or uniform, and individual children and adolescents may experience different rates of growth and development. Additionally, cultural and environmental factors can also impact the health and fitness needs of children and adolescents. Therefore, it's important to work with healthcare professionals and other experts to tailor health and fitness recommendations to individual needs and circumstances.
Training children and adolescents is quite different from training adults, due to the unique challenges and opportunities presented by their developing bodies. To ensure safe and effective training, it's important to consider factors such as age, developmental stage, and individual differences in physical and cognitive abilities. Some practical tips for adapting exercise prescription for children and adolescents include modifying exercises or activities to suit different age groups or skill levels, monitoring training intensity and volume carefully, and providing positive feedback and encouragement to promote healthy habits and attitudes towards exercise.
Expand the accordions to read more about the differences that impact exercise prescription for children and adolescents.
Because children have smaller lungs and a lower lung capacity compared to adults, they have a reduced ability to exchange oxygen and carbon dioxide. This means that when exercising, children may experience fatigue and shortness of breath more quickly than adults, which can limit their performance in cardiovascular activities such as sprinting.
Children have a faster heartbeat per minute than adults due to having a smaller heart and less blood volume. During exercise, their heart rate increases even more due to the increased demand for oxygen and nutrients. This is something to be mindful of during exercise as they may be more susceptible to over-exertion and adverse reactions such as chest pains, breathlessness, and dizziness. Careful monitoring and appropriate adjustments to intensity and duration helps keep children safe while exercising.
Children’s sweat glands are a contributing factor to overheating as they are still developing, and therefore, less effective at cooling down through evaporation than adults. It is vital that children stay hydrated and stay cool wearing loose, breathable clothing when exercising. E.g., a cotton shirt and shorts are a better alternative for sportswear than clothing made with polyester fabrics.
More heat is retained in children’s bodies during exercise due to this ratio. Children tend to overheat more quickly and are at risk of hyperthermia. It is critical to ensure that children drink plenty of water and wear breathable clothing to avoid adverse reactions.
Benefits of exercise for children and adolescents
Screentime and social media have decreased the need and desire for many young people to be physically active. This has resulted in an increasingly sedentary lifestyle. Participation in physical activity decreases with age and the decline is greater in girls than boys.
Age-appropriate physical activity helps children and adolescents with beneficial effects on:
- Body composition
- Cholesterol
- Blood pressure
- Blood sugar
- Aerobic fitness
- Muscular strength
- Movement skills (coordination)
- Bone health
- Mood
- Sleep and energy levels
- Concentration and academic performance
Regular physical activity gives young people the opportunity to learn new skills, inspires positivity, build resilience, and encourages tolerance. It relieves stress and helps children and adolescents maintain mental and emotional wellbeing. Active children and adolescents are more likely to become active adults (Physical Activity in Children and Adolescents, ACSM, 2015).
Watch
Watch the video from Sport NZ about Healthy Active Learning. This is a programme that supports schools and kura to connect with their community and enhance the wellbeing of children, encouraging healthy habits for life.
Characteristics of children and adolescents
There are a variety of characteristics which need to be considered during exercise prescription for children and adolescents. These include physical development, cognitive development, and hormonal influence.
Physical development: Childhood
Children grow at a remarkable rate. Most rapid growth happens in the first year of a child’s life and typically, children double their birth height by the time they reach 3-4 years. This slows until they reach puberty when another major growth spurt happens. The following table demonstrates the approximate growth rates per year.
| CHILDREN'S AGE | APPROXIMATE GROWTH RATE (HEIGHT) PER YEAR |
|---|---|
| 0-12 months | 25 cm |
| 1-2 years | 13 cm |
| 2-3 years | 8-9 cm |
| 3 years to puberty | 5 cm |
Young people are not simply small adults. Their body systems are growing and developing so adult exercise and conditioning programmes are not appropriate.
Physical and motor control skills
Children develop physical and motor control skills in the first 6-7 years of life. As they learn to crawl and walk, they develop coordination skills that allow them to avoid obstacles. Over time, strength and coordination skills improve, making it easier for them to participate in physical activities and sports.
Muscle growth and strength
Children aged 6-11 experience changes in muscle growth and strength, and their ligaments also undergo physiological changes. During childhood, larger muscles tend to be more developed than smaller ones, and muscle growth occurs before strength development. Bones grow at the ends, within the epiphyseal region, while ligament structures become firm and strong.
Cognitive development: Childhood
For children aged six and above, training should focus on enhancing skill development rather than fitness. Cognitive and intellectual development can also impact a child's ability and participation in sports. Activities that promote cognitive skills, such as logical thinking and problem-solving, can help improve technical skills during physical activities.
Repetition and play are key elements to help children learn and improve technical skills. Team sports are also recommended for developing social skills and positive sporting behaviour.
Physical development: Adolescence
During adolescence children go through a growth spurt where they grow taller and their bodies change. This growth spurt happens at different times for different people and parts of the body grow at different rates and times.
In the early stages of adolescence, between 11-15 years old, young people can move their bodies well with a high level of movement and coordination, but their movements can be affected by emotional fatigue. This is because their central nervous system is not yet fully developed.
Motor development

During adolescence, there is a strong focus on developing coordination, speed, and balance in movements. This includes gross motor skills, like cycling and swimming, and fine motor skills, like writing and drawing.
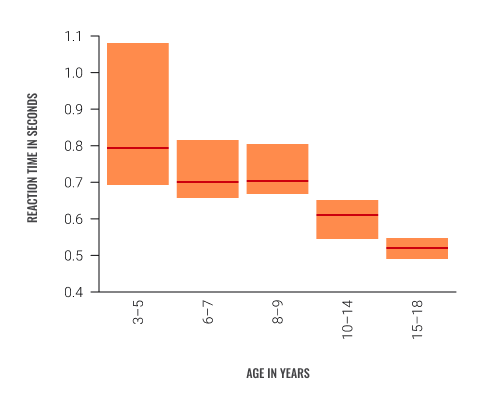
Reaction times get faster as children and adolescence get older, but training too early may not be effective. Training programmes should be designed to match young people’s abilities and development levels.
The following graph illustrates the reaction time for various age groups.
Please note: The red line reflects the average reaction time and the orange bar reflects the reactions of 25–75% of the participants.
Muscle growth and strength
During the early stages of adolescence, an increase in strength is developed due to the growth in muscle size. Boys usually get stronger than girls. The following table shows the sensitive periods for the development of static strength and power in limbs that occur with both genders at different stages.
| GENDER | STATIC STRENGTH | LEG AND ARM POWER |
|---|---|---|
| MALE | Approximately 13-16 years | Approximately 13-16 years |
| FEMALE | Approximately 11-13 years | Approximately 10-13 years |
Musculoskeletal growth and injuries
The musculoskeletal system supports the body and grows at a steady pace until it reaches a length predetermined by genetics. Children's bones grow in the growth plate and reach maturity when the plates fuse together. Most growth occurs between 9-16 years.
Injuries during the growth period can have permanent effects on growth and can cause serious problems like abnormal growth or degenerative arthritic changes. Musculoskeletal injuries include:
- Growth plate injury
- Broken bones
- Head and neck injuries
- Overuse injuries
Children's bones are flexible but not immune to fractures, so it's important to refer them to a doctor for an x-ray if there is any suspected injury.
When training, be aware that heavy training can cause injuries such as stress fractures, epiphyseal plate fractures, and Osgood-Schlatter's disease in children.
Cardiovascular capacity
Children need daily exercise like running, swimming, or cycling to develop their heart and lungs. The heart grows slowly between ages 4-10, and if the cardio-respiratory system doesn't keep up with the musculoskeletal system, a child's ability to cope with exercise will decrease. Females are 1-2 years more advanced than males at the end of this phase. Younger children have a lower proportion of anaerobic energy they can generate.
Children require more oxygen during exercise than adults, but their heart and lung capacity is smaller, so they have a limited oxygen distribution. This means they have a lower capacity for intense cardiovascular activity compared to adults, and they may not be as effective in short-duration, high-energy activities like sprinting.
About 5 in 1000 children are born with a heart defect, but only 2-3 have severe conditions that limit their physical activity. Proper screening and supervision during exercise are important to detect signs like breathlessness, which should be investigated by a doctor.
Hormonal influence
Adolescence is driven by hormones, and androgens, a group of sex hormones, play a big role in the physical changes in children and adolescents' bodies. Androgens help with body shaping, improving cardiovascular function, and increasing endurance and strength during exercise.
Watch this short excerpt from Sport NZ. Neuroscience Trainer, Kathryn Berkett discusses how adolescent hormones impact sport.
Females and males can play sports together, but there are physiological differences to consider during puberty due to differing hormone levels.
- Strength and height: Males are generally stronger and taller than females because of testosterone.
- Breast development: Female’s breast development may affect vigorous training due to sensitivity and sportswear.
- Pelvis: The pelvis weakens and widens during puberty in females, which can cause orthopaedic dysfunction during exercise.
- Menstruation: Some people may have decreased energy levels during their menstrual cycle while others set personal bests. Menstruation may impact willingness to participate in physical activity.
- Flexibility: Females are often more flexible than males, but they may have joint laxity (hypermobility), which increases the risk of injury.
Gender stereotypes
Throughout history, the perception of genders along with their ability in skills, expectations of performance and conduct in both males and females, has impacted their participation in physical activity. Click on each of the following stereotypes to read more about dissolving these assumptions when training children.
This comes from the myth that boys are more competent in sporting activities than girls. Parents have been shown to provide less encouragement for physical activity and offer fewer sport-related opportunities for their daughters than for their sons (Fredricks and Eccles, 2005).
During the ages of 2 to 8 years, children are in a sensitive period for learning fundamental motor skills. This is the optimal time for acquiring skills, as later learning is more difficult and less effective.
Girls may have fewer opportunities to develop these skills during their sensitive periods, which can lead to disadvantages in sports later. Strenuous conditioning activities can still improve their physical fitness, without negative impacts on menstruation or future pregnancy and childbirth.
Youth are often pressured into "gender-appropriate" sports (Hannon, Soohoo, Reel, & Ratliffe, 2009). If someone tells you that their child plays rugby and the other is a netballer, what assumption do you typically make about these kids? The gendered assumption would be that a boy plays rugby, and a girl plays netball.
Boys who are not physically skilled or good athletes experience ridicule and embarrassment, based on the rigid male stereotype that includes strength, muscularity, athleticism, and lack of empathy for other participants (Tischler & McCaughtry, 2011). Boys who are good at sports are often popular among peers, with enhanced self-esteem and self-image and positive identity. The ridicule experienced by boys who do not fit the culturally prescribed gender role may cause them to struggle with self-esteem and social relationships.
Sexualisation values women primarily for their sexual appeal and reduces them to objects of sexual use. Female athletes are often depicted in sexualised poses rather than in action shots, while male athletes are not. This phenomenon starts at puberty and contributes to low self-esteem, depression, mental illnesses, and eating disorders in females. Viewing sexualised images of female athletes can have negative impacts on girls' body image, whereas images of female athletes in action can increase their motivation to be physically active (Daniels, 2009).
These assumptions should not impact training of either sex or gender. Physical activity should always be encouraged to maintain a healthy lifestyle. Training should always be adjusted to suit the individual child or adolescent based on their own unique capabilities.
Possible risks
Children and adolescents are a special population group because there are risks and special considerations for exercise prescription.
As we’ve discussed, their body systems are growing and developing. High stress or continuous repetitive movements should be done with caution because these types of exercises can cause injury. You can minimise risk by teaching young people correct techniques and modifying exercises and intensity.
Young people have immature thermoregulatory systems. So, ensure young clients are properly hydrated and exercise in comfortable environments, wearing appropriate clothing.
Children and adolescents may suffer from a variety of medical conditions or disabilities that can impact their ability to engage in physical activities. Exercise programmes should be tailored to their specific needs. Common medical conditions affecting young people include:
- Asthma
- Diabetes
- Epilepsy
We’ll cover asthma and diabetes in detail in their own subtopics. These conditions impact many people across ages and are special population groups in their own right. For now, we’ll simply look at the exercise risk of these conditions as they relate to children and adolescents.
Asthma
In New Zealand, over 570,000 people take medication for asthma and one in seven (14.8%) children aged 2-14 years has been diagnosed with asthma (Bpac nz, better medicine, n.d.).
Asthma affects the airways and causes bronchospasms, swelling of the airway passages, and increased mucus production.
Asthma attacks can be triggered by allergens (e.g., animal fur, cigarette smoke, pollen) or exercise, but children with asthma can still participate in physical activity with a management plan in place. This may include the use of an inhaler. The risk of asthma attacks can also be minimised by ensuring children and adolescents with asthma have a proper warm-up before exercise and cool-down afterwards.
Other respiratory diseases which impact children and adolescents in New Zealand include bronchiectasis, childhood bronchiolitis, childhood pneumonia, and chronic obstructive pulmonary disease. Respiratory disease is New Zealand’s third most common cause of death and there are significant disparities in its prevalence based on ethnicity and socio-economic status.
Diabetes
Diabetes is a medical condition where the level of glucose in the blood is too high. There are 2 types of diabetes:
- Type 1: The insulin-making cells in the pancreas are destroyed and cannot make enough insulin. It is caused by genetic and environmental factors. It is not caused by eating too much sugar or any other foods.
- Type 2: The body is not able to use insulin effectively due to resistance to insulin. Genetics can be a risk factor, but the major risk factor is being overweight. The risk can be lessened by being physically active and eating a healthy diet (Diabetes in Children – An Overview, KidsHealth, 2022).
Over 250,000 people in New Zealand have been diagnosed with diabetes. It is more common among Māori, Pacific and South Asian people and the rate of both type 1 and 2 diabetes is increasing, especially lifestyle-related type 2 diabetes.
Type 1 diabetes is usually diagnosed in children, whereas type 2 diabetes usually develops in adults. However, type 2 is becoming more common in young people (Diabetes, Ministry of Health, 2022).
Children and adolescents with type 1 diabetes effectively treat their symptoms:
- Insulin injected into a layer of fat under the skin
- Eating a healthy diet including carbohydrates for growth and development, just like a child without diabetes
- Being physically active
- Matching insulin to the amount of carbohydrates they eat and physical activity they do
- Learning about diabetes
Children and adolescents with type 1 diabetes effectively treat their symptoms:
- Making lifestyle adjustments including healthy eating, increasing physical activity, and weight loss
- Tablets to help the body use insulin more effectively, insulin injections, or a combination of both (KidsHealth, 2022)
When children and adolescents with diabetes exercise, they can have low blood sugar (hypoglycaemia) or high blood sugar (hyperglycaemia).
Low blood sugar can happen during or after exercise and happens when the body uses up too much of its stored sugar, especially if insulin levels are still high after an injection. Signs to watch out for include:
- Sweating
- Light-headedness
- Headache
- Problems concentrating
- Confusion
- Shakiness
- Weakness
- Anxiety
- Hunger
More severe signs include fainting and seizures.
Minimise the risk of low blood sugar by making sure children check blood sugar levels and have an extra snack. Your client’s doctor may recommend a reduced insulin dosage in the case of rigorous exercise.
High blood sugar needs to be address before or during exercise. Muscles need more energy during exercise so the body will release glucose into the blood. If there isn’t enough insulin, the glucose will stay in the blood. Signs to watch out for include:
- Need to urinate more frequently which can lead to dehydration (especially when combined with increased sweating and breathing during exercise)
- Excessive thirst
- Tiredness
- Weakness
- Blurry vision
If there is not enough insulin in the blood, ketones may build up during exercise, putting the child at risk of diabetic ketoacidosis (DKA). DKA is severe and life-threatening. It requires immediate treatment. Symptoms include nausea, vomiting, abdominal pain, rapid breathing, and unconsciousness.
Children and adolescents with type 1 diabetes should test for ketones, and check blood sugar levels, before exercising and you should be aware how to give extra insulin if necessary. Work with the child’s GP or health team to safely support your client. Be aware of the signs of hypoglycaemia and hyperglycaemia and stop exercise immediately if your client shows any of these signs (Sports, Exercise, and Diabetes, n.d.).
Epilepsy
Children with epilepsy have epileptic seizures. Abnormal electrical activity causes unusual movements, behaviour, or funny feelings. In New Zealand, epilepsy affects 1 in every 200 children (Epilepsy in Children, KidsHealth, 2021).
Have a look at the following video that further explains the different types of seizures that can occur with epilepsy.
Seizures can be triggered by flashing lights or deep breathing. The chance of a seizure can increase with tiredness, illness, fever, stress, or excitement.
When working with children and adolescents with epilepsy, discuss with them or their caregivers and health team to understand how they manage it along with how you can support them. During exercise, pay close attention to them during certain activities, e.g., water-based activities as an underwater seizure is life-threatening and should involve extreme close supervision.
It is advised that the best way to deal with a child having a seizure is to allow the normal seizure to run its course. It is important to not restrain the child, ensure that they are away from any sharp objects and their head is safe / protected allowing the seizure to run its natural course. Following the seizure, the child will feel tired or sleepy and it is wise to restrict activity during this time.
Training recommendations for children and adolescents
In addition to standard practice of pre-screening, testing, programme design, and coaching, there are some special recommendations when working with children and adolescents. In particular, you need to:
- Communicate positively and with language your young client understands
- Provide encouragement and focus on building intrinsic values, e.g., skill improvement, personal success, and enjoyment
- Recognise and modify exercises and variables based on individual differences and capabilities, being mindful of age and developmental stage
- Keep things interesting with creative activities/exercises and variation
- Ensure young clients are wearing appropriate footwear and clothing
- Watch for dehydration and overheating (hyperthermia)
- Demonstrate exercises with simple, clear instructions and safety guidelines
Not all children and adolescents enjoy intense competition. Most young people want to have fun, make friends, and learn something new. Think about this when programming. Traditional games like jump rope and trail running will provide opportunities for young clients to run fast, jump high, change direction, and maintain balance.
Young clients with poor physical fitness may experience frustration, embarrassment, pain, or injury and want to quit. Be mindful of this and keep the experience positive.
World Health Organisation recommendations
WHO guidelines and recommendations provide details on how much physical activity is needed for good health for different age groups.
Children and adolescents aged 5-17 years should:
- Do an average of 60 minutes per day or moderate-to-vigorous intensity (mostly aerobic) physical activity, across the week
- Incorporate vigorous-intensity aerobic activities, and those that strengthen muscle and bone, at least 3 days a week
- Limit the amount of time spent being sedentary, especially recreational screentime (Physical Activity, WHO, 2022)
Types of exercise
Activities for children and adolescents should be developmentally appropriate, offer variety, and be enjoyable.
Aerobic activities could include bicycle riding, walking, running, games, dancing, soccer, and swimming. Healthy children and adolescents do not need to monitor their heart rate during the activity period.
Activities that promote muscle strength could include climbing, jumping, tumbling and gymnastics, and a variety of games. Older children and adolescents can participate in supervised strength training programmes if the focus is on developing proper exercise technique. Examples of appropriate activities include body weight exercises (e.g., push-ups, pull-ups) and strength exercises with dumbbells, medicine balls, and resistance bands (Physical Activity in Children and Adolescents, ACSM, 2015).
Resistance training
Resistance training is growing in popularity for young people. It can be a safe and effective method for improving muscular fitness in children and adolescents. Resistance training aims to gradually increase the resistance load to achieve muscle strength, endurance, flexibility and stability.
Children as young as 6 years have been shown to benefit from resistance training. One study showed that children can improve their strength by 30% to 50% after just 8 to 12 weeks of a well-designed strength training programme and need to continue to train at least 2 times per week to maintain their strength (Dahab & McCambridge, 2009). Resistance training can also help bone density, balance, strength and flexibility for children and adolescents.
Multi-joint exercises can be incorporated, if the focus remains developing a proper technique. When learning new exercises, children should start with light loads or a with guidance via long wooden stick which provides education on posture and good technique when performing the exercises. Skilled exercise professionals should supervise training sessions and adult spotters should be present to ensure form and safety.
Final words
Exercise offers physical, mental, cognitive, and emotional benefits to children and adolescents and you can make an impact.
Overall, children and adolescents will require the support of a personal trainer that can approach programming and coaching in a well-planned, safe, and effective manner. One key element to be mindful of is the importance of educating children in the importance of physical activity, introducing children to an active lifestyle and most importantly, the ability to adhere to regular exercise for long-term health benefits.
When working with young people, think about characteristics such as physical development, cognitive development, and hormonal influence. Be aware of risks and how to minimise them. Remember that children and adolescents are not simply small adults – adapt your programming and coaching accordingly.

Overview
In this subtopic, we focus on the effects exercise and sport can have on elderly populations. You will learn about:
- Overview of the special population group elderly people
- Benefits of exercise
- Characteristics of elderly people
- Possible risks
- Training recommendations
Elderly people are a special population group when it comes to health and fitness due to age-related changes in physiological function that can impact their ability to perform physical activities. They require specialised considerations, including a focus on safety, proper form and technique, and appropriate exercise selection and intensity.
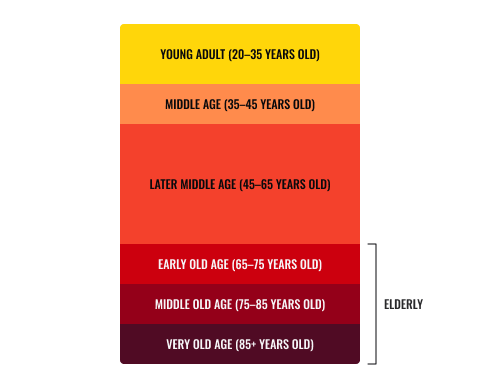
Elderly is generally defined as the people aged 65 and older. Age can be classified as follows:
- 20-35 Young Adult
- 35-45 Middle Age
- 45-65 Later Middle Age
- 65-75 Early Old Age
- 75-85 Middle Old Age
- 85+ Very Old Age
Clients in early old age usually have a modest increase in activity to fill their days after retirement. There may be some development of disability. Mobility declines and significant postural changes are evident. Poor physical capacity is common.
Clients in middle old age usually have one or more physical disabilities and a process total dependence (loss of independence) begins.
In New Zealand, there are about 842,000 people aged 65 years or older and this is estimated to reach 1 million by 2028. It will continue to increase over the next 50 years. The proportion of elderly is also increasing. In 2022, 1 in every 6 people were aged 65+ and by 2028 it will be 1 in every 5 (Stats NZ, 2022).
While population ageing is not new, it will really accelerate over the next decade. The increasing number and proportion of older people in the population has implications across New Zealand's society.Hamish Slack, Stats NZ
The stages of old age are not always clear-cut or uniform, and individual older people may experience different characteristics to each other. Cultural and environmental factors can also impact the health and fitness needs of elderly people.
Any assessment should be based on physical and mental condition of the body rather than actual age.
Benefits of exercise for elderly populations
As a personal trainer, it's important to understand the many benefits of exercise for elderly populations. Regular physical activity can improve quality of life for older people, promoting independence, mobility, and overall wellbeing. Here are some key benefits to keep in mind:
- Improved cardiovascular health: Aerobic exercise can help maintain or improve heart and lung function, reducing the risk of cardiovascular disease and related complications.
- Increased strength and mobility: Resistance training can help combat age-related muscle loss (sarcopenia) and improve overall strength and mobility, making it easier for older people to perform daily activities.
- Reduced risk of falls: Exercise programmes that focus on balance and coordination can help reduce the risk of falls and related injuries in older adults.
- Enhanced cognitive function: Studies have shown that exercise can improve cognitive function in elderly people, helping to prevent or delay cognitive decline.
- Boosted mood and mental health: Exercise has been linked to improved mood and reduced risk of depression and anxiety in older adults.
- Prevention or management of chronic conditions: Regular exercise can help prevent or manage chronic conditions such as diabetes, arthritis, and osteoporosis.
- Socialisation and community building: Group exercise programmes can help older adults stay socially connected and engaged with their communities, improving overall wellbeing.
- Improved resting metabolic rate: Resistance training can increase lean muscle mass and subsequently increase the basal metabolic rate (calories burned while resting).
It's important to work with elderly clients to develop exercise programmes that are safe, effective, and enjoyable. By emphasising the many benefits of exercise and tailoring programmes to individual needs and preferences, you can help older people achieve their fitness goals and improve their quality of life.
Watch
In this video, older people and fitness professionals discuss how staying active helps older people enjoy long and good quality lives.
Characteristics of elderly populations
There is a significant increase in numbers of elderly individuals with growing risk factors towards health conditions and decreased daily physical capacity. Physiological changes occur within each organ and body system as aging occurs. These include changes to:
- Energy consumption
- Bone mineral density
- Mobility
- Aerobic capacity
- Blood pressure
- Body composition
Energy consumption
Recent studies indicate that basal metabolic rate (BMR) and total energy expenditure (TEE) remain relatively stable during adulthood (20 – 60 years). The point TEE starts to decline is 63 years, and adjusted for BMR was 46.5 years.
At approximately 60 years old, both TEE and BMR begin to decline. Fat-free mass and fat mass also decline, but the declines in energy expenditure exceeded what would be expected from reduced body mass alone. The 2021 study found that TEE and BMR declined by 0.7% each year, which means people that are 90 years old had a TEE roughly 26% lower than middle-aged people (Pontzer et al. 2021).
Bone mineral density
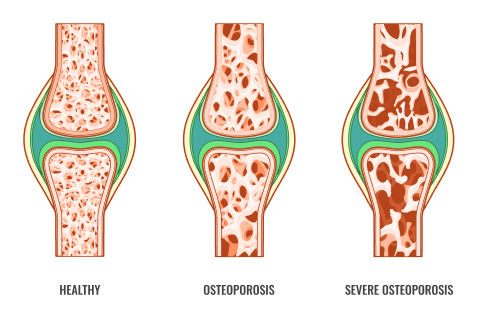
As we age, bone mineral density decreases, usually starting around age 50. This is due to a higher rate of bone breakdown than formation, leading to porous bones and osteoporosis. Osteoporosis is a degenerative condition of bone tissue and makes daily activities harder and increases fracture risk, especially in the hips, spine, and wrists. Fractures develop easily and are slow to heal. Women are at greater risk, losing about 8% of bone tissue annually, while men lose about 3%.
Degenerative joint disease (DJD)
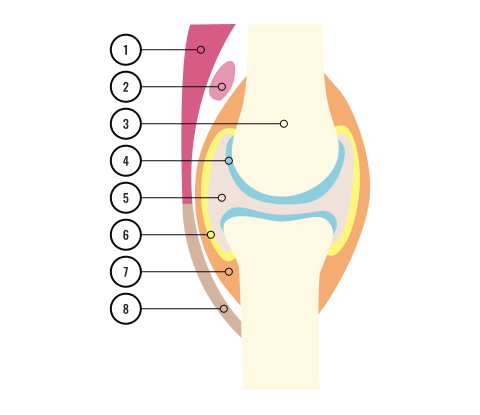
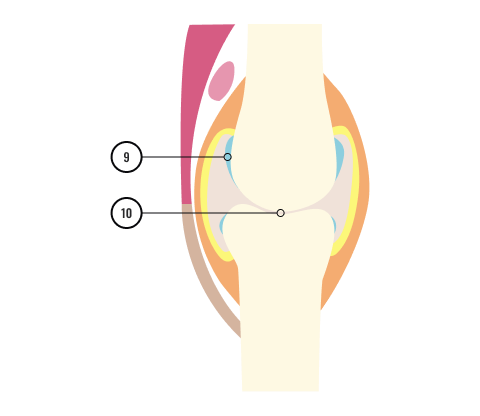
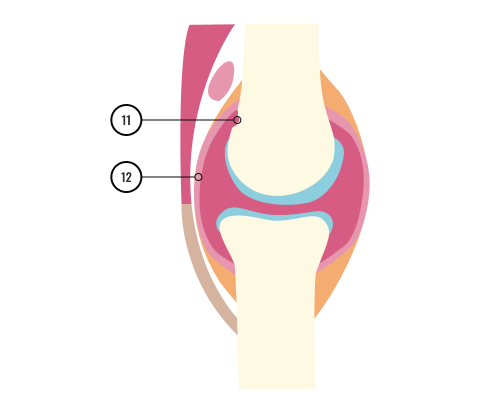
- Muscle
- Bursa
- Bone
- Cartilage
- Synovial fluid
- Synovial membrane
- Joint capsule
- Tendon
- Eroded cartilage
- Bone ends rub together
- Bone erosion
- Swollen, inflamed synovial membrane
Joint degeneration or degenerative joint disease (DJD) is a form of osteoarthritis, also known as 'wear and tear' arthritis. It occurs when the protective connective tissue (cartilage) covering the end of each bone wears down, causing bones to rub together and resulting in pain, swelling, and stiffness in the joints.
Osteoarthritis is the most common form of arthritis, affecting approximately 10% of New Zealand adults. It can affect people of all ages, but usually starts after age 40 (Arthritis NZ, n.d.).
Mobility
Reduced mobility is a common characteristic among elderly individuals, often caused by joint deterioration and loss of function in surrounding tissues. These changes can greatly impact their ability to perform daily activities, such as walking, showering, dressing, household chores, and transferring between sitting and standing positions.
It is estimated that 35% of individuals over 85 years old experience mobility problems. These changes can lead to dizzy spells, particularly postural hypotension when transitioning between positions. Therefore, improving mobility is an important goal when working with elderly clients.
Aerobic capacity
Aerobic capacity declines in elderly individuals due to factors such as:
- a reduction in myocardial contractility (leading to decrease in stroke volume)
- arterial obstruction of up to 30% by age 45
- a decrease in blood vessel elasticity
- a 50% reduction in maximum lung capacity between ages 30-70
VO2max and cardiovascular endurance also decline starting at age 20, which can impact maximal heart rate during exercise (calculated as 220 minus age).
Blood pressure
Blood pressure tends to increase gradually as we age, especially in elderly individuals, who are more likely to experience high blood pressure. The cause is not fully understood, but is believed to be related to changes in the blood vessels and heart over time, as well as lifestyle factors such as obesity, lack of physical activity, high sodium intake, and certain medications.
High blood pressure in the elderly can increase the risk of heart disease, stroke, and other complications, so it is important for them to monitor and manage their blood pressure with their healthcare provider.
Body composition
As we age, our body composition tends to change in ways that can negatively impact our health and quality of life. Elderly individuals are at risk for decreased muscle mass and bone density, as well as an increased accumulation of fat mass.
These changes can contribute to a decrease in strength and mobility, putting them at risk for falls and fractures. Additionally, a higher proportion of body fat can increase the risk for chronic diseases such as diabetes and cardiovascular disease.
Age-related changes in hormones, decreased physical activity, and reduced nutrient absorption can all contribute to these changes in body composition.
Possible risks
As people age, their bodies undergo changes that can increase the risk of injury during exercise. Personal trainers who work with elderly clients need to be aware of these changes and take steps to minimise the risks. Some of the potential risks include falls, joint injuries, heart problems, and overexertion.
Falls are a significant concern for elderly clients, as their bones are more fragile and take longer to heal. Falls typically arise from degenerative tissues around joints, but are also impacted by:
- neurological and musculoskeletal impairment
- visual impairment
- psychological
- medication
- postural hypotension (head rush)
Personal trainers need to ensure that the exercise area is free of hazards and assist as needed to help clients maintain their balance.
Joint injuries are also a concern, as the cartilage that cushions the joints can wear down over time, leading to pain and stiffness. Trainers need to be careful not to overwork the joints and to adjust the exercises as needed to accommodate any limitations or injuries.
Heart problems become more of a concern as people age. Personal trainers need to be aware of any pre-existing conditions and monitor clients for signs of discomfort or distress during exercise.
Finally, overexertion can be a problem for elderly clients, as their bodies may not be able to handle the same level of intensity as younger clients. Trainers need to carefully monitor clients and adjust the intensity of the exercises as needed to ensure that they are not overdoing it.
Training recommendations for elderly populations
When designing exercise programmes for elderly clients, you must consider the specific needs and limitations of this population. Risks can be minimised by taking the following steps:
- Completing adequate medical screening, including identifying existing musculoskeletal conditions and current health and nutritional status
- Selecting appropriate exercises – regress exercise patterns to simple mobilising movements and progress programme to challenge the client
- Provide appropriate supervision to avoid or reduce aggravation of cardiovascular or cerebrovascular events, and muscle or joint conditions (e.g., rheumatoid arthritis and osteoarthritis)
It is also important to be aware that elderly clients may have barriers to effective communication such as:
- Loss of hearing
- Loss of vision
- Loss of balance and coordination
- Loss in confidence
They may also have perceptual deficits, which can result in difficulties or differences in inputting, processing, and recalling information, such as those seen in conditions like ADHD, Alzheimer's disease, and dementia. You may need to adjust certain aspects of your delivery and instruction. E.g., using concise language and demonstrating proper exercise technique and safety measures can enhance understanding.
Resistance training
The major goal for many elderly clients is to develop muscular fitness to enhance their ability to live a physically independent lifestyle.
For arthritic patients – never permit arthritic patients to participate in strength training exercises during active periods of pain or inflammation.
The first resistance training sessions should be closely supervised and monitored by fitness professionals who are sensitive to the needs of the elderly. Begin the first eight weeks with minimal resistance to allow for adaptations of the connective tissue elements.
Teach proper training techniques for all exercises to be used in the programme.
Instruct older participants to maintain their normal breathing while exercising, asthere can be a tendency for older clients to hold their breath.
Programme considerations
The following are some programming considerations to keep in mind when designing a strength and resistance training programme for this population:
- Frequency: Aim for 30 minutes of gentle activity, as many as 7 times per week.
- Reps: Choose a resistance that allows a client to perform at least 8 repetitions.
- Progressive overload: Increase the number of repetitions first, then increase resistance.
- Speed: Emphasise controlled movements and avoid ballistic movements.
- Type: At least 2 strength and resistance training sessions per week to produce positive physiological adaptations. Interval training is great because of the lower intensity bouts for recovery. Cardio work should start at 50% intensity of HRmax and increase from there.
- Functional: Incorporate exercises that improve posture and help with ADL (activities of daily living)
- Compound: Focus on multi-joint exercises over single joint exercises.
- Pain free: Encourage clients to perform exercises within a range of motion that is within a “pain free arc” (implying the maximum range of motion does not hurt or is uncomfortable).
- Machinery: Use machines for resistance training to promote safety and stability. Machines require less skill to use, permit the user to only move and perform the exercise in a pre-determined movement pattern, protect the back by stabilising the users body position, and allow the user to start with lower resistances.
- Stretching: Encourage gentle stretching without bouncing, reminding clients to breathe and stay within their pain-free range of motion.
- Exercise should be fun and simple to perform with a focus on skill development rather than body image and looks.
Physical activity guidelines
Regular physical activity is essential for individuals of all ages, but it becomes especially crucial for older adults to delay or mitigate the physiological changes that come with aging. To help elderly people maintain their health and independence, the New Zealand Ministry of Health has published Guidelines on Physical Activity for Older People (aged 65 years and over). These guidelines provide specific recommendations on frequency, intensity, and type of exercise that can improve the quality of life for older adults:
The key highlights of the physical activity recommendations for older people in New Zealand are:
- Be physically active as much as possible, and avoid being sedentary
- Start slowly and gradually increase physical activity
- Aim to do aerobic activity on at least five days per week for either 30 minutes of moderate-intensity or 15 minutes of vigorous-intensity
- Additionally, do three sessions of balance and flexibility activities, and two sessions of muscle strengthening activities per week
- Older adults who are frail should consult with an allied health professional before beginning or increasing physical activity
- For those who are frail, low-impact aerobic activity, resistance, balance, and flexibility exercises are recommended, and consulting a doctor or allied health professional for Vitamin D supplements is advised

Overview
In this subtopic, we focus on the effects of exercise during pregnancy. You will learn about:
- Overview of pregnancy
- Benefits of exercise
- Characteristics of pregnancy
- Possible risks
- Training recommendations
Pregnant people are considered a special population group when it comes to health and fitness because their bodies undergo significant physiological changes during pregnancy. These changes can have a significant impact on their overall health and wellbeing, as well as the health of their developing foetus.
Benefits of exercise during pregnancy
Pregnancy typically occurs over a 40-week period, grouped into 3 trimesters. Historically, there was a belief that exercising during pregnancy was too risky, but research shows that exercise, planned with a qualified healthcare professional, can offer benefits for both the mother and child. These benefits include:
- Reduced risks of complications during pregnancy and labour
- Decreased risk of premature birth
- Reduced length of labour and increased recovery rate post-birth
- Strengthened heart and blood vessels
- Improved cardiovascular fitness
- Relief from backache and improved posture
- Prevent wear and tear on joints which become loose due to hormonal changes
- Reduced constipation by accelerating movement in intestine
- Increased self-esteem and mental health
- Improved sleep
- Decreased risk of preeclampsia and gestational diabetes
- Decreased susceptibility to diabetes in the child
- Boost to foetal brain health
- Promotes healthy weight gain
It's important to maintain some form of physical activity and a healthy diet for the overall wellbeing of the pregnant individual. However, with varying opinions on effective exercise routines and dietary requirements, it's best to seek guidance from a healthcare professional if unsure.
Characteristics of pregnancy
The body changes throughout pregnancy and many of these changes will impact exercise. The following are some of the physiological changes that pregnant women experience that will need to be considered when implementing safe and effective exercise programmes.
Less lung capacity
As the foetus grows within the womb, the body will adapt to allow room, pushing up organs such as the lungs. Because of this, there may be difficulty in aerobic exercises as there is a decreased availability of oxygen. Monitor for symptoms of breathlessness during training and modify the intensity accordingly.
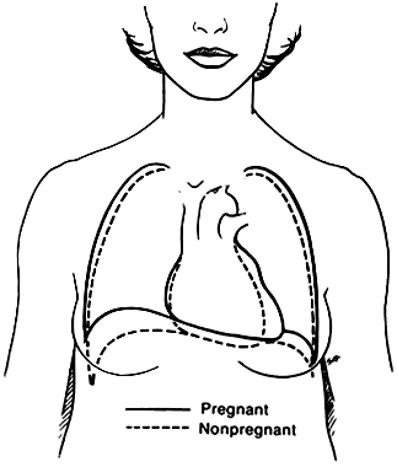
Increase in the volume of blood
The foetus places extra demand on the woman’s body for nourishment, therefore the heart increases the volume of blood by 30% – 50%. This speeds up the heart rate, putting added stress on the heart. This in turn, will need to be considered during an intense exercise programme, to ensure the heart is not over worked.
Joints and flexibility
The hormone relaxin is secreted during pregnancy. This hormone increases joint laxity (joint flexibility) which means there is a greater risk of joint injury due to increased flexibility of the stabilising connective tissues (muscles and ligaments) surrounding a joint.
- Do not take stretches to the point of maximum resistance including movements that require deep flexion or extension.
- Keep joints safe by avoiding using activities that require jumping or jarring motions, rapid changes in direction, or ballistic movements such as bouncing motions.
Balance
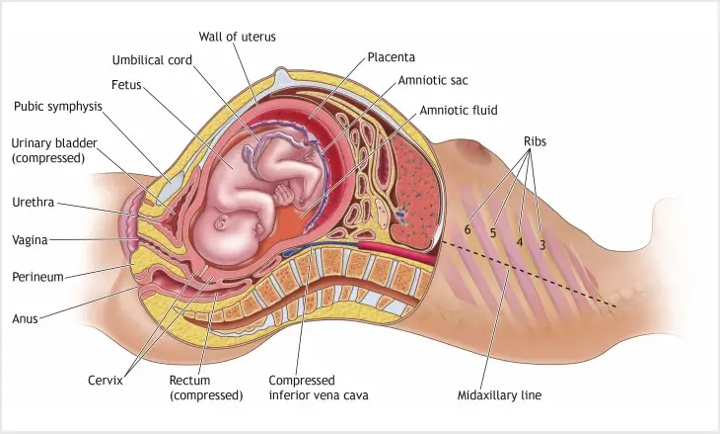
One of the obvious physical changes during pregnancy is the growth of the belly and weight gain. This growth becomes progressively more strenuous as the weight, predominantly in the front of the body (the belly), shifts the centre of gravity (COG).
Typically, a person can put on 11-18 kilos by their third trimester, adding stress to areas such as joints and muscles that can result in a higher risk of falls. The centre of gravity may affect the following:
- Posture
- Balance
- Stability
- Coordination
The centre of gravity is also altered by the hormone relaxin as it can increase lumbar lordosis (the arch in the lower back). This, along with joint laxity, can also predispose pregnant women to changes in balance and increasing occurrences of back pain. To support the shift of balance, avoid exercises that may cause abdominal trauma and exercise that involves rapid changes of directions such as twists, turns and sudden movements.
A maternity belt can also be used to alleviate any pressure on the lower body muscles.
Perform exercises on stable flooring such as on a wooden floor or tightly carpeted surface, because this will help to reduce shock to the body and provide a stable footing for balance.
Energy intake
Pregnancy requires an additional 300kcal a day so the body can maintain metabolic homeostasis.
Temperature control
Acute effects of exercise on the foetus include increases in temperature, heart rate and oxygenation.
Core temperature of mother is related to intensity and duration of exercise.
Pregnant women who exercise in the first trimester should control body temperature by:
- Staying well hydrated
- Avoiding exercise on hot humid days
- Wearing light, breathable, loose-fitting clothing
- Using fans during hot weather
- Avoiding saunas and steam baths
Possible risks
Although exercise during pregnancy can have many benefits, there are also potential risks that pregnant women and their foetuses may face. Some possible risks include:
- Increased risk of injury: As pregnancy progresses, the ligaments and joints in the body become more flexible, which can increase the risk of injury during exercise.
- Overheating: Pregnant women are at a higher risk of overheating during exercise due to changes in the body's temperature regulation. Overheating can lead to dehydration, which can be harmful to both the mother and the foetus.
- Miscarriage: Although exercise does not cause miscarriage, there is a slightly higher risk of miscarriage during the first trimester, especially if the exercise routine is too intense or involves high-impact activities.
- Preterm labour: Intense exercise or overexertion can lead to preterm labour, which is when contractions begin before 37 weeks of pregnancy.
- Restricted foetal growth: In rare cases, intense exercise can lead to restricted foetal growth or other complications, especially if the mother does not consume enough calories to support both her and the foetus's needs.
It's essential to consult a healthcare provider before starting or continuing an exercise routine during pregnancy to ensure that the activities are safe for both the mother and the developing foetus. Additionally, pregnant women should pay close attention to their bodies and avoid overexertion, overheating, and activities that may increase the risk of injury.
Supine position
Women should avoid exercise in the supine position after the first trimester. Exercising in supine position may affect blood flow to baby as the enlarging uterus can compress the vena cava reducing cardiac output, reducing O2 delivery to both baby and mother.
If dizziness or light headedness occurs, get the mother to roll onto her left side immediately, and slowly sit up.
Separation of rectus abdominis
During pregnancy, the growing uterus can often cause the rectus abdominis muscles to stretch and separate in the centre. This is called diastasis rectus abdominis.
Diastasis recti is very common during and following pregnancy. This is because the uterus stretches the muscles in the abdomen to accommodate the growing baby.
One study found that up to 60 percent of women may experience diastasis recti during pregnancy or postpartum.
The condition isn’t limited to pregnancy, though. It can affect anyone, including newborn babies and men. In some cases, it can result from lifting heavy weights incorrectly or performing excessive or unsafe abdominal exercises.
During pregnancy, to minimise chance of diastasis rectus abdominis avoid crunching exercises. Even though a strong core and pelvic floor muscles help with delivery, there are other core strengthening exercises that can help such as a side plank and birddogs.
Exercises to avoid
There are some exercises and positions that carry higher risks. it is important to be aware of these activities and modify exercises accordingly.
| EXERCISE | REASONS TO AVOID |
|---|---|
| Abdominal exercises | Abdominal exercise should be avoided for those mothers who have separation of the rectus abdominus (typically occurring in 30% of women). |
| Heavyweight training | Heavy weight training places large amounts of stress of the muscles and bones and tends to promote clients to hold their breath. This causes a rise in blood pressure (which is already elevated due to being pregnant) which can promote dizzy spells and result in fainting. |
| Complex yoga poses |
Increased tendency to hold the breath, elevating BP and promoting dizzy spells which could result in fainting. Promote further exhaustion through performing complex muscular movements and poses. |
| Exercises in the supine position (lying on your back) | These should be avoided, particularly after the first trimester, due to the uterus compressing the vena cava (major blood vessel) and affecting blood flow, and there for oxygen and nutrient supply, to the foetus. |
| Exercises in the prone position (lying on your stomach) | A number of associations such as the National Academy of Sports Medicine (NASM) have advised avoiding exercises which involve the mother directly lying on her stomach. These can place Increased pressure directly onto the unborn child which may also be uncomfortable as the baby bump begins to grow. |
| Activities which have a high chance of falls such as horse riding, cycling, or quad biking. | Activities like this should be avoided where possible, to decrease the risks of accidents or injury to both the mother and unborn child. Cycling, especially during the second and third trimesters, should be avoided because of changes in balance and the risk of falling. |
| Activities which affect the centre of gravity (COG) |
Participation in activities which require rapid movements, changes in direction and levels of balance and coordination should be avoided as these will be increasingly challenging for a pregnant mother and pose a greater increased risk of falls. Exercises should be done on a wooden floor or tightly carpeted surface to reduce shock and provide a sure footing, further reducing the potential for loss of balance and falls. |
| Activities conducted at high altitude (typically above 2,500m) | Activities performed at high altitude which result in altitude sickness can reduce foetal oxygen supply posing harm to the development of the unborn child. These can also induce shortness of breath, chest pain, promoting light-headedness, and weakness. These should be avoided, particularly in non-acclimatised women. |
| Power/plyometric training | Training that includes ballistic movements such as jerky, bouncy motions should be avoided as relaxin’s effect on the joints and their supporting ligaments, poses a greater risk of damage or injury. |
| Activities involving deep flexion or extension of joints | These should be avoided due to connective tissue laxity and the increased risk of joint injury. |
Training recommendations during pregnancy
If a pregnant woman has exercised before becoming pregnant, it is most likely that they will be able to stick to the same routine they were originally applying. Pregnancy is not, however, the time to test the boundaries or pick up a new exercise activity, especially if it is high intensity or risky. It is important to remember that pregnancy places a large amount of responsibility on the individual who is pregnant, and it is vital to be best informed. Women who have not exercised prior to pregnancy, or are newcomers to exercise in general, should discuss an exercise programme with their GP, obstetrician, or midwife.
During pregnancy, women can continue to exercise and derive health benefits even from mild to moderate exercise routines. Moderate intensity means a woman can comfortably hold a conversation throughout the workout, without pausing for a breath. RANZCOG (The Royal Australian and New Zealand College of Obstetricians and Gynaecologists) states that women should get at least 150-300 minutes of moderate-intensity aerobic physical exercise per week. This equates to approximately 30 minutes of exercise on most days, without exceeding 60 minutes or more in on session, unless the intensity is relatively light. Regular exercise, at least 3 times per week is preferable to intermittent activity.
Exercise suggestions
Non-weight bearing exercises such as cycling or swimming will minimise the risk of injury and facilitate the continuation of exercise during pregnancy. Weight-bearing exercises such as hiking, jogging, walking, or climbing stairs may under some circumstances be continued at intensities similar to those prior to pregnancy. Depending on the type of exercise performed, pregnant women should stop exercising when fatigued and not exercise to exhaustion.
Some exercises which may be considered safe, even for beginners include:
- Swimming
- Jogging
- Cycling – outdoors or on a stationary bicycle
- Walking
- Pilates
- Muscle strengthening exercises, including pelvic floor exercises
- Exercise in water (aquarobics)
- Yoga, stretching, and other floor exercises
- Pregnancy exercise classes
Water-based activities may be beneficial during pregnancy. Water can decrease the mothers heart rate by up to 10 bpm and cause foetal heart rate changes to be less dramatic. This occurs as water conducts heat 25% faster than air so core temperature will not rise as quickly. Balance and co-ordination concerns are eliminated because of the support of the water. Pressure of water also decreases the venous pooling effect helping to reduce the effects of swelling during pregnancy.
Additional benefits for water-based activity include:
- Control of body weight
- An increase in the level of amniotic fluid
- Decreased need for analgesia (painkillers)
- Decreased levels of oedema Increased diuresis
- A substantial reduction in arterial pressure
- Reduced impact on articulations
- A reduced amount of back pain
- A reduction in postpartum depression
- Psychological benefits (improved well-being, satisfaction, self-confidence, and body awareness)
The cool-down phase of a workout should be gradual, as foetal risk may be greatest immediately after the conditioning portion of a workout.
Contra-indications for exercise
The recommendations discussed in this subtopic are intended for women who do not have any additional risk factors for adverse maternal or perinatal outcomes. Several medical and obstetric conditions may require modification of these guidelines. The following conditions should be considered contraindications to exercise during pregnancy and require medical clearance prior to undertaking physical activity:
- Pregnancy-induced hypertension
- Pre-term rupture of membranes, pre-term labour during the prior or current pregnancy or both
- Incompetent cervix
- Persistent second or third trimester bleeding
- Intrauterine growth retardation
- Multiple gestations
Exercise can be uncomfortable, but it should not cause serious implications for overall health. It is important to stop exercise immediately and consult with a doctor, obstetrician, or midwife if at any time during the exercise session the women experiences or feels:
- Faint
- Dizzy
- Unusually short of breath
- Vaginal bleeding
- Palpitations
- Blurred vision
- Headache
- Chest pain
- Unusual muscle weakness
- Calf pain or swelling
- Decreased foetal movement
- Amniotic fluid leakage

Overview
In this subtopic, we focus on exercise for obese populations. You will learn about:
- Overview of obesity
- Benefits of exercise
- Signs and symptoms of obesity
- Possible risks
- Training recommendations
People with obesity are a special population group because they are at increased risk for a wide range of health problems, including cardiovascular disease, type 2 diabetes, high blood pressure, certain types of cancer, and joint problems. These health issues can significantly impact their ability to participate in physical activity and may require modifications to exercise programming.
Clients with obesity may face unique challenges when it comes to exercise, such as limited mobility, decreased flexibility, and increased risk of injury. Personal trainers who work with clients with obesity need to be knowledgeable about these challenges and be able to modify exercises to accommodate the client's needs while still providing an effective workout.
It's also important to recognise that weight loss is not the only goal for people with obesity.
Exercise can provide numerous health benefits, such as improved cardiovascular function, increased strength and flexibility, and improved mental health. Personal trainers who work with clients with obesity should focus on creating a safe and supportive environment that emphasises overall health and wellbeing, rather than just weight loss.
What is obesity?
Overweight and obesity are defined as abnormal or excessive fat accumulation that presents a risk to health.
Obesity is caused by an increase in size and amount of fat cells in the body. The number of fat cells is typically determined via genetics, established in the early years, and does not alter significantly throughout adult life. The size of fat cells, however, can be altered through diet and lifestyle modifications. Unfortunately, fat cells, like all cells of the body, have a memory and will typically aim to return to the size they remember/feel comfortable at.
New Zealand’s obesity statistics

NEW ZEALAND HAS THE THIRD HIGHEST ADULT OBESITY RATE IN THE OECD, AND OUR RATES CONTINUE TO INCREASE.NZ Ministry of Health
The New Zealand Health Survey 2020/21 reported the following statistics for adults:
- Around 1 in 3 adults (aged 15 years and over) were obese (34.4%)
- The prevalence of obesity among adults differed by ethnicity, with 71.3% of Pacific, 50.8% of Māori, 31.9% of European/other and 18.5% of Asian adults obese
- Adults living in the most socioeconomically deprived areas were 1.6 times as likely to be obese as adults living in the least deprived areas
- The overall prevalence has remained relatively stable since 2012/13, however, there was an increase between 2011/12 and 2019/20 for adults aged 45–54 years and 55–64 years
The survey found the following childhood obesity statistics:
- Around 1 in 8 children (aged 2–14 years) were obese (12.7%)
- The prevalence of obesity among children differed by ethnicity, with 35.3% of Pacific and 17.8% of Māori, 10.3% of European/other, and 6.6% of Asian children obese
- Children living in the most socioeconomically deprived areas were 2.5 times as likely to be obese as children living in the least deprived areas
Benefits of exercise for people with obesity
Exercise can provide significant health benefits for individuals with obesity and is an important component of any weight loss or management programme. Benefits of exercise for people with obesity include:
- Weight loss: Exercise can help individuals with obesity lose weight by burning calories and reducing body fat.
- Improved cardiovascular health: Exercise can help reduce the risk of heart disease and stroke by improving blood pressure, cholesterol levels, and overall cardiovascular function.
- Increased muscle mass: Exercise can help build and maintain muscle mass, which can improve metabolism and help burn more calories at rest.
- Improved insulin sensitivity: Exercise can help improve insulin sensitivity and glucose metabolism, which can reduce the risk of developing type 2 diabetes.
- Improved mental health: Exercise has been shown to improve mood, reduce stress and anxiety, and improve overall mental health.
- Better sleep: Exercise can improve sleep quality, which is important for overall health and wellbeing.
- Increased energy and endurance: Regular exercise can help improve energy levels and endurance, making it easier to perform daily activities and exercise for longer periods of time.
Signs and symptoms
Some common signs and symptoms of obesity include:
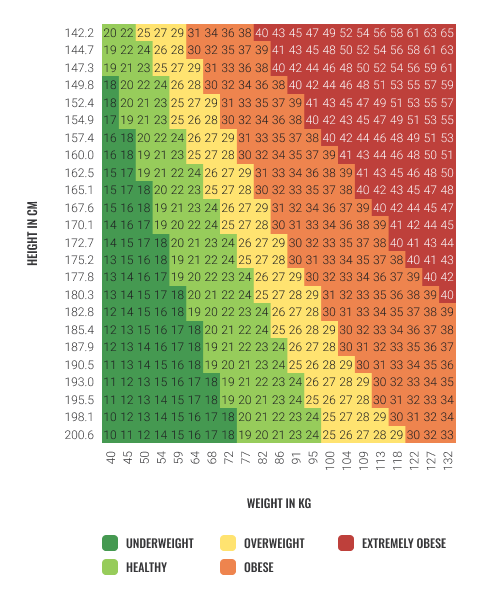
- Increased body weight: People with obesity typically have a body mass index (BMI) of 30 or above.
- Increased body fat: Excessive body fat, particularly around the waist, hips, and thighs, is a common sign of obesity.
- Breathlessness: People with obesity may experience shortness of breath or difficulty breathing, particularly during physical activity.
- Joint pain: The extra weight on the joints can lead to pain and inflammation.
- Fatigue: Carrying around excess weight can be physically tiring, leading to fatigue and a lack of energy.
- Sleep apnoea: Obesity can cause sleep apnoea, a condition in which a person stops breathing temporarily during sleep.
- High blood pressure: Obesity can lead to high blood pressure, which can increase the risk of heart disease and stroke.
- Diabetes: Obesity is a risk factor for type 2 diabetes, a condition in which the body becomes resistant to insulin.
Not all people with obesity will experience all these symptoms, and some people may not experience any symptoms at all. It's essential to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
How is obesity measured?
Measuring it accurately can be challenging, as different methods may have variances in reliability. Some commonly used methods for measuring excessive body fat include body girth, skinfold thickness, bioimpedance, hydrostatic weighing, waist-to-hip ratio, body mass index (BMI), and weight-to-height ratio.
Medical and health professionals often use BMI and waist circumference as initial measures to diagnose and monitor overweight and obesity in patients. However, it's important to note that these measurements are crude and do not account for other body tissue types such as muscle tissue. Therefore, BMI and waist-to-hip ratio should be used as a guide rather than a conclusive diagnostic tool.
BMI is calculated by dividing an individual's weight in kilograms by their height in meters squared. For example, if someone weighs 55kg and is 163cm tall, their BMI would be calculated as follows:
BMI = 55 ÷ (1.63 x 1.63) = 20.7
The resulting figure can be cross-checked against a chart to determine if an individual's weight falls within an appropriate range based on their height. It's essential to interpret these measurements together with other factors such as overall health, lifestyle, and medical history to determine the most appropriate course of action.
Contributing factors
Obesity is a complex condition that can result from various contributing factors, including lifestyle, genetics, environment, medical conditions, and medication. As a personal trainer, it is important to understand these factors and educate clients on their potential impact on weight gain.
The following are some examples of factors that can contribute to obesity:
- Diet: This includes the type of food, portion size, and the consumption of high-fat and high-sugar foods, as well as increased alcohol intake and food varieties.
- Lack of exercise: A sedentary lifestyle can lead to decreased energy output and contribute to weight gain.
- Environmental factors: This includes advertising, competitions related to fast food options, affordability of fast food, and peer influence.
- Genetics: Genetic factors can increase a person's predisposition to obesity.
- Medical conditions: Certain medical conditions can contribute to weight gain, such as hypothyroidism, Cushing's syndrome, and polycystic ovary syndrome.
- Medication: Certain medications, such as antidepressants and corticosteroids, can lead to weight gain.
- Stress or depression: Stress and depression can lead to emotional eating and increased food consumption.
- Change of routine: Disruptions in daily routine can lead to increased stress and changes in eating patterns.
Obesity is not solely attributed to one of these factors, but rather a combination of several. Therefore, personal trainers should take a holistic approach to their clients' health and wellbeing, and work with them to develop a plan that addresses all contributing factors to achieve optimal results.
Health risks and possible treatment options
The prevalence of obesity is a growing concern due to the serious health implications that can arise from increased levels of adipose tissue. These complications can include, but are not limited to, diabetes, cancer, high blood cholesterol, heart disease, atherosclerosis, high blood pressure, sleep disorders, and death.
Treatment options for obesity will vary depending on the individual's specific circumstances, including the underlying cause and the severity of the condition. Some examples of possible treatments include:
- Developing a healthy eating plan
- Increasing physical activity
- Weight loss medications such as orlistat, phentermine, liraglutide, and naltrexone/bupropion
- Weight loss surgery
It is important to note that while a balanced diet and exercise are typically the initial forms of treatment, not all cases are simple, and additional health concerns may require a specialised plan of action.
It is essential to approach conversations about obesity with care, kindness, and respect, as the condition can affect an individual's physical, social, emotional, and mental wellbeing. You should remember that they are not there to diagnose, but rather to discuss health matters and offer guidance. If you feel uncomfortable discussing such matters or are unsure how to guide a client, you should refer the client to a professional who can help them. Ultimately, clients should have the autonomy to make their own decisions about their health, and personal trainers should support them in achieving their goals while maintaining their overall wellbeing.
Possible risks
Clients with obesity may face certain risks when engaging in fitness testing and an exercise programme. As a personal trainer, you need to be aware of these risks and take appropriate precautions to ensure the safety of your clients. Risks include:
- Cardiovascular risks
- Musculoskeletal risks
- Respiratory risks
- Psychological risks
Cardiovascular risks
Clients with obesity may have underlying cardiovascular conditions that put them at risk for a heart attack or other cardiac events during exercise. Personal trainers should take precautions by assessing their client's medical history, monitoring their heart rate and blood pressure during exercise, and gradually increasing exercise intensity over time.
Musculoskeletal risks
Excessive weight can put a strain on joints and bones, leading to musculoskeletal injuries during exercise. Personal trainers should pay attention to their clients' form and technique during exercises to prevent injury and modify exercises as needed to avoid overloading certain joints or muscle groups.
Respiratory risks
Increased body weight and reduced lung capacity can result in obese clients having difficulty breathing during exercise. Personal trainers should monitor their clients' breathing patterns during exercise and modify the intensity or duration of exercise if breathing becomes difficult.
Psychological risks
Clients with obesity may feel self-conscious or anxious about their body during exercise, which can negatively affect their motivation to continue with the exercise programme. Personal trainers should create a supportive and non-judgmental environment to help their clients feel comfortable and confident during exercise.
To minimise these risks, conduct a thorough pre-screening, modify exercises as needed, and closely monitor clients' progress and health status throughout the programme.
Training recommendations for clients with obesity
Personal trainers need to be mindful of the unique needs and limitations of clients with obesity. You need to design exercise programmes that are safe, effective, and sustainable. To achieve these goals, consider modifying FITT variables. Let's take a closer look at some specific training recommendations for clients with obesity.
Frequency
Clients should engage in aerobic exercises for more than 5 days per week to maximise caloric expenditure.
Intensity
Moderate to vigorous-intensity aerobic exercises should be encouraged. Vigorous exercise is not appropriate for very obese clients with a BMI over approximately 35 kg/m2.
If clients choose to incorporate vigorous intensity activity into their programme, it should be done gradually and after an initial 4-12 week period of moderate-intensity activity.
Time (duration)
For the prevention of obesity, clients may need 45 to 60 minutes of moderate intensity aerobic activity each day, unless they also reduce their energy intake.
For clients who are already overweight or obese, a volume of 45 to 60 minutes of moderate-intensity activity per day, corresponding to approximately 225 to 300 minutes/week of moderate-intensity physical activity or lesser amounts of vigorous physical activity, is recommended.
Type
Brisk walking is an excellent form of physical activity for overweight and obese individuals, and for those with joint problems, non-weightbearing moderate-intensity physical activities like cycling, swimming, and water aerobics should be encouraged.
Resistance training is highly recommended to build muscle mass and increase metabolic rate. Resistance training exercises can be modified by using lighter weights or resistance bands, and focusing on higher repetitions and longer rest periods to prevent fatigue and injury.
Bodyweight exercises such as squats or lunges can be modified by using a chair or wall for support, or by reducing the range of motion to prevent discomfort or pain.
Exercises that require lying on the back or stomach can be uncomfortable for some obese individuals, so modifications such as seated or standing versions of exercises can be used instead.
Exercises should also be familiar to the client to increase adherence.
Safety considerations
Personal trainers should be aware of potential risks associated with exercise for clients with obesity, including joint problems, cardiovascular complications, and the potential for heat exhaustion. Clients should be monitored closely for signs of fatigue or discomfort during exercise, and exercises should be modified or adjusted as needed to ensure safety and prevent injury. Also be aware of potential psychological barriers that may impact adherence to exercise programmes and provide appropriate support and encouragement.

Overview
In this subtopic, we focus on exercise for diabetic populations. You will learn about:
- Overview of diabetes
- Benefits of exercise
- Signs and symptoms of diabetes
- Possible risks
- Training recommendations
Clients with diabetes are a special population group because exercise can have a significant impact on their blood glucose levels. Exercise can cause a drop in blood glucose, which can be dangerous for people with diabetes who are taking certain medications such as insulin or sulfonylureas. On the other hand, exercise can also cause blood glucose to rise in some people with diabetes due to hormonal responses, such as the release of stress hormones.
Therefore, it is important for personal trainers to have a solid understanding of diabetes, its complications, and the various medications and treatments, and to work with their clients with diabetes and their healthcare team to develop a safe and effective exercise programme that takes these factors into consideration.
What is diabetes?
Diabetes is a medical condition where the level of glucose in the blood is too high. There are 2 types of diabetes:
- Type 1: The insulin-making cells in the pancreas are destroyed and cannot make enough insulin. It is caused by genetic and environmental factors. It is not caused by eating too much sugar or any other foods.
- Type 2: The body is not able to use insulin effectively due to resistance to insulin. Genetics can be a risk factor, but the major risk factor is being overweight. The risk can be lessened by being physically active and eating a healthy diet.
New Zealand’s diabetes statistics
Over 250,000 people in New Zealand have been diagnosed with diabetes. It is more common among Māori, Pacific and South Asian people and the rate of both type 1 and 2 diabetes is increasing, especially lifestyle-related type 2 diabetes.
Type 1 diabetes is less common than type 2 diabetes. Of the people with diabetes in NZ, 90 – 95% have type 2 diabetes.
Type 2 diabetes usually develops in adults but it is becoming more common in young people. It is linked to, but not always caused by, obesity.
Māori, Pacific and South Asian people are more likely to have type 2 diabetes and develop complications of the condition.
Pregnant people can also develop gestational diabetes. About 50% of people with gestational diabetes will go on to develop type 2 diabetes in their lifetime (Diabetes, Ministry of Health, 2022).
Benefits of exercise for people with diabetes
Exercise can have several benefits for people with diabetes, including:
- Improved blood sugar control: Exercise can lower blood sugar levels and increase insulin sensitivity, allowing the body to use insulin more effectively.
- Weight management: Exercise can help with weight loss or weight management, which is important for people with type 2 diabetes who are often overweight or obese.
- Improved cardiovascular health: Exercise can help lower blood pressure, improve blood lipid levels, and reduce the risk of heart disease, which is a common complication of diabetes.
- Increased muscle strength and flexibility: Exercise can help improve muscle strength and flexibility, which can help with everyday activities and reduce the risk of falls and injuries.
- Improved mood and mental health: Exercise can help reduce stress and anxiety, improve mood, and increase feelings of wellbeing.
Signs and symptoms
The signs and symptoms of diabetes include:
- Frequent urination: When there is too much glucose in the blood, the kidneys have to work harder to filter and absorb the excess sugar. If they can't keep up, the excess sugar is excreted into the urine, dragging fluids from your tissues along with it.
- Excessive thirst: When you're urinating more frequently, you're also losing more fluids. The body will try to replace the lost fluids by increasing your thirst.
- Increased hunger: When insulin is not working effectively, or there is not enough of it, your body will crave more food as it is not getting the energy it needs from glucose.
- Fatigue: When glucose cannot enter the cells and provide energy, you may feel tired or fatigued.
- Blurred vision: High blood sugar levels can cause the lens of the eye to swell, which can result in blurred vision.
- Slow-healing wounds: High blood sugar levels can affect blood circulation, which can slow down the healing process of wounds and infections.
- Numbness or tingling in the feet or hands: High blood sugar can damage nerves, which can cause numbness, tingling, or a burning sensation in the feet or hands.
It is important to note that some people with type 2 diabetes may not experience any symptoms, which is why regular check-ups and blood sugar monitoring are important for early detection and management of the condition.
Possible risks
Exercise is generally safe and beneficial for people with diabetes, but there are some risks that personal trainers should be aware of when working with clients with diabetes. Here are some possible risks associated with exercise for clients with diabetes:
- Hypoglycaemia (low blood sugar): Exercise can lower blood sugar levels, which can lead to hypoglycaemia if the client's blood sugar is already low or if they have taken too much insulin or diabetes medication. Symptoms of hypoglycaemia include dizziness, confusion, weakness, sweating, and tremors.
- Hyperglycaemia (high blood sugar): If the client's blood sugar is already high, exercise can cause it to rise even higher. Symptoms of hyperglycaemia include increased thirst and urination, fatigue, blurred vision, and headaches.
- Cardiovascular complications: Clients with diabetes are at an increased risk of cardiovascular disease, so it is important to monitor their heart rate, blood pressure, and symptoms of angina (chest pain or discomfort) during exercise.
- Diabetic retinopathy: Clients with diabetes are at an increased risk of developing diabetic retinopathy, which is damage to the blood vessels in the eyes. Vigorous exercise can increase blood pressure and strain on the eyes, which can worsen diabetic retinopathy.
- Neuropathy: Clients with diabetes are at an increased risk of developing neuropathy, which is damage to the nerves that can cause numbness, tingling, and pain in the feet and legs. High-impact exercises and exercises that put pressure on the feet (such as running) can worsen neuropathy.
Personal trainers working with clients with diabetes should be aware of these potential risks and take steps to minimise them, such as monitoring blood sugar levels before, during, and after exercise, modifying exercises as needed to reduce strain on the eyes and feet, and ensuring that the client has easy access to glucose tablets or snacks in case of hypoglycaemia. It is also important to work closely with the client's healthcare provider to develop a safe and effective exercise program.
Training recommendations for clients with diabetes
When working with diabetic clients, it is important to start with a thorough medical history and physical examination to assess any potential risks or contraindications to exercise. Personal trainers should work with the client's GP or diabetes educator to develop a safe and effective exercise plan.
Frequency
Frequency of exercise should also be considered. It is generally recommended that clients engage in at least 3-5 sessions of aerobic exercise per week, with resistance training at least 2-3 days per week. Clients should also be encouraged to engage in regular physical activity throughout the day, such as taking short walks or doing light stretching at regular intervals.
Intensity
Intensity of exercise is another consideration. Moderate- to vigorous-intensity aerobic exercises are encouraged, as they can help improve glucose control and reduce cardiovascular risk factors. However, clients with uncontrolled blood glucose levels may need to start with lower intensity exercise until their blood glucose is better managed. Trainers should monitor blood glucose levels before, during, and after exercise and adjust the intensity as necessary.
Time
Duration of exercise is also important. To prevent or manage diabetes, clients may need at least 150 minutes of moderate-intensity aerobic activity per week, such as brisk walking, cycling, or swimming. This can be broken down into shorter sessions of at least 10 minutes throughout the day. Resistance training sessions should last no longer than 60 minutes to avoid excessive stress on the muscles and joints.
Type
Type of exercise is an important consideration. Low-impact exercises such as walking, cycling, and swimming are generally recommended to minimize stress on the joints and avoid injury. Resistance training is also beneficial for building muscle mass, improving insulin sensitivity, and increasing metabolic rate. Exercises should be familiar to the client, and trainers should avoid prescribing jarring activities or heavy weight-bearing exercises.
Managing blood glucose levels
Trainers should also be aware of potential complications that may arise during exercise, such as hypoglycaemia or hyperglycaemia, and have a plan to address these issues. Clients should be educated on the signs and symptoms of hypoglycaemia and hyperglycaemia and advised to monitor their blood glucose levels regularly. Trainers should also ensure that clients have access to glucose tablets or other sources of quick-acting carbohydrates during exercise in case of hypoglycaemia.

Overview
In this subtopic, we focus on exercise for clients with cardiovascular disease. You will learn about:
- Overview of cardiovascular disease
- Benefits of exercise
- Signs and symptoms of cardiovascular disease
- Possible risks
- Training recommendations
Clients with cardiovascular disease are a special population group because their condition may make them more vulnerable to complications during physical activity. Cardiovascular disease refers to a range of conditions that affect the heart and blood vessels, including coronary artery disease, heart failure, arrhythmias, and peripheral artery disease. These conditions can reduce the heart's ability to pump blood, impair blood flow to the extremities, and increase the risk of heart attack or stroke.
When designing an exercise programme for clients with cardiovascular disease, it is important to consider their individual health status and exercise capacity. Exercise can be an effective way to improve cardiovascular health and reduce the risk of further complications. However, the intensity, duration, and frequency of exercise must be carefully tailored to the individual's needs to avoid exacerbating their condition.
Moreover, cardiovascular disease may be associated with other health conditions, such as diabetes, high blood pressure, or obesity, that can also impact the design of the exercise programme. Personal trainers must be aware of these comorbidities and adjust their exercise prescription accordingly.
Clients with cardiovascular disease may require additional monitoring during exercise to ensure their safety. This can include heart rate and blood pressure monitoring before, during, and after exercise. Trainers must also be aware of the signs and symptoms of potential complications, such as chest pain, shortness of breath, or dizziness, and know how to respond appropriately.
Benefits of exercise for cardiovascular disease
Regular exercise has numerous benefits for clients with cardiovascular disease, including:
- Improved heart health: Exercise can help improve the strength and function of the heart muscle, as well as lower resting heart rate and blood pressure.
- Improved blood lipid profile: Exercise can help lower levels of harmful LDL cholesterol and increase levels of beneficial HDL cholesterol.
- Improved blood glucose control: Exercise can help improve insulin sensitivity, which can lead to better blood glucose control in clients with diabetes or pre-diabetes.
- Weight management: Exercise can help clients achieve and maintain a healthy weight, which is important for reducing cardiovascular risk factors.
- Reduced stress and anxiety: Exercise has been shown to have a positive impact on mental health, including reducing stress and anxiety, which can have a beneficial effect on cardiovascular health.
- Improved quality of life: Regular exercise can improve overall physical fitness and functional capacity, which can lead to an improved quality of life for clients with cardiovascular disease.
Signs and symptoms
Cardiovascular disease (CVD) refers to a range of conditions that affect the heart and blood vessels. Some common signs and symptoms of cardiovascular disease may include:
- Chest pain or discomfort: This is the most common symptom of CVD. It may feel like pressure, fullness, squeezing, or pain in the centre of the chest that lasts for several minutes or comes and goes.
- Shortness of breath: If you feel out of breath doing everyday activities like climbing stairs, walking, or carrying groceries, it could be a sign of CVD.
- Fatigue: Feeling tired or weak, even after a good night's sleep, can be a sign of CVD.
- Dizziness or light-headedness: Feeling faint or dizzy, especially during physical activity, may indicate CVD.
- Heart palpitations: If you feel like your heart is racing, skipping beats, or fluttering in your chest, it could be a sign of CVD.
- Swelling: Swelling in your legs, ankles, or feet may indicate CVD, especially if it's accompanied by fatigue, shortness of breath, or chest pain.
- Nausea or vomiting: Feeling sick to your stomach or throwing up may be a sign of CVD, especially if it's accompanied by chest pain or shortness of breath.
It's important to note that some people with CVD may not experience any symptoms, which is why regular check-ups with a healthcare provider are crucial for early detection and treatment.
Watch for signs of a cardiac event
It is crucial for personal trainers to be able to recognise the signs of a potential cardiac event during exercise, as immediate action can save lives. Warning signs to look out for include chest pain or discomfort, shortness of breath, light-headedness, dizziness, nausea or vomiting, palpitations, and unusual fatigue or weakness.
If a client exhibits any of these symptoms, it is important to stop the exercise immediately and call for emergency medical assistance. Personal trainers should also ensure that they have up-to-date first aid certification and are familiar with the location of any defibrillators in the facility.
Be aware of the client's medical history and any medications they are taking. You should also be familiar with the client's exercise tolerance and progress to avoid overexertion or pushing the client beyond their limits.
It is also important to encourage clients with cardiovascular disease to consult with their healthcare provider before starting an exercise programme and to follow any recommendations or restrictions given by their healthcare provider. A collaborative approach between the personal trainer, client, and healthcare provider can help ensure safe and effective exercise for clients with cardiovascular disease.
Possible risks
Exercise can pose some risks for clients with cardiovascular disease, particularly if they have not undergone a proper medical evaluation or are exercising beyond their physical capacity. Some of the possible risks include:
- Cardiac events: Clients with cardiovascular disease are at a higher risk of experiencing a cardiac event, such as a heart attack or arrhythmia, during exercise. This risk can be reduced by ensuring that clients are adequately screened and that their exercise intensity and duration are appropriately managed.
- Blood pressure fluctuations: Exercise can cause significant fluctuations in blood pressure, particularly in clients with cardiovascular disease. This can be particularly problematic for clients with hypertension, as exercise can cause blood pressure to rise to dangerous levels. Personal trainers should be aware of these risks and should monitor blood pressure regularly during exercise sessions.
- Muscle and joint injuries: Clients with cardiovascular disease may have reduced flexibility and mobility, which can increase their risk of musculoskeletal injuries during exercise. Personal trainers should design exercise programmes that are appropriate for each client's level of fitness and mobility.
- Dehydration: Dehydration can be particularly problematic for clients with cardiovascular disease, as it can exacerbate existing medical conditions. Personal trainers should encourage clients to drink plenty of water before, during, and after exercise sessions to prevent dehydration.
- Medication interactions: Many clients with cardiovascular disease take medications that can interact with exercise, particularly blood thinners and beta-blockers. Personal trainers should be aware of these potential interactions and should consult with the client's healthcare provider before designing an exercise programme.
Training recommendations for clients with cardiovascular disease
Newly qualified personal trainers should not attempt to train clients with cardiovascular disease without adequate support and supervision from experienced trainers. This is because clients with cardiovascular disease require specialised care, and training them improperly or without proper supervision can lead to serious health risks.
It is important for personal trainers to recognise their own limitations and seek guidance when necessary to ensure the safety and wellbeing of their clients.
Here are some general training recommendations for clients with cardiovascular disease:
Obtain medical clearance
Before starting any exercise programme, clients with cardiovascular disease should obtain medical clearance from their GP. This will help to determine any specific exercise limitations and to ensure that the program is safe and appropriate for the individual.
Gradual progression
Clients with cardiovascular disease should start with low-intensity exercise and gradually progress to higher levels of intensity and duration. This will help to avoid any sudden increases in workload that may lead to cardiovascular events.
Aerobic exercise
Aerobic exercise is beneficial for clients with cardiovascular disease as it helps to improve cardiovascular function and reduce cardiovascular risk factors. Examples of aerobic exercise include brisk walking, cycling, swimming, and rowing.
Resistance exercise
Resistance exercise is also beneficial for clients with cardiovascular disease as it helps to improve muscle strength, endurance, and functional capacity. However, resistance exercise should be performed with caution and under the guidance of a qualified trainer to avoid any sudden increases in blood pressure.
Flexibility exercise
Flexibility exercises such as stretching, yoga, and Pilates can be included in the exercise programme to improve range of motion, mobility, and balance.
Monitoring
Clients with cardiovascular disease should be monitored during exercise to ensure that they are not experiencing any adverse symptoms such as chest pain, shortness of breath, or dizziness.
Individualised programme
Exercise programmes for clients with cardiovascular disease should be individualised based on the client's medical history, current fitness level, and exercise preferences.
In addition to exercise, lifestyle modifications such as smoking cessation, weight management, and a heart-healthy diet should be incorporated to reduce cardiovascular risk factors and improve overall health.
It is important to note that exercise programmes for clients with cardiovascular disease should be designed and implemented by qualified trainers with appropriate certifications and experience.

Overview
In this subtopic, we focus on exercise for clients with arthritis. You will learn about:
- Overview of arthritis
- Benefits of exercise
- Signs and symptoms of arthritis
- Possible risks
- Training recommendations
Clients with arthritis are a special population group because arthritis is a chronic condition that affects the joints and causes pain, stiffness, and swelling. Exercise is crucial for managing arthritis symptoms and improving joint function, but it can also be challenging for people with arthritis to engage in physical activity due to their pain and limitations.
Arthritis can affect different joints in the body, and its severity varies among individuals. Some people may have mild arthritis symptoms, while others may have severe joint damage that limits their mobility and physical activity. Personal trainers need to understand the specific limitations and needs of each client with arthritis to design a safe and effective exercise program that improves joint health without exacerbating pain or causing injury.
Clients with arthritis may also have other health conditions or physical limitations that further complicate their exercise programme. So, personal trainers need to have specialised knowledge and training to work with clients with arthritis and adapt exercises to their individual needs and abilities.
Benefits of exercise for clients with arthritis
Exercise can be very beneficial for clients with arthritis in many ways, including:
- Pain relief: Regular exercise can help to relieve joint pain and stiffness, as it helps to strengthen muscles, increase flexibility, and reduce inflammation.
- Improved joint function: Exercise can improve joint function by increasing range of motion, reducing stiffness, and enhancing joint stability.
- Better overall physical function: Exercise can improve overall physical function and reduce disability, helping clients to perform activities of daily living more easily.
- Improved mood: Exercise can improve mood and reduce depression, anxiety, and stress associated with chronic pain conditions like arthritis.
- Improved cardiovascular health: Exercise can help to reduce the risk of cardiovascular disease, which is often higher in clients with arthritis due to increased inflammation.
- Improved bone density: Some types of exercise, such as weight-bearing activities, can improve bone density and reduce the risk of osteoporosis, which is more common in clients with arthritis.
- Weight management: Exercise can help clients with arthritis to maintain a healthy weight or lose excess weight, which can reduce the load on joints and improve overall health.
Overall, exercise can be a powerful tool for managing arthritis and improving quality of life for clients with this condition.
Signs and symptoms
Arthritis refers to a group of diseases that affect the joints, causing pain, stiffness, and swelling. The signs and symptoms of arthritis can vary depending on the type of arthritis and the severity of the condition. Some common signs and symptoms of arthritis include:
- Pain: Arthritis can cause pain in one or more joints, which can be mild or severe.
- Stiffness: Arthritis can make the affected joints stiff, especially in the morning or after sitting or lying down for a long time.
- Swelling: Arthritis can cause swelling and inflammation in the joints, making them appear red and warm to the touch.
- Reduced range of motion: Arthritis can limit the range of motion in the affected joints, making it difficult to move them as freely as before.
- Fatigue: Arthritis can cause fatigue, especially if the pain and stiffness make it difficult to get a good night's sleep.
- Warmth and redness: In some cases, the affected joints may feel warm and appear red.
- Deformity: In severe cases, arthritis can cause the joints to become deformed, which can affect a person's ability to perform daily activities.
Not everyone with arthritis will experience all these symptoms, and the symptoms may come and go over time.
Possible risks
While exercise can provide many benefits for clients with arthritis, there are also some potential risks to be aware of. These may impact exercise adherence and attitude towards exercise. Here are some possible risks of exercise for clients with arthritis:
- Joint pain: Depending on the type and severity of arthritis, certain exercises may cause pain in the affected joints.
- Joint damage: Overuse or improper exercise technique can lead to joint damage and exacerbate arthritis symptoms.
- Falls: Clients with arthritis may have a higher risk of falls due to joint pain, stiffness, and balance issues.
- Fatigue: Clients with arthritis may experience fatigue, which can impact their ability to participate in exercise and increase their risk of injury.
- Cardiovascular issues: Some medications used to treat arthritis can increase the risk of cardiovascular issues, such as heart attack or stroke, during exercise.
Personal trainers should be aware of these potential risks and take steps to minimise them when working with clients with arthritis.
Training recommendations for clients with arthritis
The following are some general training recommendations for clients with arthritis:
- Low-impact exercises: Low-impact exercises such as walking, cycling, swimming, and aquatic exercise can be beneficial for clients with arthritis. These exercises are easier on the joints and can help improve flexibility, strength, and cardiovascular health.
- Strengthening exercises: Resistance training can help improve muscle strength and joint stability, which can help reduce pain and improve mobility. Strength training exercises should be performed 2-3 times per week, focusing on major muscle groups.
- Flexibility exercises: Stretching exercises can help improve joint flexibility and range of motion. Flexibility exercises should be performed daily or at least 2-3 times per week.
- Balance exercises: Balance exercises can help improve balance and reduce the risk of falls, which is important for clients with arthritis who may have joint pain and limited mobility.
- Proper technique: Proper technique is important to reduce the risk of injury and joint pain. Personal trainers should work with clients to ensure proper form and technique during exercises.
- Pain management: Clients with arthritis may experience pain during exercise. Personal trainers should work with clients to develop strategies to manage pain, such as modifying exercises or using heat or ice therapy.
- Progression: Exercise programmes should be designed to gradually increase in intensity and duration to avoid exacerbating joint pain or causing injury. Personal trainers should work with clients to develop a programme that is challenging but manageable.

Overview
In this subtopic, we focus on exercise for clients with asthma. You will learn about:
- Overview of asthma
- Benefits of exercise
- Signs and symptoms of asthma
- Possible risks
- Training recommendations
Clients with asthma are a special population group because they may experience exercise-induced asthma or bronchoconstriction, which can make it difficult for them to breathe during and after exercise. This can make exercise uncomfortable or even dangerous for some individuals with asthma, and it may require special considerations and modifications to their exercise programme.
Individuals with asthma may have a higher risk of other health complications, such as cardiovascular disease, and may require additional precautions when engaging in exercise to prevent exacerbation of their condition.
Benefits of exercise for clients with asthma
Regular exercise can provide several benefits for individuals with asthma, including:
- Improved lung function: Exercise can strengthen the respiratory muscles and improve lung capacity, which can help reduce symptoms of shortness of breath and improve overall breathing ability.
- Improved overall fitness: Regular exercise can help improve overall fitness and endurance, making it easier for individuals with asthma to perform daily activities.
- Reduced stress and anxiety: Exercise can also help reduce stress and anxiety, which can be beneficial for individuals with asthma who may experience symptoms triggered by stress.
Signs and symptoms
Asthma is a chronic respiratory condition characterised by inflammation and narrowing of the airways, which makes breathing difficult.
- Bronchospasms occurs when the muscular lining of the airways undergoes involuntary muscle contractions (spasms) and results with loud laboured breathing.
- Swelling of the lining passages that leads to contraction of the bronchioles (airway branches) limiting the airflow travelling in and out of the lungs.
- Increased production of mucus and phlegm.
The following image illustrates the internal changes which occur within the bronchi and alveoli with asthma. You will note the progression of severity which is demonstrated by the final image where the respiratory tract completely obstructed.
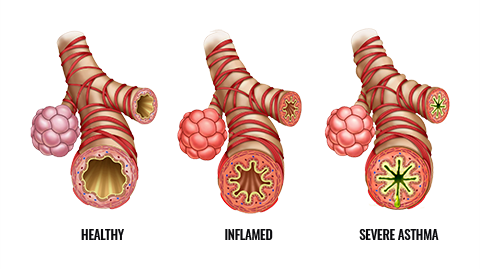
The symptoms of asthma can vary from person to person and can be triggered by a variety of factors including allergens, irritants, respiratory infections (e.g., flu and cold), physical activity or exercise, stress, and cold air. Some common signs and symptoms of asthma include:
- Wheezing: A high-pitched whistling sound when breathing, especially during exhalation.
- Shortness of breath: A feeling of tightness in the chest and difficulty catching your breath.
- Coughing: A persistent cough, especially at night or early in the morning.
- Chest tightness: A feeling of pressure or tightness in the chest.
- Difficulty breathing: Difficulty breathing that may worsen during physical activity or exercise.
- Fatigue: Feeling tired or weak due to difficulty breathing.
Some people may experience symptoms only during specific activities or at certain times of the day.
Possible risks
Clients with asthma may be at risk of having an asthma attack during exercise, especially if their asthma is poorly controlled.
Exercise-induced asthma (EIA) is a common condition in which the airways narrow during or after exercise, causing wheezing, coughing, shortness of breath, and chest tightness. Exposure to certain environmental factors such as cold air, dry air, pollen, and pollution can also trigger asthma symptoms during exercise. In severe cases, exercise-induced bronchoconstriction (EIB) can lead to respiratory failure, which requires immediate medical attention.
In addition to the risk of asthma attacks, clients with asthma may also be at increased risk of injury during exercise. Studies have shown that people with asthma are more likely to experience musculoskeletal injuries, such as sprains, strains, and fractures, possibly due to their reduced lung function and decreased physical activity levels.
Personal trainers need to be aware of these potential risks and take appropriate precautions when working with clients with asthma. It's essential to screen clients for asthma and ensure their condition is well-controlled before starting an exercise programme. Personal trainers should also be prepared to modify or stop the exercise session immediately if the client shows signs of an asthma attack or other adverse reactions.
Training recommendations for clients with asthma
When working with clients with asthma, it is important to take into consideration their individual symptoms and triggers, as well as any medications they are taking. The following are some general training recommendations that can be helpful for clients with asthma:
- Warm up and cool down properly: A proper warm-up before exercise can help reduce the risk of an asthma attack, and a cool-down can help prevent symptoms from worsening after exercise.
- Choose appropriate activities: Some activities, such as swimming or cycling, can be less likely to trigger asthma symptoms than others. Clients should avoid exercising in cold, dry air, or areas with high levels of air pollution.
- Monitor symptoms: Clients with asthma should be encouraged to monitor their symptoms and communicate with their trainer if they experience any issues during exercise.
- Use medications as prescribed: Clients should take their prescribed asthma medications as directed, including any inhalers, to help prevent symptoms from occurring during exercise.
- Gradual progression: Clients with asthma should gradually increase the intensity and duration of their exercise programme, rather than jumping into high-intensity exercise immediately.
- Be prepared: It is important to have an emergency plan in place in case of an asthma attack, including knowing where the client's inhaler is located and how to use it.
- Work with healthcare professionals: For clients with severe asthma, personal trainers may want to work with healthcare professionals, such as the client's doctor, to develop a safe and effective exercise programme for clients with asthma.
