Video Script
Upbeat music plays, visuals of athletes running, swimming, and cycling. Then a beating heart…
Welcome to one of the most fascinating and essential modules in your sport science journey—the cardiovascular system! Whether you're sprinting across a field, pushing your limits in the gym, or recovering after a grueling match, it’s your cardiovascular system that powers every move.
This module dives deep into the heart of human performance—literally. You'll explore the key structures of the cardiovascular system—the heart, blood vessels, and blood—and discover how they work together to keep your body running like a well-oiled machine.
But it’s not just about understanding anatomy. You’ll also learn how we measure cardiac function—things like heart rate, stroke volume, and cardiac output—and why these metrics are crucial for optimising performance and endurance.
Then, we’ll dive into the effects of exercise on the cardiovascular system. Ever wonder how your heart adapts to training? Why athletes have lower resting heart rates? Or how blood flow increases to working muscles? This module will give you the answers—and the science behind them.
We’ll also explore how the cardiovascular system changes across different life stages. From the rapid growth in children, to peak performance in young adults, and the challenges of maintaining cardiovascular health as we age—understanding these changes will help you tailor training and recovery strategies for athletes at every age.
So, are you ready to explore the engine that powers every sport and every athlete? Let’s get started!
The Structures of the Cardiovascular System
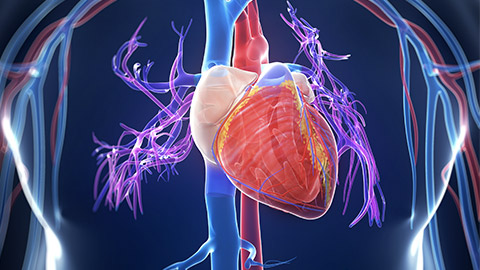
The cardiovascular system (CV System) is integral to every facet of human life and athletic performance. The cardiovascular system (cardio~= heart, vascular~= blood or blood vessels) is composed of three interrelated components:
- The heart
- Blood vessels
- Blood.
The overall role of the cardiovascular system is to provide essential nutrients to the cells and tissues of the body as they require it and remove waste products from body tissues. This is achieved via these three components working in unison.
This topic will guide you through the structure and function of the cardiovascular system, taking an in-depth look at each of its components and their contribution to the maintenance of homeostasis and of course athletic performance. Let’s start by taking a look at each of the three main components of the CV system.
The heart is the “pump” of the CV system. It is surely the most efficient pump in the world. Your heart beats on average about 100,000 times a day. This amounts to over 35 million beats in a year and over 2.5 billion beats in an average lifetime (without ever pausing to rest). Not only that, but the average resting heartbeat also occurs with a similar force to what it would take your hand to squash a tennis ball. There is no other muscle in the body that comes close to that kind of endurance!
The heart has one primary role; to keep pressure within the network of blood vessels that service every cell in the body, so that blood can replenish itself with oxygen and nutrients (for delivery to cells) and remove carbon dioxide and other wastes from tissues.
The brain communicates with the heart to set a rhythm that matches exactly the delivery and removal requirements of the body cells and together they maintain many aspects of homeostasis.
Heart Structure and Location
In the early stages of fetal development, fetus’s heart occupies most of the mid-section. When a baby is born, their heart is the same size as their fist. It continues to grow at the same rate as a person’s clenched fist until adulthood. By adult hood the hear is about the size of a person’s two fists (clasped together). The bigger a person is, the bigger their heart is (just like their fists). An adult heart typically weighs between 250 and 300g.

The heart is located in the centre of your chest, directly under your sternum. Many people believe it is located on the left side of their chest, but when you consider the position of the lungs (either side of the heart) that cannot be true. The heart does tilt towards the left at its inferior end. To get a clear picture of its position, place your left hand (as a clenched fist) directly over the centre of your sternum. Your heart is positioned the same way that your hand and wrist are (angles left).
Before we dive into the internal structures of the heart, there is something we need to get straight. When looking at diagrams of the heart, you must imagine that the heart is in a chest that is facing you. This means that when we talk about structures within the heart that are on the right side of the image, they are actually on the left. Just like when someone is facing you, their right eye and ear are on your left.

The Internal Structures of the Heart
The heart is actually two interconnected pumps that work in unison (one on each side of the heart). The right side of the heart ensures blood makes the trip to the lungs and back, replenishing blood with oxygen and removing CO2 from the body. The left side of the heart contains a strong pump that services the rest of the body, delivering oxygen and nutrients to cells, and removing waste. These two pump circuits are known as:
- The Pulmonary Circuit (to the lungs and back); and
- The Systemic Circuit (to the body cells and back).
Let’s take a look at the structures inside the heart that facilitate this blood flow.
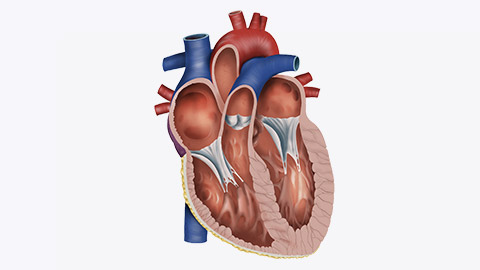
The Chambers of the Heart
Anatomically, our heart is composed of four separate chambers that play their own role in terms of how the heart performs its pumping action. There are two superior chambers (the atria) that receive blood flowing back from the lungs (right atrium) and the rest of the body (left atrium). The two inferior pumping chambers (the ventricles) then push blood out of the heart towards the lungs (right ventricle) and the rest of the body (left ventricle). You can see these chambers in the following diagram:
The atrium and ventricle on each side of the heart are separated by valves that open when blood moves between the atrium and ventricle, then close again when the ventricles pump blood out of the heart. This ensures that blood only ever moves in one direction. Two further valves open as blood is pushed out of the heart towards the lungs and body. It is these valves that produce the sounds of a heart beat we are all familiar with (“lub-dub”)
The two valves between the atria and ventricles (the tricuspid and mitral valves) open simultaneously causing the first sound in the heartbeat (the quieter “lub” sound). Then the two valves that allow blood to exit the heart (the pulmonary and aortic valves) open making the louder “dub” sound. These valves can be seen in the image below.
The walls of the atria and ventricles are made up of cardiac muscle fibres. The walls of the atria are thin as the blood needs little assistance to travel down to the ventricles (with gravity). The walls of the ventricles are thicker as these need to push blood through the vascular networks they feed. As you can see in the image below, the left ventricle has a thicker muscular wall (myocardium) than the right ventricle. This is because the right ventricle only has to move blood between the heart and lungs, while the left ventricle must generate enough force to shift the blood around the entire body.
Watch
The video below recaps the information you have just learned in visual form. It discusses the chambers of the heart, the role of the valves and the muscular walls of the ventricles. It also introduces the nervous system components in the heart that create the heart contractions. Watch the video, then answer the recap questions that follow.
- Video Title: HCL Learning: Structure of the Human Heart
- Watch Time: 2:34
- Video Summary: This video describes the location, structure and function of the human heart, the flow of blood and importance of valves in maintaining the direction of blood flow.
- Post Watch Task: Watch the video, then answer the recap questions that follow.
- Source: YouTube
How the Heart Beats
The heartbeat is produced by auto-conduction. This means the heart has the ability to maintain a heart rhythm on its own (once instructed by the medulla oblongata in the brainstem). As we learned in the nervous system, the autonomic system receives messages from sensory organs alerting it to changes in the body. It will then send signals via motor neurons to the heart to adjust the heart rate to meet any new demands. Once blood flow has met the new requirements the heart rate will settle into a rhythm that the heart can maintain itself (until it receives new messages asking it to change again).
An example of this can be seen when we begin moving. The muscles we use start to consume oxygen and produce CO2. Sensory neurons send impulses to the brain which detects the dropping levels of O2 in the bloodstream. Messages are sent via motor neurons to increase the heart rate. Once O2 levels are brough back up to the desired level, the heart rate plateaus (levels off) and maintains a new rate.
The Conduction System of the Heart
There are a number of key structures in the heart that facilitate a heartbeat. They include:
- The sino-atrial (SA) node – also known as the pacemaker. This node (located at the top of the right atrium) receives impulses from the medulla and sets the heart rate. It sends impulses through the atria causing them to contract (popping open the valves and pushing blood down to the ventricles).
- The atrioventricular (AV) node – Found on the lower wall of the right atrium, this node receives signals from the SA node, delays the impulses for a brief moment (to allow the ventricles to fill with blood), then passes signals to the walls of the ventricles.
- The bundle of His – This bundle of nerve fibres runs down the septum separating the ventricles. It then branches into fibres that wrap around the right and left ventricles.
- The Purkinje fibres – These nerve fibres wrap are spread throughout the myocardium (muscle fibres) surrounding the ventricles and cause the ventricles to contract pumping blood out of the heart.
Watch
This short video explains how these key structures work together to facilitate a heartbeat and explains how the electrical signals relate to the ECG waves we are familiar with (most probably from medical dramas).
Note
The term “depolarisation” is used a lot during this video. This term is used to describe the electrical charge that occurs as impulses arrive at each point of the process. The term depolarisation means an increase in positive charge (electrical stimulus). When this charge reaches the threshold of the muscle fibres, the contraction of the cardiac fibres occurs and the chambers contract.
- Video Title: Cardiac Conduction System and Understanding ECG, Animation
- Watch Time: 3:45
- Video Summary: The cardiac conduction system explained clearly and simply.
- Source: YouTube
Blood vessels are the tubes that transport blood around the body. Some are needed to return blood to the heart, while others leave the heart and distribute blood to the cells of the body. The network of blood vessels is incredibly extensive and complex. It is said that if all blood vessels in a body were laid end to end, they could cover a distance of around 100,000 kilometres. This would circle the earth more than twice!
There are five main types of blood vessels found in the human body:
- Arteries
- Arterioles
- Capillaries
- Venules
- Veins.
Let’s look at each in a little detail.
Arteries
Arteries are the largest of the body’s blood vessels. Their function is to carry blood away from the heart. There are two types of arteries:
- Systemic: These arteries carry blood from the left side of the heart to be distributed to the body tissues. These carry only oxygen rich blood.
- Pulmonary: These arteries carry blood from the right side of the heart to be distributed to the alveoli in the lungs. These carry only blood low in oxygen.
The image below shows the main arteries (in red) leaving the heart. The large, curved artery that sits atop the heart is known as the aorta. You can see how the aorta branches into systemic arteries that send blood upwards to the head and arms, and down behind the heart to carry blood to the internal organs and legs. The Pulmonary arteries can also be seen leaving the left and right side of the heart to the lungs (in blue).
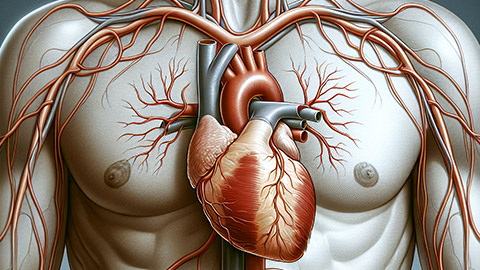
Arteries are high pressure blood vessels as they are directly connected to the heart pumps (the ventricles). This pressure keeps the arteries open, which means if cut or ruptured, blood will spill out quickly leading to life-threatening amounts of blood loss in seconds.
Arterioles
Arteries branch at intervals along their length into smaller arteries and eventually arterioles (which are tiny branches of arteries). Along with smaller the arteries, these are under the control of the sympathetic nervous system and have the ability to constrict (narrow) and dilate (widen) to regulate blood flow to different areas of the body.
The brain is able to redirect blood flow in the body as required to maintain homeostasis. It does this by adjusting the diameter of arterioles. Opening them (known as vasodilation) will increase blood flow to the areas they serve, while narrowing them (vasoconstriction) will reduce blood flow to areas of the body.
An example of this can be seen when we begin exercising. Arterioles delivering the blood to the working muscles and lunges will vasodilate to increase blood flow to these areas, while arterioles leading to the intestines and other areas not so important for exercise will constrict.
The image below shows the redistribution of blood when we move from resting to exercise. Not only does the total volume of blood increase (from 5L-25L of blood pumped by the heart per minute), but the heart lungs and particularly muscle all receive a larger proportion of blood than other organs. This is achieved through the vasodilation and vasoconstriction of the arterioles leading to various organs.
Source: https://journals.physiology.org/doi/full/10.1152/physrev.00037.2021
Capillaries
Capillaries are tiny (extremely narrow) blood vessels, of approximately 5-20 micro-metres (one micro-metre = 0.000001metre) diameter.
There are dense networks of capillaries in most of the organs and tissues of the body. Capillaries are supplied with blood by arterioles. The capillary walls are very thin which allows them to exchange substances and gasses between the blood and the surrounding tissue (for example, oxygen, carbon dioxide, water, salts).
The image below shows the arteriole and capillary network that exists in the human hand.

Venules
Venules are minute vessels that drain blood from capillaries and into veins. Many venules unite to form a vein. Unlike arterioles, venules have no muscular diameter control, instead, they drain blood from capillaries and pass it on into veins for return to the heart.
Veins
Veins transport blood back towards the heart. They feed directly into the atria of the heart. There are two types of veins:
- Systemic: These veins carry blood low in oxygen back to the right atrium of the heart. All veins eventually merge into the superior and inferior vena cava which enter the heart from above and below. The body’s veins can be seen in the image below (in blue).
Source: https://www.healthy-veins.com/spider-veins-varicose-veins/vein-system/
- Pulmonary: These veins carry blood high in oxygen from the lungs back to the left atrium of the heart, so it can be distributed to the cells of the body. These veins can be seen in the image below.
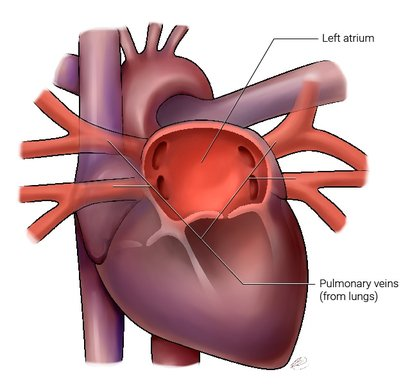
Source: https://www.bartsaf.com/af-and-the-pulmonary-veins/
Watch
This short video recaps the information on the five key blood vessels, it also gives you some additional information about their structure.
- Video Title: Blood vessels – Structure and Function
- Watch Time: 2:12
- Video Summary: This video discusses the structure and function of blood vessels.
- Post-Watch Question: Watch the video then answer the short series of questions that follow.
- Source: YouTube
Answer the following questions to check you understanding of blood vessels.
H5P here
The Pathway of Blood Through the Heart
Blood follows a certain pattern through vessels both into and out of the heart. In anatomical diagrams, you will usually see blood depicted in two colours: blue and red.
- Blue represents deoxygenated blood which indicates a lack of oxygen being carried by this portion of blood and therefore likely heading back to the lungs to receive oxygen inhaled from the environment.
- Conversely, red indicates oxygen-rich blood which has been oxygenated and is now en-route to the tissues and cells of the body to provide an energy source for metabolic activities such as digestion, muscle contraction, and cell communication.
The following image shows the direction of travel of blood both into and out of the heart. The image contains a numbered sequence from blood returning to the heart from the body (1), to leaving and returning from the heart to the lungs (5 & 6), to finally exiting the heart to the body cells (10). Click on the icon near each number to find out what is happening at each stage of the process.
Note
While the image above shows the pathway of a unit of blood through the heart in a sequence, in reality, both sides of the heart are pumping blood at the same time. As the blood leaves the heart through the pulmonary and systemic arteries, it travels through the network of blood vessels described earlier (arterioles, capillaries, venules and veins), before re-entering the heart for another cycle.
The image below shows the two circuits of blood flow (once it leaves the heart), the short pulmonary circuit which takes the blood to the lungs and back via pulmonary arteries, arterioles, capillaries, venules and veins, and the systemic circuit which takes blood to the rest of the body tissues through the systemic arteries, arterioles, capillaries, venules and veins.
Note how the blood in the systemic circuit makes its way to all of the tissues and organs of the body, often performing additional roles to simply delivering oxygen and removing CO2. For example, as the blood passes by the digestive system, it picks up nutrients to deliver to tissues where they are either stored or used as energy. Blood also drops off metabolic wastes as it passes through the kidneys (for removal in urine) and carries heat to the skin to control temperature. The image below shows the cardiovascular systems network of blood vessels interacting with a range of these organs.
The image also shows how the pressure within the cardiovascular system reduces as blood moves further away from the heart.
Recap of Learning So Far
Watch
This video covers all the key learning we have discussed so far from the structure and location of the heart, the pathway of blood through the heart and the two circuits for blood flow in the body. It gives a little more detail about the structure of the heart (not necessary to remember, but interesting). Finally, the video introduces the concept of blood pressure (which is something we will cover in more detail later in the course). Once you have watched the video, answer the questions that follow. Buckle up, this guy has some serious energy!
- Video Title: The heart, part 1 – Under Pressure: Crash course Anatomy & Physiology
- Watch Time: 10:07
- Video Summary: This video discusses the heart’s ventricles, atria, and valves create a pump that maintains both high and low pressure to circulate blood from the heart to the body through your arteries and bring it back to the heart through your veins. You'll also learn what your blood pressure measurements mean when we talk about systolic and diastolic blood pressure.
- Post-Watch Question: Watch the video then answer the series of questions that follow.
- Source: YouTube
Answer the following questions to show your understanding of the learning we have completed to this point.
H5P here
Something Else You Should Know
While blood in the pulmonary circuit only travels to the lungs and back, the blood in the systemic circuit makes its way to all of the tissues and organs of the body, often performing additional roles to simply delivering oxygen and removing CO2. For example, as the blood passes by the small intestines, it picks up nutrients to deliver to tissues where they are either stored or used as energy. Blood also drops off metabolic wastes as it passes through the kidneys (for removal in urine) and carries heat to the skin to control temperature. The image below shows the cardiovascular systems network of blood vessels interacting with a range of these organs.
There are a number of key cardiac measures that are useful to know when embarking on a role in the SRE industry. Cardiac measures can be used to:
- To assess the readiness to exercise of an individual – including both level of fitness and the risk of training an individual.
- To ensure clients are working out at the correct intensities to achieve exercise goals.
- To assess the effectiveness of an exercise program on achieving fitness goals.
The following questions are designed to check your retention of learning about key cardiac measures, what they tell us, and how exercise can adapt them.
H5P here
Let’s take a quick look at the acute and chronic effects of exercise on the key measures we have been discussing.
H5P here
Let’s see how well this information has sunk in. The following task is a set of questions designed to test your retention of the acute and chronic effects of exercise on the heart and cardiac functions.
H5P here
Functions of Blood
- Transport: Blood serves as the body’s main transport system. It carries oxygen from the lungs to working muscles and tissues, while removing carbon dioxide and other waste products from metabolic processes. It also distributes nutrients, hormones, and enzymes to support cellular activity and energy production, which is crucial for athletes.
- Regulation: Blood plays a key role in regulating body temperature, which is vital during exercise when the body generates excess heat. It also helps maintain pH balance and fluid distribution across tissues, ensuring that physiological processes remain stable under varying conditions of physical exertion.
- Protection: Blood is an integral part of the body’s immune system. It contains white blood cells and antibodies that help defend against infections, as well as clotting factors that prevent excessive blood loss during injury, a common concern in sports.
Components of Blood

Blood is comprised of 4 basic components including plasma (the liquid component) and 3 types of blood cells (the solid components).
Watch
This short video discusses the components of blood and their key functions. Watch the video, then answer the questions that follow.
- Video Title: What is Blood?
- Watch Time: 2:23
- Video Summary: This video discusses the function and composition of human blood.
- Post Watch Task: Watch the video, then answer the questions that follow.
- Source: YouTube
As you can see blood plays many important roles in the body. Let’s see what you can remember from the video. Drag and drop the words next to the sentence that they belong with.
H5P here
As the video introduced, blood is a collection of cells (with varying roles) that is suspended in a watery substance called plasma. The proportion of blood made up of cells is known as hematocrit. An average tertiary aged male has a hematocrit level of approximately 42%. An average tertiary-aged female has a hematocrit level of approximately 38%. Hematocrit is largely determined by red blood cell numbers. If males have higher hematocrit, it follows that they also have a higher red blood cell count, so can deliver more oxygen to working muscles per unit of blood.
Blood Pressure
Blood pressure (BP) is the force exerted by circulating blood on the walls of blood vessels during the heart contraction cycle (both contraction and resting phases). A resting blood pressure reading tells us how hard the heart is working at rest.
A minimum blood pressure is required to ensure adequate blood flow to all parts of the body, especially the brain. The term blood pressure generally refers to arterial pressure, i.e., the pressure in the larger arteries. We measure it here as these vessels come directly off the ventricles of the heart, so give the greatest insight to the pressure the heart is creating. As blood moves further from the ventricles, it loses pressure.
Blood pressure is measured in 2 parts.
- Systolic: the maximum pressure reached in the arteries during the ventricular contraction phase of the heartbeat.
- Diastolic: the minimum pressure recorded just before ventricular contraction (resting phases).
Blood pressure is generally recorded as systolic/diastolic (this means systolic over diastolic).
To measure blood pressure, a cuff is placed around the client or patient's arm and inflated. The measurement can be taken manually using a stethoscope or using an electronic device that measures the pressure. Blood pressure is measured in mmHg (millimetres of mercury).
Normal systolic pressure is between 110-130 mmHg and normal diastolic pressure is between 70-80 mmHg (Health Navigator NZ, 2022). The New Zealand Heart Foundation say 120/75 mmHg is the ideal blood pressure for most people.
If your blood pressure is high, your heart works harder with every heartbeat. Constant high blood pressure puts extra strain on your heart and blood vessels. This puts you at higher risk of a heart attack, heart failure, stroke, kidney failure and other health issues. If a person has very high blood pressure, exercise may place them at risk of a cardiac event.
The stroke Foundation of NZ provides the following table that outlines the different categories of blood pressure:
| Systolic | Diastolic |
|---|---|
|
Less than 120 A healthy result, recheck in a year |
Less than 80 |
|
Between 120-129 Monitor as there is a high chance of your blood pressure increasing |
Less than 80 |
|
Between 130-139 A high result, usually treated with lifestyle changes. Medication may be suggested if you have other stroke risk factors |
Between 80-90 |
|
Greater than 140 Usually treated with medication and lifestyle changes |
Greater than 90 |
|
Greater than 180 Needs urgent attention right away |
Greater than 120 |
You will have a chance to take your blood pressure using an electronic cuff in your next face to face lesson. This video shows the process of taking your blood pressure using one of these devices. Please watch this video so you are ready to go in your next lesson.
Watch
- Video Title: Automated Blood Pressure Cuff Use
- Watch Time: 4:09
- Video Summary: This video shows Dr. Evan Matthews explaining how to use an automated blood pressure cuff.
- Post Watch Task: Watch the video in preparation for your next face to face lesson where you will have the opportunity to take your blood pressure with a similar device.
- Source: YouTube
How Does High Blood Pressure Usually Occur?
High blood pressure (hypertension) most often occurs due to cholesterol build up within the arteries. Hypertension is diagnosed when a person records consistent test results of 140/90mmHg or higher. This short video from the NZ Heart Foundation (2015) shows (and explains) how this process occurs. Watch the video and answer the questions that follow.
Watch
- Video Title: Blood Pressure Animation
- Watch Time: 1:40
- Video Summary: This animated video explains what blood pressure is, how it affects your risk of heart attack and stroke, and choices you can make to lower your risk.
- Post Watch Task: Watch the video and answer the short series of questions that follow.
- Source: YouTube
Let’s recap what we know about blood pressure by answering the questions below.
H5P here
The cardiovascular system undergoes significant changes across different life stages, influencing an individual's capacity for physical activity and exercise performance. Understanding these physiological changes is crucial for tailoring training programs to suit the needs and limitations of different age groups.
Let’s take a brief look at how the CV system adapts in each stage of life.
Infants
In infancy, the cardiovascular system is still developing. Infants have a high heart rate, typically between 120-160 beats per minute, to meet their metabolic needs. However, their stroke volume (the amount of blood ejected per heartbeat) is relatively low due to the small size of their heart. The heart muscle is not fully matured, and blood vessels are more elastic, which impacts circulation efficiency.
Interesting fact: Babies are born with 75ml of blood per kilogram of their body weight. This means an 8 pound baby has only 270ml of blood in its whole body!
Children
As children grow, their cardiovascular system begins to mature. Heart rate decreases, with typical resting rates ranging from 70-130 beats per minute, while stroke volume and cardiac output gradually increase due to heart growth. Children also have a greater proportion of elastic tissue in their blood vessels, promoting better circulation. However, their blood pressure remains relatively low compared to adults. While children are obviously capable of physical activity, they are less efficient at off-loading heat, so less able to tolerate prolonged, high-intensity exercise.
Adolescents
Adolescence is marked by a significant increase in heart size and cardiovascular efficiency due to puberty, particularly in males. As the heart becomes larger and stronger, stroke volume and cardiac output increase significantly, enabling better oxygen delivery to muscles during exercise. Resting heart rate continues to decrease, stabilizing between 60-100 beats per minute. Blood pressure rises as blood vessels develop greater resistance. Adolescents can begin to handle more intense exercise, but their cardiovascular system is still adapting to rapid physical changes, making them more prone to the effects of overtraining.
Tip
Keeping hearts healthy from a young age is key for a long, vibrant life. When kids and teens learn good habits, they carry these into adulthood. It’s all about starting early for lasting health. It is important to establish good heart health practices early in life. This involves adults role modeling to kids how to eat healthy and be active. Adolescence and teenage years can bring stress. It is important that teens learn how to deal with stress effectively. Maintaining regular exercise and a healthy diet when teens start to make more of their own choices is key to continuing to look after the heart.
Adults
In adulthood, the cardiovascular system reaches its peak efficiency. The heart is fully developed, and adults generally have a lower resting heart rate (60-80 beats per minute) and higher stroke volume, allowing for efficient blood flow during exercise. Maximal cardiac output reaches its highest levels, which enables adults to sustain prolonged, high-intensity physical activities. Blood pressure remains stable in healthy adults, and the cardiovascular system is well-suited to both endurance and strength-based sports. However, lifestyle factors such as diet, physical activity levels, and stress start to impact cardiovascular health in this life stage.
Tip
Being an adult means dealing with more stress and tasks. It’s important to look after their heart health actively. Making time for exercise, balancing work and life, and getting regular check-ups are key. These visits help find heart problems early. This means they can get treatment sooner. It’s important to keep track of their cholesterol and blood pressure to prevent bigger issues.
Older Adults
As individuals age, the cardiovascular system undergoes several degenerative changes. The heart muscle becomes stiffer and less efficient, reducing stroke volume and cardiac output. Resting heart rate may remain stable, but maximal heart rate declines with age, limiting exercise capacity. Blood vessels lose elasticity, leading to increased blood pressure and higher resistance to blood flow. These changes result in a decreased ability to perform high-intensity or prolonged exercise. Additionally, older adults have a reduced capacity for off-loading heat efficiently and are more susceptible to cardiovascular disease issues like the narrowing of arteries, which can further limit physical performance.
Tip
Older adults should continue to get checked regularly by their health professional and monitor their cholesterol and blood pressure. Other key things older adults can do to maintain heart health are to drink plenty of water and to stay socially connected with others (avoid loneliness).
End of Topic
That is the end of the cardiovascular topic. At the start of this topic, we set out to learn the key structures of the CV system and their functions and how regular exercise affects these. We have also learned about the key measures relating to the CV system and tried a few out on ourselves. The final topic we will cover prior to our next assessment event is the Respiratory System. The remainder of your online learning for this week will cover the basic structures and functions of this system. Enjoy!
