Get ready. We have a packed week of learning for you!
This week, you will explore two more body systems: the nervous system and the digestive system. You will explore the anatomy that makes up these systems as well as their primary functions.
Later, in Anatomy and Physiology, you will continue to discover medications and treatments for hypertension, as well as be introduced to some new cardiovascular disorders.
Tālofa lava, greetings, and welcome back to Patient Care 2.
Body systems review
To kick your learning off this week and to review your understanding of last week’s content, complete this quiz… without referring to your notes. Karawhiua, go on. Give it a go!
How did you get on with these review questions?
Quick quizzes like this are a good way to check what you know and refresh your memory of the previous week's learning. This recall method has also been shown to help you retain information more than if you re-read your notes.
Tip
As we delve further into discussions about body systems this week and beyond, you'll encounter unfamiliar terms, medical terminology, and a lot of beloved acronyms (CV, anyone?).
Take a moment to pause and ensure you grasp their meanings. If you haven’t already, create a personal glossary jotting down these new words with their meanings next to them. This can aid in remembering their correct spelling and definitions for future reference.
Let's now move on to the anatomy of another body system. Don’t be nervous...
Nervous system
The nervous system is like the command centre of the human body. It’s a complex network that transmits signals between the brain, spinal cord and the rest of the body. It’s a busy system as it helps you do things like move, think, feel, dream, blush, bend your fingers and even takes care of the things you don’t think about, like digestion.
Organisation of the nervous system
The following graphic shows how the nervous system is organised. In this session, we will look at each division and how it works together to control the body’s functions.
We will start by looking at the role of the nervous system as a whole before zoning in on the central nervous system and the peripheral nervous system.
Role of the nervous system
The nervous system plays a fundamental role in regulating and coordinating various functions throughout the body. Click the labels or the (+) icon to read more about each of these roles.
The nervous system receives information from outside and inside the body.
Once information is received, it is interpreted.
Responses to information are generated by sending signals to muscles, glands, and other organs, initiating various actions and behaviours.
The nervous system helps maintain homeostasis (remember homeo = similar to / stasis = standing still) by regulating vital functions such as heart rate and breathing.
The nervous system enables voluntary and involuntary movements.
The nervous system is responsible for thinking, learning and memory.
The nervous system is involved in the expression and regulation of emotions.
The nervous system contributes to the body's survival through responses such as fight, flight and rest.
The nervous system is busy! To make its job a little easier, the system breaks these roles up. As you viewed in the diagram above, the nervous system is divided into two main parts that work together – the Central Nervous System (CNS) and the Peripheral Nervous System (PNS). Let’s start with the CNS (another great acronym for your glossary!).
The Central Nervous System (CNS)
The CNS is the core control centre of the body's nervous system and consists of the brain and spinal cord.
Let’s look at each of these.
The brain
 |
|
The brain acts as a control centre by receiving, interpreting and directing sensory information throughout the body. It is made up of neurons (approximately 85 billion!), the basic building blocks of the nervous system, along with glial cells that provide support and protection. The brain is divided into left and right hemispheres, connected by a bundle of nerve fibres that allows communication between the two halves. |
Brain functions
As you can see in the image above, the brain is divided into specific regions responsible for various functions. These are:
- The frontal lobe for decision-making.
- The temporal lobe for auditory processing.
- The parietal lobe for sensory integration.
- The occipital lobe for visual processing.
The brain is also organised into three major divisions. These are:
- The forebrain
- The midbrain
- The hindbrain.
Journal post
Major brain divisions
Carry out your own rangahau (research).
- Create a journal post titled ‘Major Brain Divisions’
- Find out:
- what each of the three major divisions of the brain consists of.
- what their functions are.
- Publish your answers to ‘All course users’. This will allow your tutor to check your response and provide feedback if necessary.
- Save the permalink to your Index of Journal Posts. Remember, you want to get in a good habit of doing this for Level 5 so that it’s a breeze to find your work later.
Introducing the next key player in the CNS... The spinal cord.
The spinal cord
The spinal cord is a cylinder of nerve tissues that extends from the brain down through most of the spinal column's length. Like the brain, it is made up of neurons and glial cells.
Spinal cord functions
The functions of the spinal cord are:
- To transmit signals: transmitting nerve signals between the body and the brain.
- Reflexes: reflex actions are rapid, involuntary responses to information.
- Coordination of movements: the spinal cord plays a significant role in coordinating body movements.
In summary, the brain controls our thinking, feeling, and movement and sends these messages along the spinal cord. From here the messages travel via the peripheral nervous system to the rest of the body. What's the peripheral nervous system? Read on...
The Peripheral Nervous System (PNS)
The second part of the nervous system is the Peripheral Nervous System (PNS). The PNS is a network of nerves that lay outside the CNS.
These nerves transmit information between the central nervous system and the body's organs, muscles, and tissues.
PNS functions
The functions of the PNS are:
- Sensory: nerves transmit sensory information from the body's periphery (skin, muscles, organs) to the CNS.
- Motor: nerves carry motor signals from the CNS to muscles and glands, enabling voluntary and involuntary movements.
- Autonomic: certain peripheral nerves are part of the autonomic nervous system that regulates involuntary bodily functions.
- Reflexes: nerves are involved in rapid and involuntary responses to specific information.
- Communication: nerves serve as communication channels, transmitting signals between the central nervous system and various body parts.
The brain and spinal cord are encased in three layers of membranes called the meninges. Cerebrospinal fluid circulates between two of these layers, delivers nutrients to the structures of the nervous system, and removes wastes from the spinal cord and brain. The cerebrospinal fluid protects and cushions the brain and spinal cord from injury or trauma.
PNS divisions
Up to this point, we've explored the central nervous system (CNS) and the peripheral nervous system (PNS). Now, let's take a brief look at the various divisions within the PNS, which are shown in the diagram that we viewed earlier.
Organisation of the Nervous System
The following is a full diagram of the nervous system. The CNS system is greyed out, so you can focus on the PNS system.
Note how the motor divisions align with the central and peripheral system divisions.
Watch: The Nervous System: Peripheral Nervous System (PNS) (4:07 minutes)
This video clip discusses these major PNS divisions, focusing on sensory neurons, motor neurons and the reflex arc. As you watch, you might like to pause and look at the diagram to help visualise how the PNS divisions fit together. After watching, consolidate your learning and answer the nine pātai (questions) that follow.
How did you go?
If you need some more time on the PNS system or the nervous system as a whole, go back and look at the organisation diagram. You may like to draw this out on a piece of paper or in your notebook and add notes from the video and this content beside each division. Alternatively, put on your independent learner hat and conduct your own research.
Digestive system
The digestive system is made up of several organs and structures that work together to break down food into chemical components that the body can absorb and use.
The digestive system consists of the following:
- Mouth
- Pharynx
- Oesophagus
- Stomach
- Small intestine
- Large intestine
- Rectum
- Anus
- Accessory organs - salivary glands, liver, gallbladder, pancreas
Watch: GCSE Biology - Digestive System #18 (6:02 minutes)
Mātakitaki mai, watch here for an overview of the digestive system – what it does, how it works, what organs are involved and what the system looks like. The video does a great job of breaking the system into digestible pieces for you (pun intended), so make notes, pause the video where needed and draw your own diagram of the system to prepare yourself for the following knowledge check.
Find out how well you stomached the introductory information in the video by completing this five question quiz.
Parts of the digestive system
Now, we will look closer at these parts of the digestive system, focusing on their structure, function and role in digestion. We will also look at some health disorders affecting these parts and their treatments. This week, we will explore the mouth, pharynx, and oesophagus. Let’s begin from the top down.
The mouth
Sometimes called the oral cavity, the mouth is the first part of the digestive system. It is lined with moist tissue called the oral mucosa. This tissue protects the underlying tissues from physical damage, pathogens, and irritants.
The oral mucosa contributes to digestion by helping to lubricate food during chewing and swallowing. It also plays a role in digestion by secreting salivary amylase, an enzyme that chemically breaks down carbohydrates. Sensory receptors in the mucosa contribute to the sense of touch, temperature, and taste, which is important in the process of eating.
Journal post
The mouth - role in digestion
What are the other structures of the mouth that contribute to digestion by physically breaking down food?
- Create a journal post titled ‘The mouth – role in digestion’.
- Carry out your own research to answer the question above.
- Publish your post to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
Disorders
Mouth ulcers are painful sores that can develop on the oral mucosa, including the gums, tongue, and inside of the cheeks. They vary in size and can be round or oval-shaped with a white or yellowish centre and a red border.
Causes include:
- Tissue damage or breaks from:
- accidental biting.
- aggressive tooth brushing.
- dental appliances such as plates and braces.
- burns from hot food or drink.
- Virus-herpes simplex or varicella zoster.
- Nutritional deficiencies such as vitamin B12, iron or folic acid.
- Food intolerance or allergies.
- Immune system issues.
- Medical treatments, such as certain drugs or radiotherapy, to the head and neck area.
- Hormonal changes.
- Stress.
Treatment
Mouth ulcers are common and usually resolve within 1-2 weeks on their own. If they persist longer than three weeks, patients should seek medical advice.
Journal post
Ulcer Scenario
Step into the shoes of a pharmacy technician to assist a patient.
- Carry out your own research to complete the following Documentation tool activity.
- Download and save the completed activity.
- Create a journal post titled ‘Ulcer scenario’.
- Upload the completed activity to your journal post and publish your post to ‘All course users’ so your tutor can review your answers.
And now, we continue our journey down to the next part of the digestive system - the pharynx.
Pharynx
The pharynx is part of the throat. It’s the muscular tube that connects the nasal and oral cavities (e.g. mouth) to the larynx (voice box) and oesophagus (eating tube). After food is chewed and formed into a bolus (a blob of chewed food) in the mouth, the muscles of the pharynx contract to initiate swallowing.
Oesophagus
Connected to the pharynx, the oesophagus is a muscular tube that extends down to the stomach. It moves food from the pharynx to the stomach through rhythmic contraction of the muscle walls called peristalsis.
There are two circular muscles in the oesophagus called sphincters, creatively named the upper oesophageal sphincter and the lower oesophageal sphincter.
The upper oesophageal sphincter
- Located near the point where the oesophagus meets the pharynx.
- Contracts to create a barrier between the pharynx and the oesophagus.
- Prevents entry of air into the oesophagus when breathing.
The lower oesophageal sphincter
- Located at the lower end of the oesophagus, near its junction with the stomach.
- Contracts to create a barrier between the oesophagus and the stomach.
- Prevents the backflow of the acidic stomach contents into the oesophagus.
Disorders and treatments
You will learn about common oesophageal disorders and treatments in this week’s SDL…
Self-directed learning activities
activity 1 - Nervous system
To summarise your learning on the nervous system, watch this video presented by Hank Green. This video will be helpful for the learning you will be doing in the next session of Anatomy and Physiology. You may like to take notes as you watch.
The video covers the following:
- Sensory input
- Integration
- Motor output
- Organisation of the central and peripheral nervous systems
- Glial cells
- Neuron types and their structure and function.
Watch: The Nervous System, Part 1: Crash Course Anatomy & Physiology #8 (10:35 minutes)
Level-up activity:
To illustrate how sensory input, integration, and motor output functions work, Hank uses an example of a spider walking on someone’s skin. Level up your learning and challenge yourself to think of another example that demonstrates these three primary functions.
Activity 2 - Digestive system
As we cruelly left you with a cliffhanger for the treatments of oesophageal disorders, continue your learning with this task.
A disorder of the oesophagus you will be very familiar with is heartburn (acid reflux). However, heartburn is often discussed interchangeably with indigestion (dyspepsia).
To refresh and consolidate your knowledge about these disorders:
- Read this article on indigestion and heartburn: The Difference Between Heartburn and Indigestion.
- Make notes on their symptoms, causes, treatments and why they are often discussed interchangeably.
- Save your notes to an easy-to-find location on your device for future reference.
That’s the end of another week of Patient Care 2!
He pai aū mahi i tēnei rā, you have done a great job, and once again, there has been a lot to learn.
Kia ora, welcome back to our journey through the cardiovascular system and medications for related disorders.
Hypertension review
Last week, we looked at hypertension and antihypertensive medication groups. In particular, you investigated Enalapril, an ACE inhibitor. If you feel like you have a solid grasp on this, continue to the next paragraph to get straight into this week’s content.
Otherwise, if you want to get your mind back in the zone and refresh your learning of angiotensin-converting enzyme action, re-read the online learning section on hypertension and rewatch this video from last week. Watch: How do ACE inhibitors work? (2:11 minutes).
Hypertension medications
Now, let’s get straight into investigating other medications that are used in the treatment of hypertension. This week, we will cover:
- Angiotensin II Receptor Blockers (ARBs)
- Beta-blockers
- Diuretics
Angiotensin II Receptor Blockers (ARBs)
ARBs have a similar effect to ACE inhibitors and are used when ACE inhibitors are not an appropriate treatment. An example of an ARB is Losartan.
Action
ARBs work by preventing angiotensin II from binding to its receptors. By blocking the effects of angiotensin II, ARBs help relax blood vessels, decrease sodium and water retention, and ultimately lower blood pressure.
Treatment
CV disorders that ARBs may be used in the treatment of include:
- Hypertension
- Heart failure
- Diabetic kidney disease
- Myocardial infarction
Beta-blockers
As noted last week, beta-blockers are no longer used as first-line treatment for hypertension unless indicated for a specific clinical reason. An example of a beta blocker is Metoprolol CR.
Action
The name is a bit of a giveaway. Beta-blockers block beta receptors in the heart, which reduces the effects of adrenaline (epinephrine) and other stress hormones on the heart. This action reduces the impact of stress hormones like adrenaline (epinephrine) on the heart, leading to a decrease in heart rate, a reduction in the force of heart contractions, and a lowering of blood pressure.
Treatment
CV disorders that beta-blockers may be used in the treatment of include:
- Congestive heart failure
- Hypertension
- Arrhythmias
- After a myocardial infarction
- Management of angina
Journal post
ARBs and Beta-Blockers
You now have a basic understanding of how ARBs and beta-blockers work and what they’re typically used to treat. Undertake your own research now to build on this knowledge.
- Create a new journal post titled: ‘ARBs and Beta Blockers’.
- Answer the following questions. You can use the New Zealand Formulary (NZF), Healthify and any other reliable and current resources available to you to help you.
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
- Remember to check back on your post in the next week for any tutor feedback.
Questions
Losartan:
- What are the side effects?
- Are there medications or food that should be avoided while taking this medication?
Metoprolol CR:
- What does CR mean?
- What are the side effects?
- Are there medications or food that should be avoided while taking this medication?
Remember, the responses you post to your journal are valuable study notes for future reference. The more detailed your answers, the better the study notes for future you!
Diuretics
Diuretics are used to increase the excretion of water and electrolytes through the kidneys into the urine. Diuretics are mainly used to treat hypertension and oedema (build-up of fluid in the body) caused by heart failure (which will be discussed later in this session).
Types of diuretics
Different types of diuretics work in different ways. Read this table to see three different examples.
| Type | Action |
|---|---|
| Thiazide diuretics | They prevent sodium from being reabsorbed by the kidneys. As the sodium is excreted, it takes water along with it. |
| Loop diuretics | Loop diuretics act mainly on the part of the nephron known as the ascending Loop of Henle. A nephron is the part of the kidney that filters blood and produces urine. Loop diuretics increase the secretion of sodium, chloride and water. |
| Potassium-sparing diuretics | These act on the distal tubule of the nephron and have weaker diuretic and antihypertensive effects. They have the advantage of conserving potassium, which is an essential electrolyte in the body for homeostasis. |
Ready to add to your notes? Here’s another journal post activity to get you exploring another type of diuretic, furosemide.
Journal post
Diuretics
Furosemide is a commonly used diuretic. Once again, use the NZF, Healthify and any other resources available to you to complete this activity.
- Create a new journal post titled: ‘Diuretics.’
- Answer the following questions in your post. You can use the New Zealand Formulary, Healthify and any other reliable and current resources available to you to help you.
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
- Remember to check back on your post in the next week for any tutor feedback.
Questions
- What type of diuretic is furosemide?
- In your own words, describe the action of furosemide.
- What are OTC medications that should be avoided when taking furosemide?
- What are the potential side effects, and what can you do about them?
Ka pai, you’ve wrapped up your learning for hypertension. It’s time to look at these other CV disorders, their symptoms, related disorders and their treatments:
- Dyslipidaemia
- Hypercholesterolemia (Mate toto hinuhinu)
- Atherosclerosis
- Thrombosis and Embolism
- Ischemic Heart Disease (IHD)
- Angina Pectoris
- Myocardial Infarction (MI)
- Congestive Heart Failure
Me ruku ki te kaupapa, let’s dive in!
Dyslipidaemia
What do you think this disorder is? Try breaking down the word into parts to work out its meaning. Once you think you have it, click the (+) symbol to see the answer.
Dys-: A prefix from Greek meaning "bad," "difficult," or "abnormal."
-lipid-: Refers to fats or fat-like substances in the body, including cholesterol and triglycerides.
-aemia: A suffix meaning a condition of the blood.
So, if you put the words and their meanings together, dyslipidaemia effectively means abnormal amounts of lipids or lipoproteins in the blood.
Wondering what lipids and lipoproteins are? Read on…
Lipids
Lipids are a group of molecules that include fats, oils, phospholipids, and steroids that are produced in various tissues and organs throughout the body. They serve as energy storage molecules, form cellular membranes, and act as signalling molecules.
Common types of lipids include triglycerides (fats and oils), phospholipids, and cholesterol.
Lipoproteins
Lipoproteins are complex particles composed of lipids and proteins produced by the liver. They are responsible for transporting lipids in the bloodstream.
There are two major types:
- Low-Density Lipoprotein (LDL): Often called "bad cholesterol," LDL transports cholesterol from the liver to cells. Elevated LDL levels are associated with an increased risk of atherosclerosis.
- High-Density Lipoprotein (HDL): Known as "good cholesterol," HDL helps transport cholesterol away from cells to the liver for excretion. Higher levels of HDL are generally associated with a lower risk of cardiovascular diseases.
Dyslipidaemia is a disorder of the blood and the blood vessels throughout the body. It can lead to various CV disorders as well as disorders of other body systems, such as:
- Stroke
- Kidney disorders
- Vision issues
- Fertility issues
- Impaired wound healing
- Peripheral vascular conditions
Hypercholesterolemia (Mate toto hinuhinu)
Hypercholesterolemia is a form of dyslipidaemia. Based on its name, what do you think hypercholesterolemia means? Here’s a hint: Hyper-cholesterol-emia.
Think you have it? Answer the quiz question to check your understanding.
Pānui, read this webpage from the National Heart Foundation of New Zealand to learn more about hypercholesterolemia. High cholesterol: Symptoms, causes and treatment. Be sure also to watch the brief video demonstrating the accumulation of cholesterol within artery walls and the resulting consequences of this buildup.
Journal post
Causes of hypercholesterolemia
Hypercholesterolemia can result from both modifiable factors (aspects individuals can alter) and non-modifiable factors (aspects outside an individual's control). Use this journal post activity to examine these factors.
- Create a new journal post titled ‘Causes of hypercholesterolemia’.
- Create a list of modifiable factors and a list of non-modifiable factors that can lead to hypercholesterolemia. Like the previous journal post activities, use reliable and current resources available to you to help you.
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
- As your tutor will be reviewing your post, check back on your post in the next week for feedback.
Atherosclerosis
Atherosclerosis is a condition linked to hypercholesterolemia, characterised by the narrowing and hardening of arteries. Atherosclerosis occurs due to the accumulation of fatty deposits of cholesterol and other substances on the inner walls of arteries.
The disease process of atherosclerosis is broken down into three phases.
- Fatty streaks – damage to the artery's inner wall, often caused by factors like high blood pressure, smoking, or inflammation. The damaged artery wall attracts cholesterol and other substances, creating fatty streaks.
- Soft plaque – the fatty streaks develop into plaques, which cause thickening of the artery's middle layer. Over time the plaques grow, narrowing the artery and restricting blood flow.
- Hard plaque – in this phase, all three layers of the artery wall are affected. As the plaques change and harden, they can rupture. This can trigger blood clot formation at the site. If a blood clot becomes large enough, it can block the artery completely, leading to a sudden and severe reduction in blood flow.
This illustration shows (from top to bottom) these stages of plaque formation.
Thrombosis and embolism
When a blood clot (poketoto in te reo) forms within an artery, it is referred to as a thrombus. The term "thrombus" is commonly used to describe a stationary blood clot that forms within a blood vessel. In an artery, a thrombus can occur due to conditions such as atherosclerosis, inflammatory vessel conditions, irregular heart rhythms and blood disorders. When a thrombus detaches and travels in the bloodstream to another location, it is called an “embolism”. Both thrombus and embolism can cause complete blockage of the arteries of the heart and, therefore, can be fatal.
Thrombus and embolisms can also occur in veins.
- Thrombus in veins - also known as a Deep Vein Thrombosis (DVT). DVTs often occur in the deep veins of the legs.
- Embolism from veins - if a portion of a venous thrombus breaks loose and travels through the bloodstream, it is called a venous embolism. The most serious complication of venous embolism is when it travels to the lungs, causing a Pulmonary Embolism (PE).
Treatment of dyslipidaemia

The aims of the treatment of dyslipidaemia are to normalise blood lipid levels and reduce cardiovascular risk. This risk refers to the likelihood of developing serious and potentially life-threatening cardiovascular disorders. Dyslipidaemia treatment typically involves a combination of lifestyle adjustments and medication.
Treatment of dyslipidaemia may include the following medications.
Statins
This group of medicines are called ‘HMG-CoA Reductase Inhibitors’, more commonly known as ‘statins’. An example is simvastatin.
Action
Statins target a specific enzyme involved in cholesterol formation. Statins bind to this enzyme, inhibiting its activity and blocking the process of cholesterol formation in the liver. As a result, less cholesterol is produced, leading to reduced levels circulating in the blood. A decrease in cholesterol minimises the potential for forming plaques in the arteries.
Treatment
CV disorders that statins may be used in the treatment of:
- Atherosclerosis
- Hypercholesterolemia
Journal post
Statins
- Find out more about the use of statins in New Zealand.
- Read this Healthify webpage, Statins, and find out:
- What statins are used in New Zealand?
- Common side effects from statins.
- Medications or foods that interact with statins.
- Create a new journal post titled ‘Statins’ and post your findings.
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
- Your tutor may post feedback, so make sure to check back next week.
Other medicines used in the treatment of dyslipidaemia include the following. Select the (+) icon to read more about each medicine.
- They inhibit cholesterol absorption in the small intestine, reducing Low-Density Lipoprotein (LDL) cholesterol levels.
- An example is ezetimibe.
- Fibrates reduce the production of very low-density lipids in the liver (VLDL). VLDL carries cholesterol from the liver to the bloodstream. They also speed up the removal of cholesterol from the blood by increasing HDL.
- An example is bezafibrate.
- Again, the action of this medicine is in the name! Bile acid binding resins bind to bile acids, forming a complex that is excreted in the faeces. This leads to an increased demand for new bile acids. The liver responds by using cholesterol to make more bile acids. This results in a reduction of circulating cholesterol levels, particularly low-density lipoprotein.
- An example is cholestyramine.
Ischemic Heart Disease (IHD)
The word "ischemia" may be a medical term you are unfamiliar with. The prefix "isch" means 'holding back or restricting,' and as you may have observed, terms ending in "-emia" relate to the blood. Therefore, ischemia refers to a condition where blood flow is constrained.
As we have discussed, this constraint of blood flow in the coronary arteries occurs due to atherosclerosis. If left untreated, insufficient blood supply to heart muscle can damage tissue, disrupting the heart's ability to function. If the restricted blood supply persists or blood supply is blocked, it can lead to the death of the heart muscle, which has serious and life-threatening consequences. IHD is often referred to as coronary artery disease (CAD).
Conditions resulting from reduced or blocked blood flow to the heart muscle include angina pectoris and Myocardial Infarction (MI).
Angina pectoris
Angina is a symptom of IHD. Chest pain or discomfort occurs when the heart muscle doesn't get enough blood flow, usually during exercise or stress. It occurs when a coronary artery is partially blocked, reducing blood supply and oxygen to a part of the heart muscle.
It is a warning sign that the heart is not receiving enough oxygen and often resolves with rest or medications.
Myocardial Infarction (MI)
Myocardial Infarction, commonly known as a heart attack, is a severe form of IHD. It occurs when a coronary artery is completely blocked, leading to a lack of blood supply and oxygen to a part of the heart muscle. This can result in damage or death of the affected heart tissue.
Once the heart muscle is damaged or has died, the heart can no longer pump effectively. This can lead to a variety of CV disorders. An MI is not always relieved by rest or medications and can cause permanent damage to the heart.
The development of plaques inside a coronary artery results in tissue damage and death of the heart muscle.
Journal post
IHD
Wā rangahau, research time!
- Create a new journal post titled ‘IHD’ and carry out your own research to answer the following questions.
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
- Your tutor may post feedback, so make sure to check back next week.
Questions
- What are the signs and symptoms of an MI?
- What are the signs and symptoms of angina?
- What does stable angina mean?
- What does unstable angina mean?
- What is an angioplasty, and why is it performed?
- What lifestyle factors can lower the risk of IHD?
Treatment of angina pectoris
The treatment for angina pectoris aims to relieve symptoms, prevent or reduce the frequency of angina attacks, and lower the risk of more serious heart conditions. Treatments include lifestyle changes, medical procedures, management of underlying health conditions and medications.
Medications used in the treatment of angina include the following:
- Antiplatelets reduce the tendency of platelets to stick together and form blood clots. This makes it easier for blood to flow through narrowed arteries due to atherosclerotic plaques. Reducing blood clot formation decreases the risk of blood clots breaking off and causing more severe complications.
- Example: Aspirin
- CV disorders that antiplatelet medications may be used in the treatment of:
- Coronary artery disease
- Myocardial Infarction (MI) - immediate treatment and ongoing management after an (MI).
- Nitrates help dilate blood vessels, improving blood flow to the heart.
- An example is: Glyceryl trinitrate spray (GTN spray).
Journal post
Glyceryl trinitrate
Glyceryl trinitrate is an example of a nitrate treatment for angina pectoris.
- Use these resources to complete the following Documentation tool activity.
- NZF: Glyceryl trinitrate (systemic)
- Healthify: Glyceryl trinitrate spray
- Download and save the completed activity.
- Create a journal post titled ‘Glyceryl trinitrate’.
- Upload the completed activity to your journal post and publish your post to ‘All course users’ so your tutor can review your answers.
Other treatments
Other medications used to prevent angina are:
- Beta-blockers - reduce the work the heart has to do, so it needs less oxygen, and in this way, they prevent angina.
- Calcium channel blockers - when beta-blockers are not suitable.
- Isosorbide mononitrate - works by widening blood vessels, letting more blood and oxygen reach your heart, reducing strain on it and making it easier to pump blood.
Congestive Heart Failure (Manawa ngoikore)
Congestive Heart Failure (CHF) is a cardiovascular condition characterised by weakened pumping power of the heart. In CHF, blood circulation slows, leading to increased pressure in the heart. This impairs the heart's ability to supply oxygen and nutrients to the body. The heart chambers may adapt by stretching or thickening, initially aiding blood flow. However, over time, the heart muscle weakens, hindering efficient pumping. The kidneys may respond by retaining fluid and salt, causing congestion in various organs.
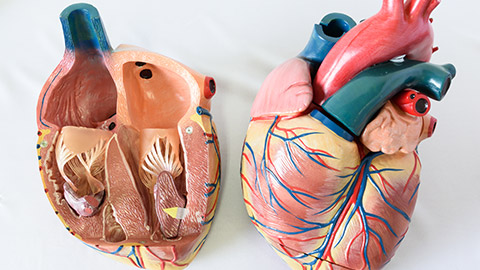
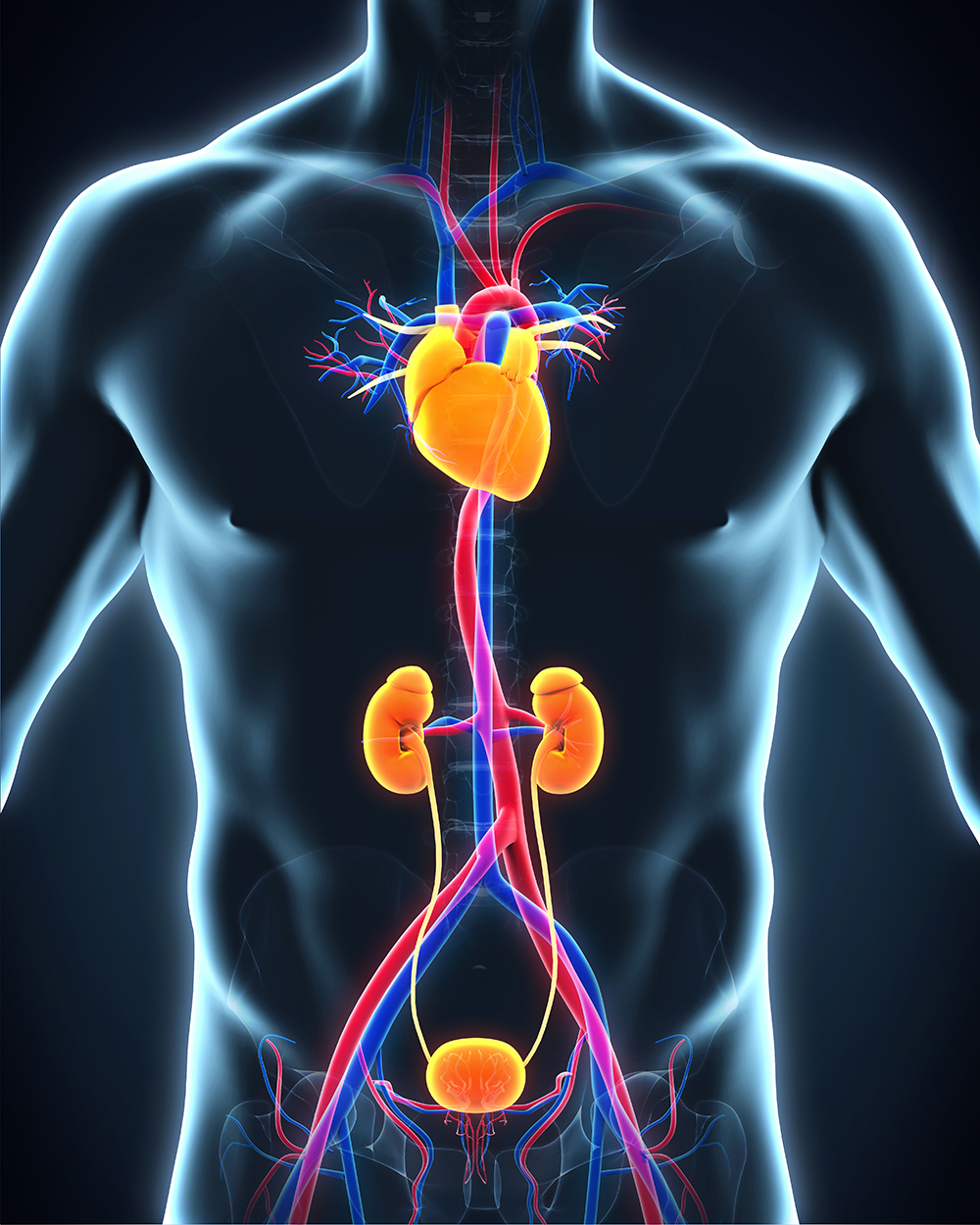
Here, you can see the effects of CHF on the heart chambers.
Watch: Congestive Heart Failure (2:48 minutes)
Transport yourself into the body and witness the anatomical changes that happen in left-sided heart failure and in right-sided heart failure. As you watch, pay special attention to any parts of the heart’s anatomy that you may have forgotten from last week.
Causes of CHF
CHF can be caused by various factors that affect the heart's ability to pump blood effectively. Common causes include:
- Coronary artery disease - where there is decreased blood flow to the heart muscle, therefore reduced oxygen and nutrients available.
- MI - where the heart muscle is damaged, resulting in a scarred area that does not function properly.
- Cardiomyopathy - damage to the heart muscle from causes other than artery or blood flow problems, such as from infections or alcohol or drug abuse.
- Conditions that overwork the heart - such as high blood pressure, valve disease, thyroid disease, kidney disease, diabetes, or congenital heart defects.
Treatment
Treatment of CHF includes self-care, surgery, and devices such as pacemakers and medicines.
Self-directed learning activity
Over the last couple of weeks, there has been a lot of new learning and many activities where you sought out information independently. This is a vital skill to have for your future work and to ensure that you’re a lifelong learner!
Therefore, your SDL this week is to revise your learning on the CV system from both Patient Care 2 and Anatomy and Physiology.
We suggest you focus on revising and organising your notes for the following:
- Anatomy and physiology of the CV system.
- Disorders of the CV system.
- Medicines used in the treatment of CV disorder and their:
- Action
- Side effects
- Food and medicine interactions
- Patient advice
If you find that you have unanswered questions or gaps in your knowledge, don’t be shy to do your own research (using reliable sources) or talk to your pharmacy colleagues.
He pukumahi koe! Pat yourself on the back for all your hard work - this has been a huge week of learning.
