Every child and adult who works in or uses your service has the right to feel safe and to have their health protected from work-related threats to health.
As we have seen, harm to health and well-being can take physical and psychological forms. It can result from exposure to work hazards such as contagious illnesses and infections, exposure to elements such as extreme heat and sun, vehicle accidents, trauma and stress.
This topic will take you through examples of specific controls that can be considered for different types of hazards and risks.
By the end of this topic, you will understand:
- Common legislation and strategies to ensure the health and wellbeing of children using the service
- Safe strategies for managing children's medical conditions
- How to prevent and respond to incidents and accidents
- How to follow emergency procedures
- Ways to manage safe drop-off and collection routines.
Infection Control Risks
In a children’s services environment, exposure to potentially infectious substances such as blood and other body fluids can put workers, other children and families at risk of many common and not-so-common infectious conditions and diseases. These can include infections such as colds, flu and gastro-enteritis; childhood diseases such as chicken pox and whooping cough; and more serious conditions such as hepatitis.
Body fluids such as urine, faeces, saliva, mucous, vomit and blood are the main methods by which viruses and disease-causing bacteria travel from one person to another.
The most effective and important infection control practices are:
- Regular washing of hands by both staff and children
- Cleaning all regularly touched surfaces multiple times a day; and having routines for daily, weekly and
- monthly cleaning and disinfection
- Being immunised from common infections and diseases
- Excluding staff and children when they are unwell.

Website
Division 2: Sections 85-89 of the Education and Care Services National Regulations outline the legal requirements for managing incidents, injury, trauma and illness.
Quality Area 2 of the NQS links with legislation requirements around infection control. Some of these requirements include:
| Problem or Hazard | Compulsory Control Measures |
|---|---|
| Contact with body fluids during nappy changing and toileting |
|
| Infectious illness |
|
| Food preparation and cleaning services |
|
Exclusion Periods
By law, your service must take reasonable steps to prevent the spreading of any known infectious disease at the service. This includes notifying a parent or authorised contact of any suspected or actual case of an infectious disease as soon as possible.
Exclusion periods apply to children and staff with particular infections to protect the health of others. Staying Healthy in Childcare (5th edition) helps ECEC workers to identify how long parents/guardians should be asked to keep children from the service, depending on the type of condition the child has.
Some common examples of exclusion periods include:
| Condition | Exclusion Period |
|---|---|
| Pertussis (whooping cough) | Children with pertussis should be excluded for 21 days from the onset of symptoms or until they have taken an appropriate antibiotic for at least 5 days. |
| Influenza (flu) | Children and adults with influenza should stay home until they feel well. |
| Conjunctivitis | Children with infectious conjunctivitis should be excluded until the discharge from the eyes has stopped. |
| Impetigo | Children with impetigo should be excluded until appropriate antibiotic treatment has commenced. Any sores on exposed skin should be covered with a watertight dressing. |
| Diarrhoea and gastroenteritis | Children with infectious diarrhoea should be excluded until the diarrhoea has stopped for at least 24 hours. |
| Hand, foot and mouth disease | Children with hand, foot and mouth disease should be excluded until all blisters have dried. |
Resource
You can find more details about exclusion periods on page 13 of Staying Healthy in Childcare (5th edition).
Education and Care Services National Regulations
Read the Education and Care Services National Regulations, Sections 85- 89, available online.
- What must happen if there is a suspected infectious disease at the service?
- What are the requirements for first aid kits?
Immunisation
Children should be immunised against conditions according to vaccination schedules, and your service needs to keep records of vaccinations.
Childhood vaccinations given at various ages from birth include:
- Hepatitis B
- Diphtheria
- Tetanus
- Pertussis
- Polio
- Haemophilus influenza
- Rotavirus
- Measles
- Mumps Rubella
- Varicella (chicken pox)
Website
The National Immunisation Program provides the National Immunisation schedule.
Environmental Risks to Health
Exposure to factors like smoke, poorly ventilated areas, fumes from cleaning products, potting mix used for gardening activities and many other inhaled hazards can accumulate over time, putting you at a higher level of risk than occasional exposure to toxins and irritants.
Chemicals such as cleaning solutions can be toxic if used in enclosed areas without adequate ventilation and harmful if mixed together. For small children, in particular, these inhaled irritants can contribute to conditions like asthma.
Your workplace must have policies regarding no smoking, no drugs and no alcohol, and these must be strictly enforced.
Where an environmental hazard has been identified, your service should use a systematic approach to assessing the risk and putting in place controls to reduce or eliminate it.
Sun Exposure Risks
Most Australians are aware of the risks of continued sun exposure over a person’s lifetime and how this exposure can contribute to skin cancer, even many years later. This hazard applies to children and educators, who often spend much time outdoors.
Children and adults should be reminded to wear a hat outside. Children should be familiar with the routine of applying sunscreen at least twice per day before going outdoors.
Child-friendly posters promoting sun-smart practices can be designed or printed from the internet and displayed near exits and outdoor areas.
Case Study
Liliane’s service has the following strategies in place to reduce the incidence of infection:
There are bright and colourful posters near the hand-washing basin to remind staff and children how to wash their hands. The posters include large photos of children washing their hands.
They encourage children to use disposable tissue and cough and sneeze into their elbows rather than onto their hands.
Photos of children engaged in the handwashing routine are also displayed.
Educators must wear gloves when undressing toddlers and then remove the gloves before re-dressing the children to avoid contaminating the clean clothing and nappies.
LEARN MORE
SunSmart has a range of excellent resources, including apps, sunscreen calculators, posters and widgets to help you and your service maintain safe shade and sun protection practices.
Practice
Exceeding the National Quality Standards
Watch the ACECQA Video ‘Exceeding the National Quality Standard Theme Guidance’.
What specific examples are given for health and safety risks?
Make sure that you keep notes for your future reference, as this information will support you in your assessment and professional practice.

In early childhood education and care settings, small injuries and accidents can happen regularly and are dealt with easily. However, there are also many hazards in this workplace setting that can potentially lead to moderate to severe injuries to children.
Example
Examples of injuries to children and babies can include:
- cuts and knocks from sharp edges on furniture or equipment
- trips and falls
- choking and strangulation from food, small objects, cords or equipment
- suffocation and cot death
- poisoning from chemicals, craft supplies or medications that are not stored correctly
- burns from boiling water, stoves or sharp utensils
- a child leaving the premises alone without the knowledge of staff
- vehicle accidents in parking and pick-up areas
- physical or sexual harm caused by visitors or intruders.
Maintaining a High Level of Physical Safety in the ECEC Environment
There must be a planned and systematic approach to safety in and around the centre. By law, a risk assessment must be completed for all indoor and outdoor areas, and daily safety checks must be done, using a hazard checklist made at the beginning of each day or before play (or both). Classrooms and play areas should be kept tidy and as free from hazards as possible.
Here are indoor and outdoor examples of safety checklists for indoor and outdoor play.
You must have specific practices to ensure safety during high-risk activities such as cooking and climbing equipment. Dangerous chemicals and products require storage in an area with a childproof lock. Power points must be protected, and curtain cords should never be accessible to children.
Record any hazards you cannot immediately rectify, such as in the maintenance book, and isolate them until maintenance is completed. It is important to talk with children regularly about safety.
The NQS also encourages educators to involve children in setting rules, such as setting rules for the number of children on a piece of play equipment, for example.
Think
Reflect on the following:
- What would safe practices look like for high-risk activities?
- How can you make cooking safer for children?
- How can you ensure safety for a child swinging on the top of an A-frame?
- How do you protect children from playing with water?
Watch
Watch the following video from ECA Learning Hub to find out more about how to involve children in safe risk-taking: ‘Learning to Take Risks’.
The Importance of Supervision
Supervision is the most effective way to reduce the incidence of accidental injury to children.
Some ways in which supervision is legislated include:
- The service layout and design must facilitate easy, constant supervision, with sightlines as clear as possible
- Minimum numbers of educators to child ratios, including how many educators present, must be early childhood teachers. These must be maintained at all times.

Adequate supervision is not just dependent on ratios, however. You must be able to notice and respond immediately to any incident or situation that could cause harm, even though you are also encouraged to actively engage with children rather than simply standing and watching them play. You must know where all children are at all times and give your complete focus to the children in your care.
To do this, you should be able to implement the four supervision points:
- Positioning—Position yourself at all times where you can see all children
- Scanning—Make use of peripheral vision when you are engaging with one child
- Knowing—Learning about your group of children will give you a better understating of their behaviour patterns and who may need higher levels of supervision.
- Listening—Pay attention to changes in children’s voices and respond immediately to differences in tone or volume.
Supervision Planning Considerations
Effective supervision planning is essential for ensuring the safety and well-being of children in early education and care settings. The following factors will be taken into account:
| Legal Compliance: Adherence to the National Law and Regulations is critical. This includes: |
Section 165: Ensuring adequate supervision of children at all times. |
| Age Group |
Consideration of children's supervision needs based on age is vital. Younger children typically require more supervision, while older children can have increased opportunities for agency. Supervision strategies will be tailored to the predictable behaviours, support needs, and capabilities of children at different stages of development, using knowledge of their play patterns to minimise risk. |
| Number of Children | The total number of children present in a given location will influence the supervision strategy, ensuring that all children can be adequately monitored. |
| Health and Known Conditions | Consideration will be given to any health issues or conditions that children may have, as these can impact their safety and supervision requirements. |
| Number and Positioning of Adults | Number and Positioning of Adults: The number of adults present and their strategic positioning throughout the environment will be planned to ensure that all areas are visible and accessible. |
| Areas | Educators will assess environmental factors, such as weather conditions, and plan the layout to facilitate constant supervision in both indoor and outdoor settings. Techniques such as scanning the environment and positioning themselves to maintain sightlines of all children will be implemented. Specific strategies will be in place to supervise children visiting restrooms in playground settings. |
| Activities | The nature of activities and their associated risks will be considered. High-risk activities, such as water play or construction projects, require closer supervision, while quieter activities, like drawing, may allow for more independence. Educators will monitor children closely during exploration and risk-taking and regularly check sleeping areas to ensure safety. |
| Context-Specific Needs | Depending on the specific location (such as during excursions, transporting babies, or engaging in bush kindy activities) and the nature of the activities, a higher educator-to-child ratio may be necessary to maintain safety. |
By carefully considering these factors in supervision planning, we can create a safe and supportive environment that promotes children's well-being and development.
Note
The National Regulations (Section 165) confirm that negligence in your role by not providing adequate supervision is a serious offence.
Website
The updated requirements for educator-to-child ratios in different services and based on the age of children can be found on the ACECQA website.
Case Study
Liliane supervises the children every day as they play outside. She notices that when children run behind a large piece of play equipment, they are hidden completely from her view. Liliane completed an incident form and raised the issue with her manager. A risk assessment is completed, and a maintenance request is carried out to have the structure safely moved to a different part of the outdoor area so that sightlines can be maintained at all times.Incident Report
Date of Report: 10.03.2024
Reported By: Liliane
Position: Supervisor
Location: Outdoor Play Area
Date of Incident: 10.03.2024
Time of Incident: 10:00 am
Description of Incident: During outdoor playtime, I observed that when children run behind a large piece of play equipment, they become completely hidden from my view. This situation poses a potential risk as I am unable to supervise the children effectively in that area.
Action Taken: I immediately noted the concern and completed this incident report.
I raised the issue with my manager for further assessment.
Witnesses:
Recommendations:
It is recommended that a risk assessment be conducted to evaluate the safety of the current placement of the play equipment.
Risk Assessment for outdoor area |
|
Assessment Date: 10.03.2024 Assessor: Liliane Location: Outdoor Play Area Activity: Supervised Play |
|
| Identified Hazard | Children running behind large play equipment, becoming hidden from the supervisor's view. |
| Risk Level | Likelihood: High Consequence: Moderate Overall Risk Rating: High |
| Existing Controls |
Supervisors are present to monitor children during playtime. |
| Recommended Actions: |
Relocate Play Equipment: Move the large piece of play equipment to a different area of the outdoor space to maintain clear sightlines. |
| Action Taken |
A maintenance request was submitted to relocate the equipment to ensure children's visibility at all times. |
| Follow-Up |
Confirm the completion of the maintenance request and review the play area after changes are made. |
Other supervision practices that will assist in ensuring safety are:
- Configuring children in groups that allow for maximum supervision
- Maintaining constant eye contact with the children, even if you need to talk to another adult
- Using teamwork and communication—Let other staff know in clear terms when you are taking a break or dealing with something important that interferes with your supervision duties.
- Regularly monitoring and checking cot rooms, including, but not relying on, the use of technology such as monitors.
Practice
Supervision Points
Consider the following space inside an ECEC facility used for children aged three to five by the Empowered Eductor4. Review the image and identify where you think the main supervision points should be if the children were spread evenly throughout the space.

Safe Sleep Practices
Your service must follow best practice principles and regulations regarding safe sleep, which are informed by current research.
When children are sleeping, an educator must physically check them every five minutes. This can include entering the sleeping room and ensuring the child is breathing. All cots, bedding and other equipment must meet Australian Safety Standards.
Your approach to safe sleep should be documented and shared with families.
Resource
See Little.ly Early Learning service Safe Sleeping Policy to read more details about safe sleeping practices.

Tips for the safe sleeping of babies:
DOs
- The cot meets Australian Standard AS2172
- The mattress is the correct size for the cot and is firm, clean, flat and not tilted or elevated
- The baby sleeps on its back
- The baby’s head and face are uncovered
- The baby’s feet are placed at the bottom of the cot
- Tuck blankets in firmly or use a safe baby sleeping bag
- Breastfeed baby
- Keep baby smoke-free
- Safe sleeping environment night and day
DON’Ts
- There are no pillows, doonas, soft toys, cot bumpers, or lambswools anywhere within the cot.
- The baby does not sleep on a water bed or beanbag
Reporting Incidents and Accidents
Incidents may involve anyone in the services, such as children, other staff, visitors and volunteers. Educators will ensure that they report incidents and accidents promptly. Incidents can include any event or near miss that has the potential to cause harm or causes harm to a child or adult. When a workplace incident or accident has occurred, educators will provide a verbal report to their supervisor where they accurately explain the details of what has occurred.
All incidents involving harm, injury or near-misses must also be recorded on your service’s internal reporting forms. This might be called an incident report or an incident, injury, trauma and illness record, such as the template provided to services by the ACECQA. The historical incident report, or an incident, injury, trauma and illness record, must be kept by the service until the child is 25.
The National Regulations require a detailed list of information to be collected whenever an incident or injury has occurred. If a child has been involved in any incident, injury, trauma or illness, you must notify the child’s parent/guardian/s as soon as possible but no later than 24 hours after the incident.
Incident Reporting Process
When reporting an incident, the policy outlines the following steps to ensure a thorough and effective response:
| Immediate Response | Ensure the safety of all individuals involved. Administer first aid or call for emergency assistance if needed. |
| Notify Supervisors | Inform your immediate supervisor or designated authority about the incident as soon as possible. Provide them with preliminary details about what occurred. |
| Document the Incident | Date, time, and location of the incident Names and contact information of those involved or witnesses A detailed description of the incident, including circumstances leading up to it and actions taken Any photographs or evidence related to the incident, if applicable Submit the Report: Send the completed incident report to the appropriate personnel, as specified in the policy. This may include a safety officer or management team. |
| Follow-Up Investigation | Be prepared to participate in a follow-up investigation. This may involve providing additional information or answering questions about the incident. |
| Review and Action Plan | Once the investigation is complete, the organisation will review the findings and implement any necessary actions to prevent similar incidents in the future. |
This process ensures that all incidents are properly documented and addressed, contributing to a safer environment for everyone.
Resource
You can download a PDF version of the Incident, injury, trauma and illness report by visiting the ACECQA site.
You can review the ACECQA Incident, injury, trauma and illness Policy Guidelines.
Resource
See the Little.ly Health and Safety policy HS19: Incident, Illness, Accident and Trauma for an example of a policy relating to this section.
Note
Serious incidents, accidents, and trauma must be reported to your state or territory regulatory authority within 24 hours.
These include:
- Incidents that require professional medical attention, such as from an ambulance, doctor or hospital, e.g. a severe asthma attack or a broken limb.
- Diagnosis of certain infectious diseases of a child or children in the service, such as whooping cough or an outbreak of gastroenteritis.
- The death of a child at the service or as a result of an incident at the service.
- A complaint alleging that children's safety, health or well-being has been compromised. For example, a child left the service unnoticed or a child locked in or out of the service (regardless of how quickly the situations were addressed)
- Any emergency that has required the police, ambulance or fire brigade.

Children with non-contagious medical conditions or disabilities have the same right to enjoy the full benefits of your service and to be included as much as possible in the same activities as other children. This might require you to pay particular attention to factors that might put the child at additional risk, but you must do so in the most inclusive and least restrictive way possible.
Example
Common medical conditions that might present themselves at your service include:
- Asthma
- Allergies, including severe anaphylactic reactions
- A health condition that requires regular or intermittent medication, such as diabetes.
General requirements under the Education and Care Services National Regulations for children with medical conditions include:
- At least one educator with a current approved Level 2 First Aid Qualification must always be on the premises.
- You should be aware of how children with medical conditions are managed.
- Anaphylaxis training and asthma management training should be provided regularly to all staff.
- First aid kits should be in a prominent place.
- First aid kit contents - there are requirements about what must and must not be contained in them, what they look like, how often they are checked and where they are positioned.
Risk Minimisation Plans (RMPs)
A risk minimisation plan can help you and other educators to allow the child the freedom to do as other children do while considering ways in which you can minimise risk to children with health needs. It should be developed in conjunction with the child’s parent/guardian/s and includes a risk assessment to determine:
- The particular risks that apply to this child and an assessment of the risks.
- Strategies to reduce the risk to the child.
- An assessment of the practices used in the service against the child's needs. Such as food preparation, handling practices, and ways to ensure that the child always has medication available at the service.
Medical Management Plans (MMPs)
A medical management plan (MMP) should be completed for a child with a medical condition or health care need in conjunction with or supplied by the child’s parent/guardian/s. The MMP outlines how staff should respond when a child has an episode or incident of a known health condition, including asthma, allergies and diabetes.
You must be familiar with each child’s medical management plan, where it is kept, and the location of the medication. New or casual staff must also know the children's identity with MMPs and can easily identify them.
Your service must have a process for updating the plan as soon as possible whenever the child’s parent/ guardian/s communicates a change in the plan.
A copy of your service’s medical conditions policy must also be provided to the parent/guardian/s of children with a specific health care need, allergy or other medical condition.
Resource
Go to the ASCIA website to review downloadable first aid and action plans for a range of medical conditions and treatments, including:
- Allergic reactions
- Anaphylaxis
Administering Medication
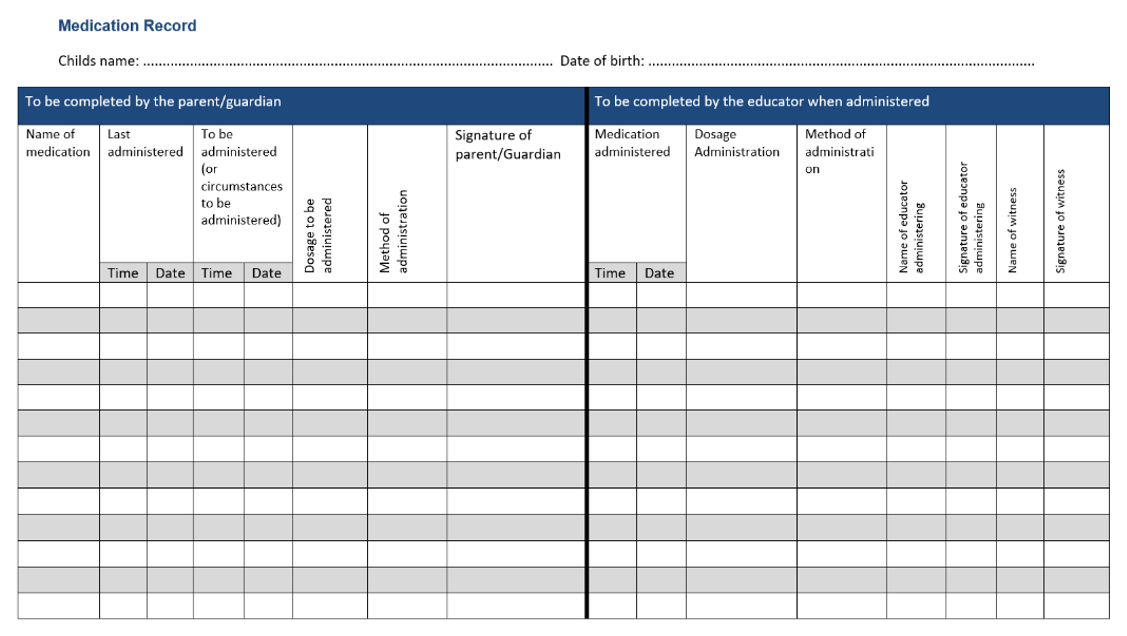
Medication must only be administered when there is a medication record in place, and it must include the details of each medication the child receives.
Medication records must include:
- The child’s name
- An authorisation for you to administer the medication signed by the parent or authorised person
- The name, dose and route of the medication to be administered
- The time and date the medication was last administered and when it should be administered next
- A place for qualified staff to record the above details when you have given medication and include the time, date and their name and signature.
Some policies will require two staff members to check the medication, and the medication chart will include these details. The medication record must then be stored at the service to maintain compliance.
Here is the ACECQA Medication Record Template5:
Note
Suppose there is an emergency and the child is not authorised to be given medication. In that case, there is an allowance in the regulations for authorisation to be given verbally (such as over the phone) by a parent or person authorised on the child’s enrolment form, a doctor, or an emergency services officer.
Parents or guardians authorise staff to administer emergency medication such as an EpiPen in the child’s enrolment form. However, in the case of an anaphylaxis or asthma emergency, medication such as a Ventolin inhaler or EpiPen may be administered to the child without authorisation. In this situation, an ambulance and the child’s parent or guardian must be notified as soon as possible.
Resource
Refer to the Little.ly Early Learning Administration of Medication Policy for more details.
Website
Allergy and Anaphylaxis Australia provide resources to help your service identify and manage children with allergies.
Self-Administration of Medication
You must have a written authorisation for a child to self-administer their own medication in your service. Only children over pre-school age may self-administer medications, and there must be clear policies around this procedure if it takes place in a service such as an Outside School Hours Service.
An example of this may be medication for Asthma or Diabetes.
Medical Emergencies
When alerted to a medical emergency in which CPR might be required, educators should follow the DRSABC response:
| DRSABC | Action |
|---|---|
| Danger | Check for danger to yourself and then others, such as where the emergency is the result of an accident inside the facility. |
| Remove | If safe, remove any hazards that might have caused the emergency, such as a weapon, faulty electrical equipment, an attacking dog or a chemical spill. |
| Response | Check for a response from the person or child by tapping them, calling their name, and asking, ‘Are you okay?’ |
| Send for Help | Stay with the person or child, and attract another person’s attention, asking them to call for an ambulance. State the nature of the medical emergency and the exact location of the victim. |
| Airway | Check that the airway is clear |
| Breathing | Check for normal breathing |
| Compressions | If the person is not breathing, commence chest compressions |
Resource
See the Little.ly Health and Safety policy HS10: Administration of First Aid for an example of a policy relating to medical emergencies.
Practice
How to Give an EpiPen
Watch this video from Allergy and Anaphylaxis Australia and consider the following questions:
- What are the risks involved in administering an EpiPen?
- What effect does adrenaline have on anaphylaxis?
- What are the procedures for administration?
Make sure that you keep notes for your future reference, as this information will support you in your assessment and professional practice.

Emergencies can take several forms, and you and other educators must be trained to manage them using emergency procedures, remaining calm and keeping in mind the welfare of the children and others around you.
Example
Emergencies can include:
- Internal emergencies, such as gas leaks, partial building collapse, fire or flood
- Natural disasters, such as bushfires, earthquakes, floods or major storms
- Aggression and violent threats, such as from an intruder or known offender
- Bomb threats over the phone
An Emergency Management Plan (EMP) is a detailed plan outlining how to respond during an emergency or potential emergency. It should be created with local emergency professionals, government departments and other services. The EMP aims to keep staff, children and visitors safe. It also helps ensure that continuing quality care can be provided to children. It includes diagrams such as the locations of emergency exits and the chain of command that applies in an emergency.
EMPs must be regularly reviewed and practised using drills, including with children, to ensure that they understand the need and reason for practice. Records of emergency drills and evaluations of these drills must also be kept.
A copy of the emergency and evacuation floor plan and instructions must also be displayed prominently near each exit at the service.
It is your service's legal responsibility to ensure that educators have easy access to emergency equipment, such as fire extinguishers and fire blankets, and know how to use them. Records must be kept that emergency equipment is tested as the manufacturer recommends.
Emergency procedures and emergency telephone numbers should be displayed in a place where they can be easily seen. Relief educators should also be inducted into emergency plans and exits as part of their introduction to the service.
Familiarise yourself with emergency response procedures and evacuation assembly points for your work area. Know where equipment such as duress alarms and evacuation kits are kept, and be familiar with how they work. The service should also communicate to families about the service’s emergency plans and how incidents are managed.
During and after any emergency, your main priorities should be as follows:
- If you feel a situation is threatening or out of your control, never hesitate to call or ask another person to call 000. If the situation improves soon after, you can cancel the service.
- Stay calm. If you talk and think calmly, you are more likely to be in control of a positive outcome.
- Continue to provide care and support to children.
- Do not take risks with your own life or safety to protect others. If you are in a personal risk situation, get yourself to safety before calling for help.
Note
Training in emergency responses and the use of emergency equipment must occur at least annually, with records of staff attendance and participation. This training should include educators, coordinators, FDC educator assistants and other staff.
Resource
Sections 97 and 98 of the Education and Care Services National Regulations outline the legal requirements for emergencies and communication that must be maintained during an emergency.
Evacuation
Depending on the type of emergency, an evacuation may be:
| Type of Evacuation | Example |
|---|---|
| Partial | This might involve evacuating from a lower to a higher floor or moving staff and children from a room or area through fire or smoke doors. |
| Progressive | Several stages of evacuation might occur as the hazard—such as fire or a violent intruder—draws nearer when it is considered unsafe to leave, for example, to the next safe area and then on to the next safe area through the building. |
| Full | Evacuation to the outdoor area or into another safer building or location. |
Evacuation Procedures
Most evacuations must follow a procedure similar to the following:
- An alarm will sound, or you will be alerted to an emergency by other staff
- Staff member/s will calmly move children to line up at the exit door of the room and complete a head check
- The room leader will collect sign-in sheets and medications and do a final check of the room
- At the exit door, staff will do a head count of children and staff and ask walking children to hold the evacuation rings in a straight line
- Babies will be placed in an evacuation cot if possible
- Staff and children will exit to the assembly point (often the car park or an empty piece of land)
- As they walk out the door, staff will collect the emergency evacuation bag that holds parent/ guardian contacts, first aid kit and other survival items
- Once they have arrived safely, staff will do another head check of staff and children
- When safe, return to the room. If it continues to be unsafe, call parent/s or guardian/s to collect the children.
An evacuation should involve a designated staff member/s checking each area or room, including toilets for children or adults, and completing counts at each stage of evacuation.
Good record-keeping can help keep all children and adults safe and comply with legal and accreditation requirements. You must keep excellent records of children’s attendance each day, and a senior worker collects this during an evacuation so that emergency services workers can easily see who is present in the service during an emergency.
A senior educator should also carry a current hard copy record of children’s emergency contacts in case of emergencies and evacuations. Emergency bags should also be kept in all rooms where children might be cared for during an evacuation. These should include first aid kits, contact details of families, lists of the children who use or sleep in each room, evacuation rope and a copy of each child’s medical plans.
Natural Disasters
Natural disasters are weather or environmental events that can significantly impact the safety and well-being of staff and children in an ECEC. While these events are relatively rare, some areas of Australia are at higher risk than others for disasters such as floods, fire, earthquakes and major storms. Even if you do not live in a high-risk area, natural disasters can still threaten many areas of Australia.
Pay attention to official warnings such as bush fire alerts, particularly if you work in a rural, semi-rural or remote facility. Families should be notified to keep children at home when a natural disaster threatens their area. The EMP will include details about how your service will respond.
Internal Fire
If you notice a fire, such as on a stovetop or piece of electrical equipment, your first response should be to call for help to assist children in evacuating from the area or the building. The fire department should be notified immediately on 000. If it is safe to try and fight the fire while other staff assist with removing children from harm, turn off any possible ignition sources, such as the gas on the stove. If possible, ask someone else to shut down air-conditioning to prevent the spread of gas or flames.
Follow the instructions of area wardens, chief wardens or emergency services officers if an evacuation has been called and evacuate children calmly to a safe area. Remain at the assembly area until emergency services officers further advise you.
Example
Your Emergency Management Plan will include:
- The decisions that might trigger the need to evacuate, partially evacuate or shelter in place.
- The contents of emergency evacuation kits.
- The roles of different staff members.
- How will liaisons with emergency services take place?
- How will children continue being provided safe care during and after the emergency?
Bomb Threats
Bomb threats in children’s services are rare but should always be taken seriously.
A bomb threat might be received in writing or via phone. Police must be notified immediately when any such threat is made. If you receive a bomb threat by phone, stay calm and keep the caller on the phone for as long as possible. Do not hang up until police arrive, even after the caller has hung up.
In the meantime, try to attract the attention of other staff members, silently asking or writing down for them to contact the police on 000. If you have one available, complete a bomb threat checklist. This will help you to ask questions recommended by the police.
Example
Ask questions and record the responses, along with any accent, gender, approximate age, tone of voice and background noise.
Questions you might ask include:
- What type of bomb is it?
- Where is it?
- When will it explode?
- What does it look like?
Violence or Aggression, Including Armed Aggression
You might be faced with a threatening situation as a result of:
- a family member using aggression or violence towards you or other staff
- a suspicious person lurking near the service
- a known or unknown, armed or unarmed person that makes or acts on threats of violence.
A lockdown may be ordered by police or an emergency warden, especially if the intruder is not inside the service.
You may be given instructions to:
- Lock all doors and close all blinds
- Collect the emergency bag and attendance list if it is safe to do so
- Collect all children and babies in emergency cots, accounting for each child or baby, taking them to an area in the centre of the building, away from windows and exits
- Stay on the phone with the police.
- Remain with children and keep them calm until the police have given you the all-clear.
Passive self-defence is a strategy that aims to allow you to leave an aggressive situation safely when you are trapped in a room or space where an aggressive person is making threats or making you feel frightened. This is so that you or others can help children and staff to safety. You should:
- Agree with the person rather than arguing. Agreeing, even with untrue statements, can help to deescalate the person’s aggression long enough for you to get help. Divert blame is directed at you and sent to a safer source.
- Use passive body language. Minimise your body movements and use a low, calm voice. Make yourself appear smaller and unthreatening by lowering your shoulders and avoiding prolonged or insistent eye contact.
- Keep a distance between you and the person by moving away from them and towards a safer area, such as a door, if possible. Do not try to approach the person or touch them to calm them.
- Use objects to protect yourself. Use items such as chairs, tables or other items you can pick up. Protect yourself from harm with the item in your grasp while you attempt to leave so that you can call for help.
If you are involved in an armed threat:
- Remain calm and respond politely and quietly to the armed person. Obey orders such as handing over valuables without question if the demands are not dangerous to you or others.
- Use a duress alarm, call bell, mobile phone or internal communications only if it does not put you or others in more danger.
- Remove yourself from the situation as soon as it is safe to leave, and alert others to call 000 and ask for the police. All staff not directly affected should follow instructions to stay quiet and safe and to protect children in an area based on instructions from the police.
- Try to take note of as many physical details about the person as possible.
- Staff should not follow the offender if they leave the service. Instead, inform police of the person’s details and information about their mode and direction of departure.
Debriefing After an Emergency

A debriefing session following a major incident can help all staff talk through their emotions and practical coping strategies and discuss what could have been done differently in a non-threatening and no-blame environment. An Employee Assistance Program should also be utilised to help with individual counselling.
Resource
See the Little.ly Health and Safety policy HS5: Emergency Management for an example of an emergency policy.
Case Study
Liliane is being threatened by the father of a six-year-old child at the doorway of the service. Liliane has become aware of a court order that prevents the father from having unsupervised access to the child, but he demands that his son be brought out to see him. The father is aggressive and abuses her with names and insults. He tells her that the government is out to get him and doing whatever it can to cause him to break.
Liliane remains calm. She tells the father that she is sorry that the government are doing this to him. She asks if she can make a call, but he realises that she wants to call the police and refuses to allow her to move, cornering her and demanding to see his son. Liliane nods and agrees with the man. ‘I’m so sorry that you are in this situation,’ she tells him, still cornered.
One of the other educators, Paula, notices the man yelling at Liliane. She alerts the other staff, and together, they evacuate the children into a safe back room, locking the door while Paula calls the police.
Police arrive a few minutes later, and the man is arrested. Liliane is shaken but relieved. The workers are involved in a debrief a few days later and talk about how the incident played out, including how additional policies and equipment could help. A duress alarm is provided to every staff member a few weeks later, which provides them with added reassurance.
Practice
Emergency Management Plans
Obtain a copy of the Emergency Management Plan from your workplace or placement organisation.
What are the specific requirements outlined in the plan for responding to:
- A fire emergency?
- Aggression?
Make sure that you keep notes for your future reference, as this information will support you in your assessment and professional practice.

Several factors create risks at the time of drop-off and collection. These include:
- Risk of injury to children near cars in car parks and adjacent roads, particularly when many parents/guardians are arriving and leaving at the same time
- Problems with the supervision of children if staff are being distracted by questions from parents/guardians or carers
- The risk of children being picked up by an authorised or unknown person, particularly during child custody disputes.
Resource
Section 99 of the Education and Care Services National Regulations outlines the legal requirements for children leaving the premises.
Policies Relating to the Collection of Children
Your service must have a policy that is provided to families about the need to update authorised permissions for pick-up children. In all states and territories except Western Australia, the following rules apply to the pick-up and collection of children.
The child may only leave the premises:
- with a parent/guardian who is not prohibited by a court order from having contact with the child
- with a nominee authorised (such as by the parent) and named in the enrolment record
- if the child requires medical, hospital or ambulance care or treatment or because of another emergency
- when taken on an excursion with the written authorisation of the parent/guardian.
Protecting Children From Harm From Visitors or Intruders
You have a duty of care to ensure that no visitors, including contractors, are left alone with a child or children for any period. Entrances must be secure, and all visitors are required to sign in and out.
You must supervise every person who enters and leaves the service in areas where children are present.
Maintaining Supervision During Pick-Up and Collection Times
Monitor children’s arrival and departure carefully, and plan rosters and tasks to ensure you can maintain visual contact with all children. Avoid lengthy conversations with parents/guardians and carers while you are supervising. Instead, make time to speak to them when you can give them your attention and focus.
Example
Families should be informed of the importance of road safety, speed and parking during drop-off and pick-up. Remind each child to hold their parent’s or carer’s hand while leaving.
Where street parking allows parents/guardians to obstruct the sightlines of other drivers, who may not see a child running from behind a car, local councils can help with planning and implementing parking restrictions and fines to improve traffic safety.
